Translate this page into:
Magnetic resonance imaging in arthropathies of elbow joint: A pictorial review

*Corresponding author: Madhurima Sharma, Department of Radiodiagnosis, Post Graduate Institute of Medical Education and Research, Chandigarh, India. madhurimashrm88@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma M, Soundararajan R, Verma N, Sinha A, Chouhan DK, Prakash M. Magnetic resonance imaging in arthropathies of elbow joint: A pictorial review. Indian J Musculoskelet Radiol. doi: 10.25259/IJMSR_49_2024
Abstract
A wide variety of degenerative, inflammatory, and infective arthropathies can involve the elbow joint. These conditions usually present with overlapping clinical signs and symptoms thereby posing a diagnostic dilemma. Due to its excellent soft-tissue contrast resolution and multiplanar capability, magnetic resonance imaging (MRI) has made a significant contribution in the early and accurate diagnosis of various arthropathies. In this article, we have provided a brief review of common and uncommon MRI features of various arthropathies involving the elbow joint.
Keywords
Arthropathy
Elbow joint
Magnetic resonance imaging
Osteoarthritis
Rheumatoid arthritis
Septic arthritis
INTRODUCTION
The elbow is a complex joint due to its highly improved bony architecture and comprises three articulations: Ulnohumeral, radiocapitellar, and radioulnar joints. The complex bony anatomy of the elbow joint makes its imaging challenging. Conventional radiography is usually the first radiological investigation performed for the elbow joint. The standard radiographic examination comprises two views in orthogonal plane: Anteroposterior and lateral view. While conventional radiography is cheap and easily available, it is limited by its ability to pick early changes in various pathologies, suboptimal soft-tissue evaluation, and two-dimensional assessment of the joint. Computed tomography (CT) is an excellent cross- sectional imaging modality for the evaluation of bony structures. 3D reconstructed CT images are particularly useful for pre-operative planning. However, due to suboptimal soft-tissue contrast, the role of CT is limited in the evaluation of soft-tissue structures. Ultrasonography (USG) is an easily available, nonionizing imaging modality for the evaluation of soft-tissue structures around the elbow joint. Joint effusions, synovial thickening, fluid in bursae, tendon sheaths, and bony erosions can be detected on sonography. Doppler USG can be used to demonstrate hyperemia within the synovial tissue thereby indicating an active inflammatory process. In addition, USG can also be used to guide various diagnostic aspirations and interventional procedures. However, sonographic evaluation is often limited by operator expertise, patient habitus, and suboptimal evaluation of bony structures. Due to its multiplanar capability and excellent soft-tissue resolution, magnetic resonance imaging (MRI) has emerged as a powerful tool for the assessment of elbow joint.
MRI of the elbow joint is performed using a surface coil in a high-field strength magnet. T1, T2, and proton density sequences are acquired with and without fat suppression. Gradient echo images are particularly useful for the evaluation of loose bodies, tenosynovial giant cell tumor (TGCT), and hemophilic arthropathy. Post-contrast images after administration of gadolinium-based contrast are useful in cases with suspicion of synovitis, infective, or inflammatory arthropathy. Various arthropathies affecting the elbow joint are not specific to this joint. MRI is helpful in differentiating among the various common and uncommon disease processes involving the elbow joint. The presence of synovial proliferation, erosions, marrow changes, adjacent collections, intra-articular bodies, and magnetic susceptibility artifacts can help narrow the differential diagnosis of various arthropathies involving the elbow joint. In this article, we have demonstrated MRI features of various arthropathies involving the elbow joint.
