Translate this page into:
Can we Rotate the Head Safely During Cervical Nerve Root Injection?

*Corresponding author: Dr. Rajesh Botchu, Department of Musculoskeletal Radiology, Royal Orthopedic Hospital, Bristol Road South, Birmingham, West Midlands, B31 2AP, United Kingdom. drbrajesh@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Iqbal A, McLoughline E, James S, Botchu R. Can we Rotate the Head Safely During Cervical Nerve Root Injection? Indian J Musculoskelet Radiol 2020;2(1):32-5.
Abstract
Objectives:
Trans-foraminal epidural injections have been used successfully to aid in the management of cervicobrachialagia. The aim of this study was to assess the cross sectional area of the vertebral artery during transforaminal cervical nerve root injections (TFCNRI) when the head is typically rotated and to compare with the neutral position cross sectional area. We hypothesize that head rotation does not lead to a change of vertebral artery calibre at the neural foramen, thus this technique can be performed relatively safely during TFCNRI.
Material and Methods:
A pilot study involving a retrospective review of 16 computed tomography guided TFNRI was performed and cross sectional area of vertebral artery with head tilted and head in neutral position was performed.
Results:
There was no correlation between the degree of head rotation and change in the area of the ipsilateral or contralateral vertebral artery.
Conclusion:
We suggest that head can safely be rotated to varied degrees while performing TFCNRI.
Keywords
Cervical
Head
Rotation
Nerve root injection
INTRODUCTION
Cervicobrachialagia (CBA) refers to pain arising in the cervical region and radiating down the arm and is commonly due to a disc osteophyte complex causing narrowing of the cervical exiting foramen.
The incidence of CBA is around 82/100,000, with a slight female predominance, and peak incidence between 40 and 60 years. Trans-foraminal epidural injections have been used successfully to aid in the management of this condition. This results in a decrease in the oedema of the nerve roots and sensitisation of C-fibres.[1-3]
Prior to performing a nerve root injection, the patient must be consented and the risks associated with the procedure explained including pain during the procedure, bleeding, infection, nerve root injury, failure to respond to injection, syncope, transient hoarseness and stroke/paralysis.[4-10] The risk of stroke/paralysis is thought to relate to vasospasm of the ipsilateral vertebral artery due to its close proximity with the adjacent nerve root.[10]
The vertebral artery lies in close proximity to the exiting nerve roots [Figure 1]. It is well known that there is considerable variation in the cross sectional area and course of the vertebral arteries and it is also apparent that there is variation in blood flow and cross sectional area with head rotation. We also hypothesize that the nerve, which lies posterior to, the vertebral artery can change in dimensions and morphology resulting in alteration of pressure and course of nerve on head tilt. The aim of this study was to assess the cross sectional area of the vertebral artery during transforaminal cervical nerve root injections (TFCNRI) when the head is typically rotated and to compare with the neutral position cross sectional area. We hypothesize that head rotation does not lead to a change is vertebral artery calibre at the neural foramen, thus this technique can be performed relatively safely during TFCNRI.

- Diagrammatic representation of anatomy of cervical spine. N (needle), VA (vertebral artery).
MATERIAL AND METHODS
After obtaining institutional review board approval, a pilot study involving a retrospective review of 16 consecutive computed tomography (CT) guided TCFNRI was performed. All procedures were undertaken in the supine position with a varied degree of head rotation. The needle was inserted via an anterolateral approach with the spinal needle position confirmed with contrast (Omnipaque 240). Following this 1 ml of 1% lidocaine and 3.3 mg of dexamethasone was injected [Figure 2]. At the end of the procedure, final images were obtained with the head in a neutral position to assess the final distribution of contrast post steroid injection. The demographics of the patient cohort were analysed. The vertebral artery cross sectional area was measured at the level of the exit foramen in both positions (neutral and with head rotation) after magnifying the image by 400% [Figure 3]. Measurements were completed in the soft tissue window setting as there was better contrast resolution between the vertebral artery and surrounding tissues. A line was drawn perpendicular to the CT table centered over the midpoint of the posterior arch of the vertebra (A) and another by joining the midpoint of the posterior arch of the vertebra and mid point of the mandible or maxilla (B). The degree of head rotation was calculated by measuring the angle between A and B [Figure 4]. The data was analysed using a t-test.