DISCUSSION
Osteoarthritis
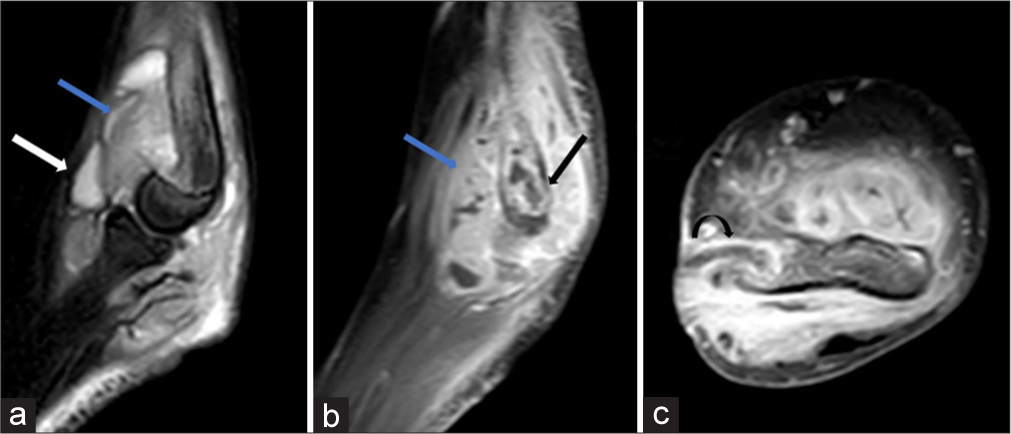
Primary osteoarthritis of the elbow is common and is frequently seen in manual laborers or patients engaging in heavy sports. It typically involves the ulnohumeral joint of the dominant extremity.[1] Bilateral involvement can be seen in 25–60% of cases.[2] Early osteoarthritic changes can be seen in patients with past history of trauma, infection, or inflammatory process. In the early stage, patients present with pain at terminal flexion and extension, due to olecranon and coronoid osteophytes engaging their fossae. With disease progression, pain is encountered during the whole range of motion.[1] Radiographs show osteophytes along the anterior margin of coronoid, the posterior margin of olecranon, the radial head, and the distal end of humerus. Loose bodies are not infrequently seen. Radiocapitellar joint space narrowing can also be seen. However, ulnohumeral joint space narrowing is seen in advanced osteoarthritis. MRI is particularly useful in demonstrating the articular cartilage. Deep fissuring of articular cartilage or full-thickness cartilage loss can be seen with abnormalities in the underlying bone. Bony osteophytes, loose bodies, and subchondral cysts are other associated findings[2] [Figures 1 and 2]. In throwing athletes, cartilage changes involve the posterolateral aspect of trochlear notch. In elderly patients, cartilage loss is more common in radiohumeral articulation.[3]

- (a) Coronal T1 weighted (b) sagittal T1 weighted and (c) coronal T2 fat saturated MRI images in a case of primary osteoarthritis show degenerative changes in form of bony osteophytes involving coronoid process (white arrow in b) and medial humeral epicondyle (white arrow in a) with cartilage loss (black arrow in c) and a loose body superior to coronoid process (blue arrow in b). Mild joint effusion was also present.
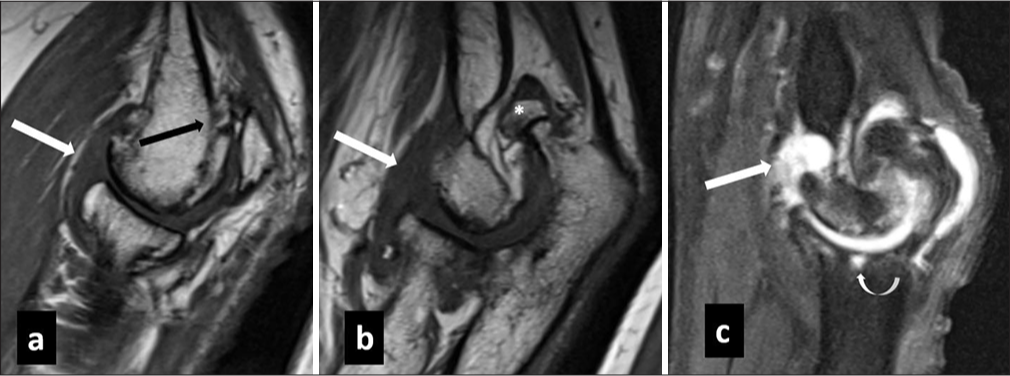
- (a,b) Sagittal T1 weighted and sagittal (c) T2 weighted fat saturated images in a case of post infective osteoarthritis show degenerative changes in radiocapitellar and ulnohumeral joints in form of extensive bony osteophytes (black arrow in a), cartilage loss, subchondral cysts (curved white arrow in c) and loose body (* in b). Also note presence of mild joint effusion (white arrow in a-c).
Rheumatoid arthritis (RA)
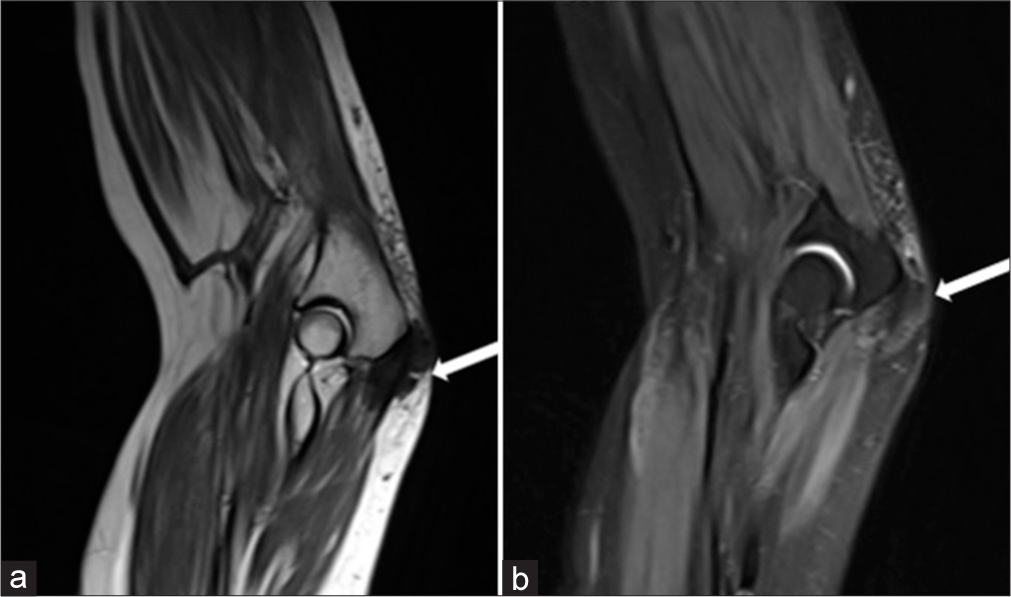
Elbow involvement has been reported in 20–50% of cases of RA, usually presenting within 5 years of the diagnosis.[2] Key MRI findings include synovial thickening and effusion, with post-contrast synovial enhancement in active phase [Figure 3]. Bone marrow edema, bony erosions, and periarticular contrast enhancement are the other common MRI findings in RA. In addition, dynamic contrast-enhanced MRI has been shown to differentiate active from inactive RA. MRI is the most sensitive modality to detect early RA changes with erosive bony changes being more specific for RA than synovitis.[4] Gradual destruction of articular cartilage leads to joint space narrowing. Intraosseous synovial cysts may be seen which occur away from the load-bearing areas (unlike osteoarthritis). Rarely inflammed synovium may herniate into periarticular soft tissue leading to compression of adjacent neurovascular bundle.[5] Erosion and deformity of the distal humerus, radial head, and coronoid process are the typical findings. Associated extra-articular findings such as olecranon bursitis, tenosynovitis, and rheumatoid nodules over the extensor aspect are also well depicted on MRI.
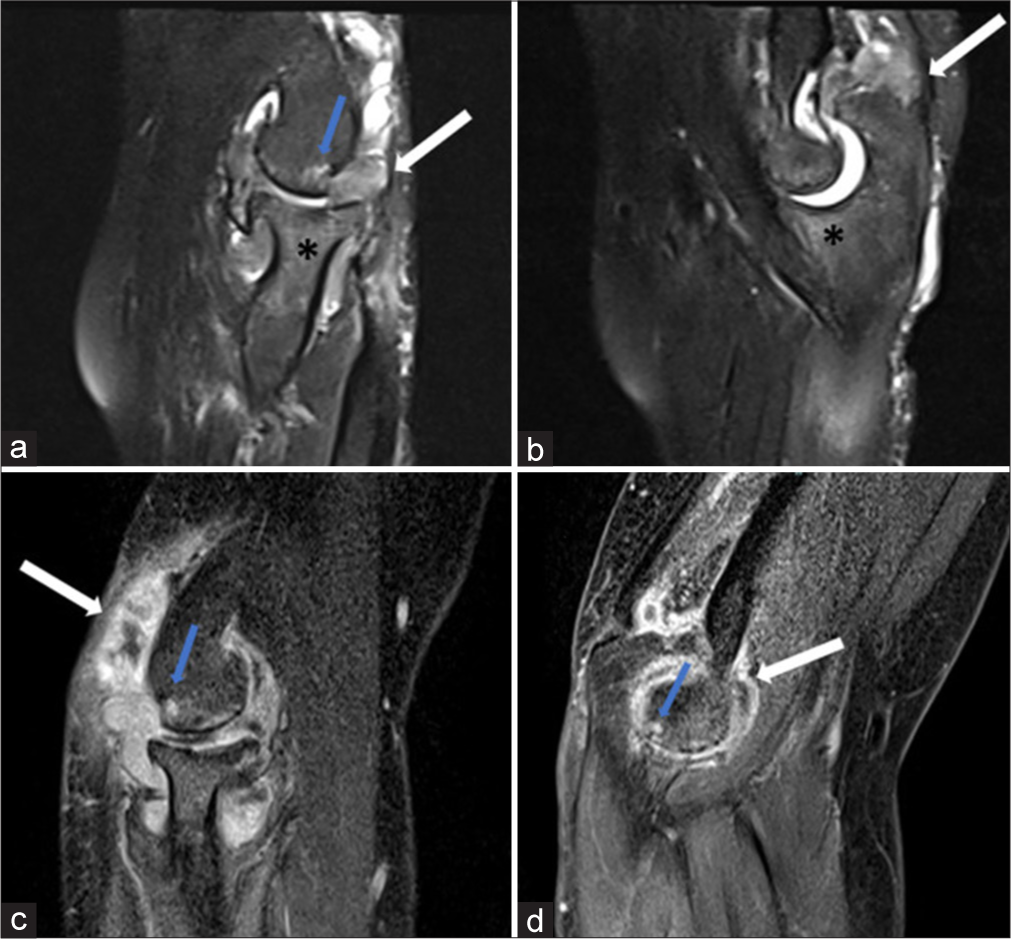
- (a,b) Sagittal proton density fat saturated images and (c,d) sagittal post contrast T1 weighted images at the level of radiocapitellar and ulnotrochlear joint in a case of rheumatoid arthritis reveal joint effusion with synovial thickening and proliferation with post contrast enhancement (white arrow in a-d) suggestive of synovitis. Associated bony erosions (blue arrow in a,c,d) and bone marrow edema (* in a and b) were also seen.