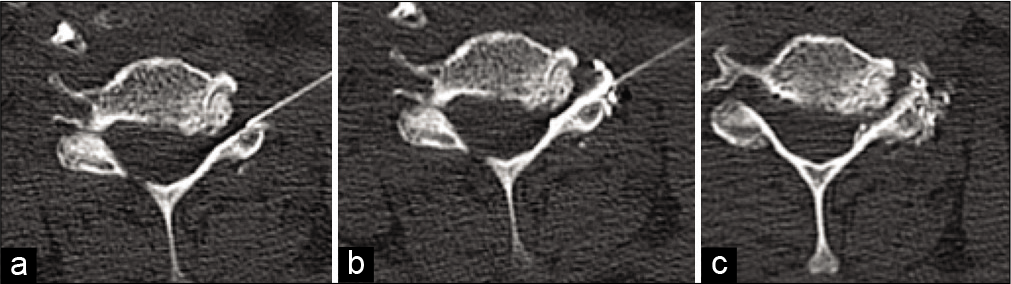
- Axial CT images (a) showing needle over the left facet, (b) after injection of omnipaque contrast and (c) after injection of dexamethasone and 1% lidocaine.
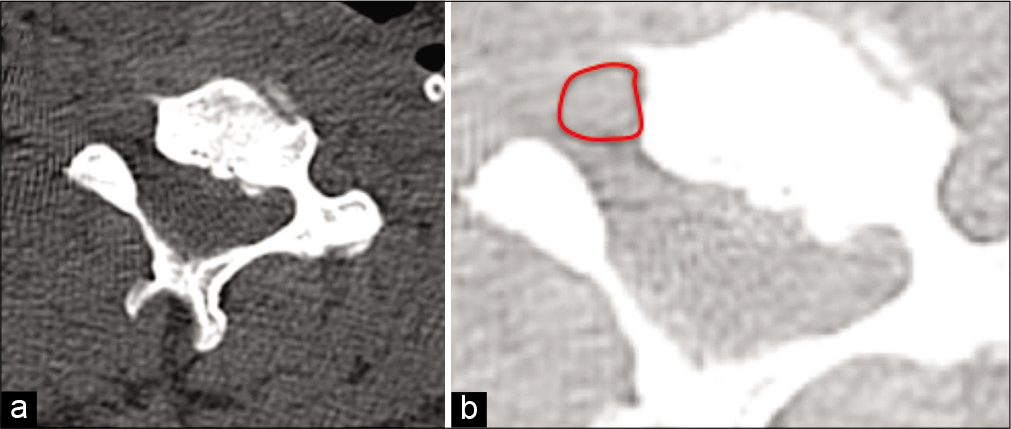
- Axial CT (a) and (b) with 400% magnification(soft tissue window) showing area of the vertebral artery (red circle).