Septic arthritis
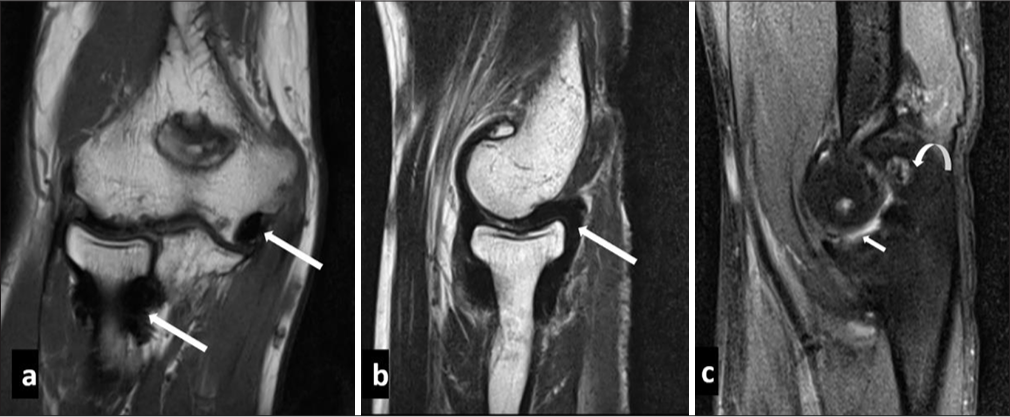
Involvement of the elbow can be seen in approximately 3–13% of all cases,[6] with more common involvement in pediatric and immunocompromised population. Infection may spread through hematogenous route, contiguous spread, or direct implantation. Timely diagnosis of septic arthritis is crucial to prevent bony destruction and osteomyelitis. However, imaging findings of septic arthritis usually overlap with inflammatory arthritis. A combination of bone erosion with marrow edema is suggestive of septic arthritis over inflammatory arthritis.[7] Associated perisynovial edema, soft-tissue edema, and marrow enhancement increase the diagnostic confidence for septic arthritis [Figures 4 and 5]. However, no single MRI feature can clearly differentiate infective from non-infective arthritis and joint aspiration can be necessary to rule out infection. The presence of a T1 hyperintense rim of granulation tissue in an intra-osseous collection can help in differentiating osteomyelitis from other non-infective etiologies.
- (a,b) Sagittal proton density fat saturated images and (c,d) sagittal post contrast T1 weighted images in a case of septic arthritis reveal joint effusion with synovial thickening and enhancement (white arrow a and c) with large bony erosions (blue arrow in a,b and d) showing peripheral irregular enhancement and marrow edema (* a,b and d). Also note associated perisynovial soft tissue edema.
- (a) Coronal T2 weighted fat saturated and (b,c) post contrast coronal and axial fat saturated images in a case of septic arthritis reveal ulnohumeral joint space narrowing with synovial thickening and enhancement (white arrow in a,b and c), associated erosions (blue arrow), marrow edema (black arrow in c) and adjacent soft tissue edema (* in c).
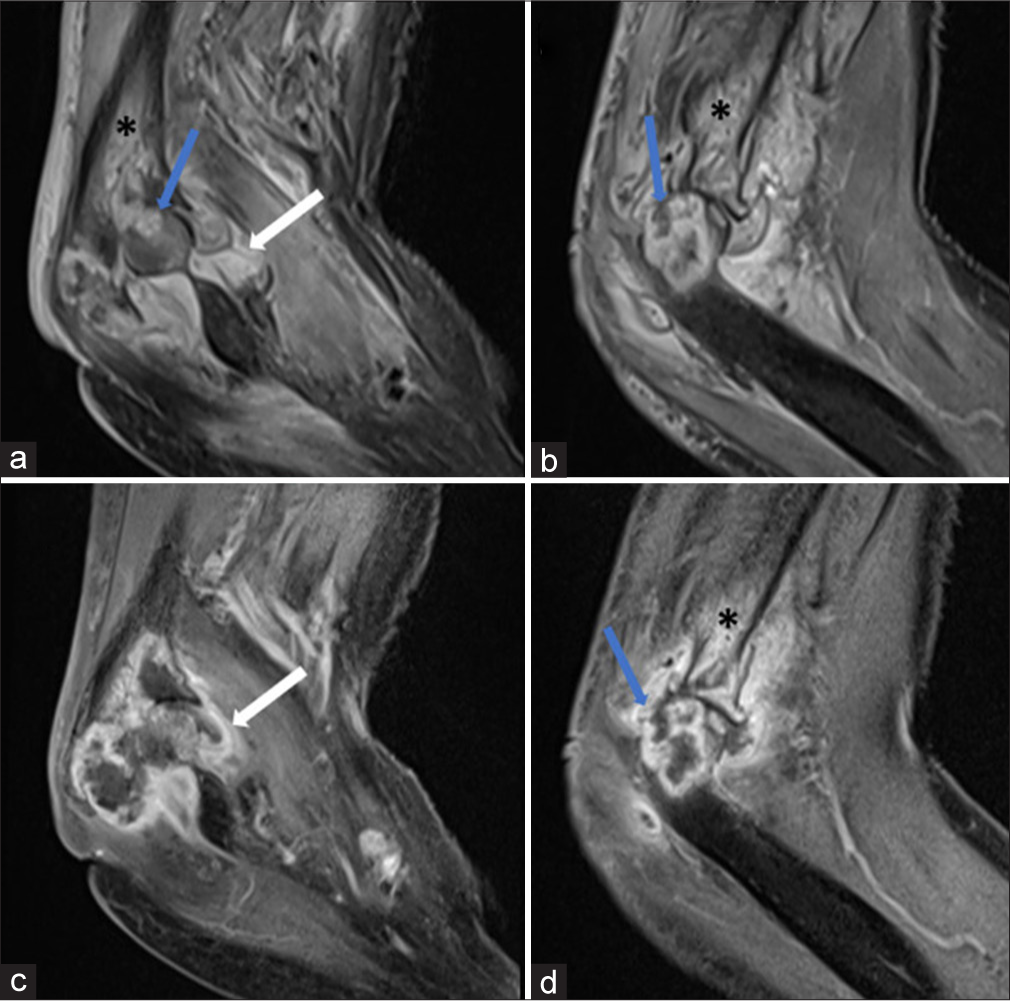
Tubercular arthritis of the elbow accounts for 2–5% of cases of skeletal tuberculosis (TB).[8] Unlike bacterial arthritis, tubercular arthritis of the elbow has more indolent course. Most patients are young with female predominance and preferential involvement of the right elbow. Clinical findings are non-specific and include pain, swelling, and loss of motion. Enlarged supratrochlear and axillary lymph nodes can be seen. Associated discharging sinus can be seen in approximately 18% of patients. The sinus tract in these cases may communicate with lymph node or joint space.[9] Disease process usually originates from the lower end of humerus or the olecranon process.[10] Synovial effusion and thickening are the most common imaging findings. T2 hypointense signal in the synovium due to the presence of granuloma has been considered characteristic for tubercular arthritis. Associated osteomyelitis and intraosseous abscesses are also frequent findings [Figure 6]. Due to its indolent nature, tubercular arthritis of the elbow can be difficult to differentiate from mono-articular RA. It has been shown that a greater degree of synovial thickening favors a diagnosis of rheumatoid arthritis, while larger erosions with peripheral enhancement and extra-articular cystic masses favor TB.[11] The presence of large collections, soft-tissue edema, and associated sinus tract [Figure 7] also favor a diagnosis of tubercular arthritis. It can be difficult to differentiate tubercular from pyogenic arthritis. However, the presence of bone erosions, absence of subchondral marrow signal changes, and presence of smoothly enhancing thin-walled abscess favor a diagnosis of tubercular over pyogenic arthritis. While, thick- walled irregularly enhancing abscesses are more common in pyogenic arthritis.[12]

- (a) Sagittal T2 weighted fat saturated, (b) sagittal T1 weighted and (c) sagittal contrast enhanced images in tubercular arthritis reveal a peripherally enhancing collection along the intermuscular planes of elbow showing intra-articular extension (white arrow in a-c) with presence of joint effusion and synovial enhancement. Adjacent bones show altered signal intensity (T2 hyper and T1 hypointense) with heterogenous post contrast enhancement.