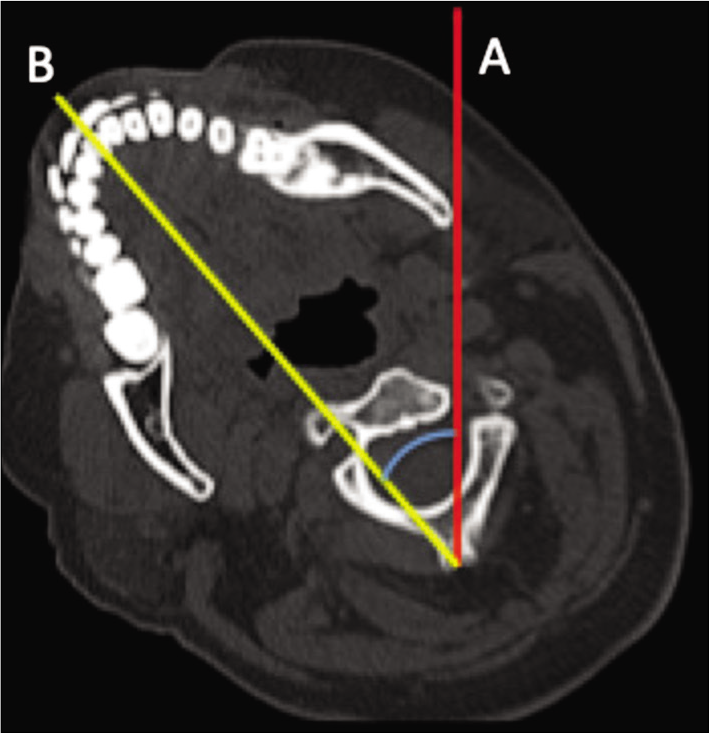
- Axial CT showing angle of rotation calculated by drawing the line A (line perpendicular to the CT table centered over the posterior arch of the vertebra) and B (connecting the midpoint of the posterior arch of vertebra and midpoint of the mandible).
In addition to the data collection we performed a survey of musculoskeletal radiologists in UK to ascertain if they rotate the head during TFCNRI. This was performed via survey monkey and questions included extent of rotation and prevalence of complications.
RESULTS
The average age of the patient cohort was 56.5 years (43–77 years) with a female predominance (6 male and 10 females). The level of nerve root injections was C6 in 11 patients, C7 in four and one had C5. There were 6 left sided nerve root injection and 10 right sided. There were varying degrees of rotation ranging from 16.9 to 47.5 degrees with an average of 36.2 degrees. The average change of cross sectional area of the ipsilateral artery with head rotation was 8.7 mm2 (−4.3 to 22.6) and that of contralateral vertebral artery was 7.9 mm2 (−6.7 to 17.9). There was no correlation between the degree of head rotation and change in the area of the ipsilateral or contralateral vertebral artery.
There were 35 responses to our online survey. 37% of respondents rotated the head and the degree of rotation was <10 degrees (13%), 10–20 degrees (25%), 20–30 degrees (33%) and 30–40 degrees (27%). There were 3 episodes of transient Horner’s syndrome (no head rotation), which recovered, and one vasovagal (30–40 degrees of rotation).
DISCUSSION
The vertebral artery is a branch of the subclavian artery and has four segments. The second part courses through the transverse foramen of the C6 vertebra upto C1. There is variation of the course of the vertebral artery in upto 20% of patients with the vertebral artery traversing through the transverse foramen of C7 in 7.5%. The cervical nerve root exits through the intervertebral foramen, posterior to vertebral artery along the groove on the transverse process.
TFCNRI is a diagnostic and often therapeutic treatment for cervical radiculopathy.[3] Variation of normal vertebral anatomy might predispose to accidental injection of local anaesthetic or steroids that could result in serious complications. The normal variation of corkscrew morphology can result in posterolateral displacement of the vertebral artery at one or more levels.[11] An accessory vertebral artery which can lie posterior to the nerve root is a rare anatomic variation and if present and may lie along the path of the needle for cervical nerve root injection.