- (a) Sagittal T2 fat saturated, (b) sagittal and (c) axial post contrast T1 weighted images reveal elbow joint effusion (white arrow in a) with marked synovial thickening and enhancement (blue arrow in a and b) and bony erosions (black arrow in b) in a case of tubercular arthritis. A sinus tract (curved arrow in c) was also seen extending from medial epicondyle of humerus to overlying skin surface. Also note associated soft tissue edema.
Crystal deposition disease
Calcium pyrophosphate dihydrate crystal deposition disease (CPPD)
Like elsewhere in the body, general radiographic features of CPPD in the elbow joint include calcification of articular and periarticular structures with pyrophosphate arthropathy. Crystal deposition in the triceps tendon is specific to the elbow. Joint space narrowing, cysts, sclerosis, and bony resorption can be seen in the proximal radius and ulna. Cubital tunnel syndrome has also been reported as a complication of CPPD deposition.[13,14] Intraarticular calcifications can be easily overlooked on routine MRI sequences and are more conspicuous on gradient sequences due to the presence of blooming effect.
Hydroxyapatite crystal deposition disease
Hydroxyapatite crystal deposition is characterized by periarticular and intra-articular calcification around the elbow joint, appearing low signal intensity on all MRI sequences.[13] The calcification may incite an inflammatory response in the bursa, tendon sheath, or articular structures. Bony erosions and marrow edema can also be seen in some cases.
Gout
Gout is characterized by episodic attacks of synovial inflammation with the development of erosive changes and articular and periarticular soft-tissue calcifications. Three clinical stages of gout have been described: Acute, intercritical (interval phase between attacks), and chronic tophaceous gout. During an acute attack, the MRI reveals non-specific synovitis. With repeated attacks, there is development of characteristic erosions with overhanging edges and associated soft-tissue calcification. Tophi are seen in chronic stages which show low signal intensity on T1-weighted images but heterogeneous signal intensity on fluid-sensitive sequences[15-17] [Figure 8]. Bilateral soft-tissue swelling over the extensor surface of elbow can occur due to bursal inflammation.
- (a) Sagittal T2 weighted and (b) proton density fat saturated images in a patient with chronic gout reveal subcutaneous tophaceous deposit overlying olecranon process (white arrow in a and b).
Hemophilia
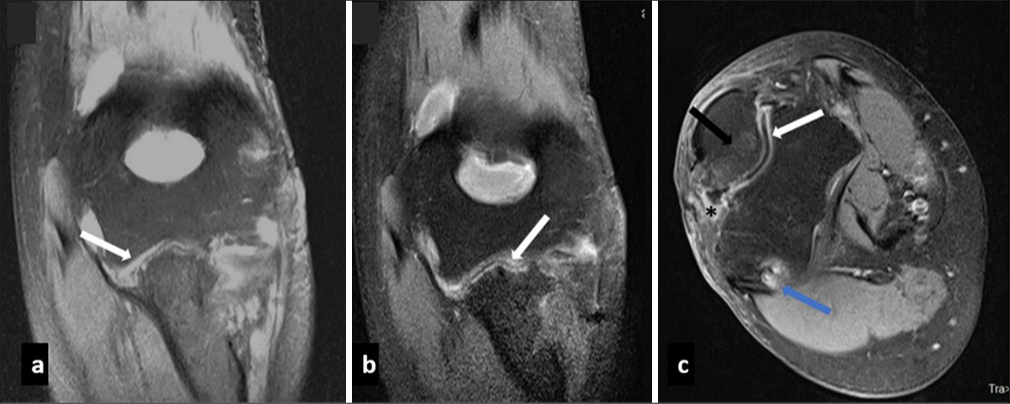
Hemophilic arthropathy occurs in the first and second decades of life and is characterized by repeated bleeding into the joint space with the development of arthropathic changes. Hemarthroses can occur spontaneously or secondary to trauma. After the knee and ankle, the elbow is third most common joint to be involved.[18] Repeated episodes of hemarthrosis result in the hemosiderin absorption in the synovial membrane leading to synovial hypertrophy and inflammation. This pannus leads to the destruction of articular cartilage resulting in erosions and subchondral cyst formation. Joint effusion, osteoporosis, cartilaginous, and osseous destruction are seen in the hemophiliac arthropathy of the elbow. The radial and trochlear notches of the ulna are widened with enlargement of the radial head. Muscle contractures and soft-tissue pseudotumors can occur due to chronic bleeding. MRI findings in the acute phase demonstrate hemarthrosis and synovitis. Areas of low signal intensity are seen on T1 and T2-weighted sequences, which correspond to areas of hemosiderin deposition in the synovium. Gradient-echo imaging is a more sensitive means to detect blood products in the synovium. Associated erosions and subchondral cysts are also seen [Figure 9]. In the chronic stage, the joints become fibrosed and disorganized with exposure to subchondral bone.[19]
- (a) Coronal T1 weighted, (b) sagittal T2 weighted and (c) proton density fat saturated images in a haemophilic patient reveal synovial thickening which appears hypointense on both T1 and T2 weighted images (white arrow in a and b) suggestive of hemosiderin deposition. Also note associated mild joint effusion (small white arrow in c) and articular surface erosions (curved arrow in c).