Head rotation in the supine position results in a decrease in contralateral blood flow of the vertebral artery and an increase in the ipsilateral blood flow of the vertebral artery.[12] This has been suggested to be related to the extent of rotation.[13] The possible explanation for the decrease in blood flow is due to stretching of the vertebral artery and compression accentuated by osteophytes. This change is accentuated in older patients with cervical spondylosis where there may be subsequent impingement of osteophytes onto the vertebral artery compounded by atherosclerosis and a decrease in elasticity of the artery.[12,13]
Aristokleous et al. had demonstrated that the vertebral artery curvature is not altered in the prone or supine position.[14] However the extent of tortuosity of the right vertebral artery had significantly increased with rotation of the head to the right in some cases but this was not consistent in the entire cohort. Sakaguchi et al. concluded that there was minimal change in blood flow through the vertebral artery during rotation of neck in the majority of their cohort of 1108 subjects who were all assessed using ultrasound doppler. In the minority of cases (<5%) there was compression of the vertebral artery with head rotation.[12]
One needs to be aware of Bow Hunter’s syndrome, which is an uncommon cause of vertebrobasilar insufficiency due to compression of the vertebral artery by a fibrous band or bony prominence during rotatory movement of the head.[15] Mitchell had shown a significant decrease in the blood flow of the contralateral vertebral artery in cadavers.[13] Quesnele et al. showed an increase in blood flow in the ipsilateral vertebral artery though this was not statistically significant. Overall therefore, there are conflicting studies in the literature regarding the effect of head rotation on the flow of vertebral artery.[16]
In our pilot project of 16 patients, there was no correlation between the degree of head rotation and change in the area of the ipsilateral or contralateral vertebral artery. There is a direct correlation between diameter of the artery and blood flow.[17] It appears that head rotation does not affect the cross sectional area of the vertebral artery. Our results, coupled with results from the study by Sakaguchi et al. imply that complications related to the vertebral artery calibre are unlikely to occur with head rotation. Hence we suggest that the head can safely be rotated to varied degrees while performing TFCNRI in order to increase visibility and access to the target site.
Small cohort is one of the limitations of our study.
CONCLUSION
We suggest that head can safely be rotated to varied degrees while performing TFCNRI.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Does pain relief by CT-guided indirect cervical nerve root injection with local anesthetics and steroids predict pain relief after decompression surgery for cervical nerve root compression? Acta Neurochir (Wien). 2016;158:1869-74.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided cervical nerve root block: Does volume affect the spreading pattern? Pain Med. 2016;17:1978-84.
- [CrossRef] [PubMed] [Google Scholar]
- CT-guided cervical selective nerve root block with a dorsal approach. AJNR Am J Neuroradiol. 2010;31:1831-6.
- [CrossRef] [PubMed] [Google Scholar]
- Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehabil. 2005;86:277-83.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and complications of cervical epidural steroid injections. Phys Med Rehabil Clin N Am. 2018;29:155-69.
- [CrossRef] [PubMed] [Google Scholar]
- Major risks and complications of cervical epidural steroid injections: An updated review. Surg Neurol Int. 2018;9:86.
- [CrossRef] [PubMed] [Google Scholar]
- Hemiparesis and facial sensory loss following cervical epidural steroid injection. Pain Physician. 2014;17:E761-7.
- [Google Scholar]
- Transforaminal cervical nerve root block: Outcomes and complications. Coluna/ Columna. 2016;15:219-21.
- [CrossRef] [Google Scholar]
- Spinal cord infarction after cervical transforaminal epidural steroid injection: Case report and literature review. Case Rep Neurol. 2017;9:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Transient quadriplegia after fluoroscopic-guided selective cervical nerve root block in a patient who received cervical interbody fusion-a case report. Korean J Anesthesiol. 2010;59:S95-8.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral artery anatomical variations as they relate to cervical transforaminal epidural steroid injections. Pain Med. 2014;15:1109-14.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical compression of the extracranial vertebral artery during neck rotation. Neurology. 2003;61:845-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral artery blood flow velocity changes associated with cervical spine rotation: A meta-analysis of the evidence with implications for professional practice. J Man Manip Ther. 2009;17:46-57.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of head rotation on the geometry and hemodynamics of healthy vertebral arteries. Ann Biomed Eng. 2015;43:1287-97.
- [CrossRef] [PubMed] [Google Scholar]
- Rotational vertebral artery compression: Bow Hunter's syndrome. J Korean Neurosurg Soc. 2013;54:243-5.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in vertebral artery blood flow following various head positions and cervical spine manipulation. J Manipulative Physiol Ther. 2014;37:22-31.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of pressure and flow to arterial diameter. Invest Radiol. 1982;17:265-70.
- [CrossRef] [PubMed] [Google Scholar]