Synovial osteochondromatosis
Synovial osteochondromatosis is a proliferative and metaplastic disorder characterized by the presence of multiple cartilaginous or osseocartilaginous bodies within the joint space or synovial lined structure. The most common sites of occurrence are the knee followed by the elbow, hip, and shoulder.[20] It may occur as primary or secondary form. Primary osteochondromatosis is uncommon and presents as uniform-sized intra-articular bodies, distributed throughout the joint. Secondary osteochondromatosis form is fairly common and occurs on a background of degenerative joint disease.[19] Cartilaginous bodies are lobulated in appearance with intermediate to low signal intensity on T1-weighted sequences and high signal intensity on fluid-sensitive sequences.[21] These cartilaginous bodies show heterogenous post-contrast enhancement, thereby differentiating them from synovial fluid.[22] Calcified intraarticular bodies appear as foci of low signal intensity on both T1-weighted and fluid-sensitive sequences.[23]
TGCT
TGCT is a monoarticular, synovial proliferative process which may occur in localized or diffuse form. The diffuse form usually involves large joints and may affect the synovial lining, bursae, or tendon sheaths. The knee is the most frequently involved joint followed by the hip, ankle, shoulder, and elbow.[18] MRI is the imaging modality of choice for the diagnosis and surgical planning. TGCT appears as diffuse or nodular synovial thickening, appearing low-to-intermediate signal intensity on T1-weighted images and low signal intensity on T2-weighted images. Areas of low signal intensity on T2-weighted images are due to magnetic susceptibility effect caused by hemosiderin and are more prominent in long-standing cases and gradient echo sequences.[18] Bone erosions, reactive marrow edema, and extra-articular spread of the lesion can also be seen.[17]
Neuropathic arthropathy
Neuropathic arthropathy or Charcot joint is a progressive degenerative arthropathy secondary to a chronic neurological disorder. Neuropathic arthropathy of the elbow joint is rare and usually presents with instability and subluxation. Syringomyelia is the most common cause of neuropathic arthropathy of the shoulder. Other causes include diabetes, syphilis, and congenital insensitivity to pain. Radiologically mixed atrophic and hypertrophic type is seen.[24,25] Various findings of neuropathic joint include large joint effusions, osseous debris, joint destruction, disorganization, subluxation/dislocation, and periarticular soft-tissue swelling [Figure 10]. Hypertrophic changes such as osteophytes, osseous debris, and periarticular new bone formation are more frequently found in elbow joint.[26] Compression of ulnar and posterior interosseous nerves are known complication of neuropathic elbow.[24]
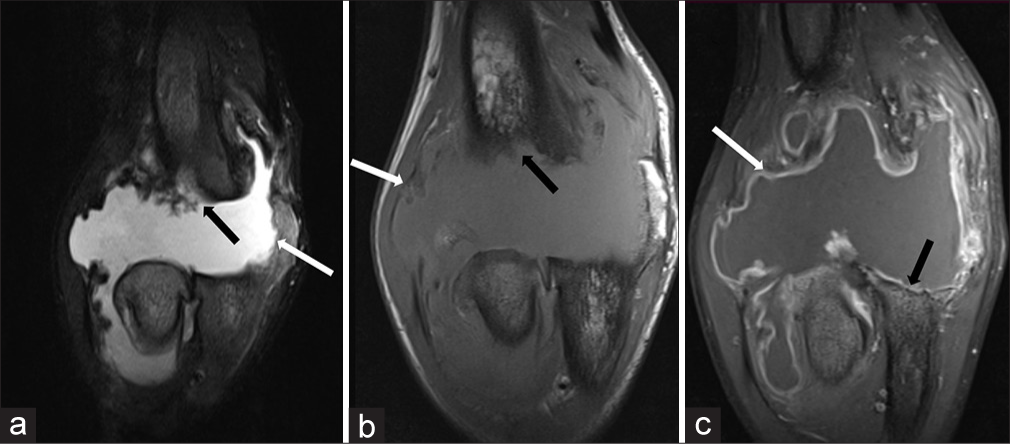
- (a) Coronal T2 weighted fat saturated, (b) coronal T1 weighted and (c) coronal post contrast images in a patient with neuropathic arthropathy reveal disorganization of elbow joint with gross joint effusion and synovial enhancement (white arrow in a-c). In addition, there is complete resorption of distal humerus (black arrow in a, b), proximal ulna (black arrow in c) and radial head.
CONCLUSION
MRI is helpful in the early diagnosis of various arthropathies affecting the elbow joint. Familiarity with the imaging findings is crucial in making a timely and accurate diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Primary and posttraumatic arthritis of the elbow. Arthritis. 2013;2013:473259.
- [CrossRef] [PubMed] [Google Scholar]
- The elbow In: Stoller DW, ed. Magnetic resonance imaging in orthopaedics and sports medicine. United States: Lippincott Williams and Wilkins; 2007. p. :1463-625.
- [Google Scholar]
- The pattern of ageing of the articular cartilage of the elbow joint. J Bone Joint Surg Br. 1967;49:175-81.
- [CrossRef] [Google Scholar]
- MR imaging: Arthropathies and infectious conditions of the elbow, wrist, and hand. Radiol Clin. 2006;44:625-42.
- [CrossRef] [PubMed] [Google Scholar]
- Nerve entrapment at the elbow in rheumatoid arthritis. Rheumatol Rehabil. 1975;14:212-7.
- [CrossRef] [PubMed] [Google Scholar]
- Arthropathies and inflammatory conditions of the elbow. Magn Reson Imaging Clin N Am. 1997;5:603-17.
- [CrossRef] [PubMed] [Google Scholar]
- The septic versus nonseptic inflamed joint: MRI characteristics. Skeletal Radiol. 1999;28:616-20.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging findings in tubercular arthritis of elbow. Clin Imaging. 2016;40:114-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis of elbow: A clinicoradiological correlation. Indian J Orthop. 2012;46:2.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis of the elbow. A report of 10 cases. Acta Orthop Scand. 1995;66:57-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rheumatoid arthritis and tuberculous arthritis: Differentiating MRI features. AJR Am J Roentgenol. 2009;193:1347-53.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculous versus pyogenic arthritis: MR imaging evaluation. Radiology. 2001;218:848-53.
- [CrossRef] [PubMed] [Google Scholar]
- Cubital tunnel syndrome associated with calcium pyrophosphate dihydrate crystal deposition disease. J Hand Surg Am. 1996;21:870-4.
- [CrossRef] [PubMed] [Google Scholar]
- Acute calcific periarthritis of the hand and elbows in women. A study and review of the literature. J Rheumatol. 1993;20:1533-8.
- [Google Scholar]
- MR imaging of tophaceous gout. AJR Am J Roentgenol. 1997;168:523-7.
- [CrossRef] [PubMed] [Google Scholar]
- Monoarticular gout following trauma: MR appearance. J Comput Assist Tomogr. 1993;17:151-3.
- [CrossRef] [PubMed] [Google Scholar]
- Tophaceous gout in an amputation stump in a patient with chronic myelogenous leukemia. Skeletal Radiol. 2003;32:429-31.
- [CrossRef] [PubMed] [Google Scholar]
- Nonseptic monoarthritis: imaging features with clinical and histopathologic correlation. Radiographics. 2000;20 Spec No: S263-78
- [CrossRef] [PubMed] [Google Scholar]
- Miscellaneous disorders of the elbow In: Chung CB, Steinbach LS, eds. MRI of the upper extremity, Shoulder, elbow, wrist and hand. United States: Lippincott Williams and Wilkins; 2010. p. :491-525.
- [Google Scholar]
- Synovial chondromatosis in a lumbar apophyseal joint. Skeletal Radiol. 1998;27:385-7.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic synovial osteochondromatosis of the hip: Radiographic and MR appearances in 15 patients. Korean J Radiol. 2002;3:254-9.
- [CrossRef] [PubMed] [Google Scholar]
- Primary synovial chondromatosis and synovial chondrosarcoma: A pictorial review. Eur Radiol. 2002;12:2112-9.
- [CrossRef] [PubMed] [Google Scholar]
- Synovial osteochondromatosis of the shoulder: MR findings. J Comput Assist Tomogr. 1989;13:360-1.
- [CrossRef] [PubMed] [Google Scholar]
- The many facets of neuropathic arthropathy. BJR Open. 2019;1:20180039.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple sclerosis neuropathic arthropathy of elbow: Report of a rare case and literature review. J Orthop Trauma Rehabil. 2019;26:52-5.
- [CrossRef] [Google Scholar]
- Neuropathic arthropathy of the elbow. A report of five cases. J Bone Joint Surg Am. 2001;83:839-44.
- [CrossRef] [PubMed] [Google Scholar]







