Translate this page into:
Role of High-Resolution Ultrasonography in Evaluation of Median Nerve and Thickness of Flexor Retinaculum in Patients with Hypothyroidism

*Corresponding author: Kunwar Pal Singh, Department of Radiodiagnosis, Sri Guru Ram Das Institute of Medical Sciences and Research, Sri Amritsar, Mehta Road, Post Office Vallah, Amritsar - 143 501, Punjab, India. kpsdhami@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh KP, Gupta K, Kaur I, Arora V. Role of High-Resolution Ultrasonography in Evaluation of Median Nerve and Thickness of Flexor Retinaculum in Patients with Hypothyroidism. Indian J Musculoskelet Radiol 2020;2(1):36-43.
Abstract
Objectives:
To determine the role of high resolution ultrasonography in evaluation of cross sectional area, maximum nerve fascicle thickness and thickness/width ratio of the median nerve and flexor retinaculum thickness in patients with hypothyroidism and to correlate it with the healthy volunteers.
Material and Methods:
A prospective study was conducted from February 2018 to October 2019 on 62 patients which included 32 clinically proven cases of hypothyroidism and 30 healthy volunteers. High resolution ultrasonography was performed using high frequency linear probes.
Results:
The most affected parameter was cross sectional area of median nerve at three levels, inlet/outlet ratio of CSA of the median nerve and thickness of flexor retinaculum in hypothyroidism patients in correlation with healthy volunteers. These parameters showed statistically significant p values. Maximum nerve fascicle thickness and thickness/width ratio of the median nerve showed no statistical significance in hypothyroid patients in correlation with healthy volunteers.
Conclusion:
High-resolution ultrasonography plays an important role in evaluating the changes occuring in cross sectional area of the median nerve, its inlet/outlet CSA ratio and flexor retinaculum thickness in hypothyroidism patients as correlated with the healthy volunteers.
Keywords
Hypothyroidism
Median nerve
High resolution ultrasonography
INTRODUCTION
Hypothyroidism is a clinical disorder due to the deficiency of the thyroid hormone. This hormone is a key regulator of cellular metabolism in our body. This deficient state is estimated to affect 3.8–4.6% of the general population, with a four-fold affection in women.
Peripheral nerve dysfunction is a well-documented feature of clinical hypothyroidism. Thyroid hormone deficiency causes sensory neuropathy by affecting different peripheral nerves, especially the median nerve. The mechanism involved in the development of neuropathy in hypothyroidism still remains unclear.[1]
Carpal tunnel syndrome (CTS) is the most frequent entrapment syndrome of the upper limb; it arises due to the compression of the median nerve at the wrist, which leads to an enlargement of the median nerve cross-sectional area (CSA). An early diagnosis based on clinical and electrodiagnostic findings is essential to prevent permanent nerve damage and functional sequelae.
The pathologic mechanics observed in the carpal tunnel during activity suggest a multifactorial cause of CTS: Increased intracarpal pressure, decreased nerve mobility, nerve compression, increased stiffness of the synovium, and flexor retinaculum.
The most commonly described abnormality has been enlargement of the median nerve CSA usually proximal to the carpal tunnel.
Phalen’s maneuver can also be used in an adjunctive manner in diagnosing CTS. High-resolution ultrasound and MRI have emerged as feasible, non-invasive imaging tools for evaluating the median nerve in the carpal tunnel.[2]
Ultrasonography has emerged as an important diagnostic investigation for CTS. A number of ultrasonographic changes have been demonstrated in CTS, including swelling of the median nerve, flattening of the nerve, palmar bowing and thickening of the flexor retinaculum, and changes in the median nerve appearance.[3]
MATERIAL AND METHODS
Study design
We conducted a prospective study of 62 patients which include 32 patients of hypothyroidism (Group A) and 30 healthy volunteers (Group B) each in the department of radiodiagnosis from February 2018 to October 2019 referred for ultrasonography by the outpatient department or who were admitted to the hospital. The inclusion criteria were Group A – patients with hypothyroidism and Group B – healthy volunteers. The exclusion criteria were all patients with peripheral neuropathy due to diabetes mellitus, obesity, pregnancy, alcohol, and drug induced.
Sonography technique
The high-resolution sonography was performed using Voluson E8 Expert BT09 (Wipro GE) with linear transducers of frequency 7–11 MHz and 7–18 MHz, Affiniti 50G (Phillips Healthcare) with linear transducer of frequency 4–12 MHz or Logiq P6 (Wipro GE) with linear frequency of 7–11 MHz.
RESULTS
The study included 124 wrists of 62 patients, in which 32 patients were clinically proven cases of hypothyroidism and 30 healthy volunteers, and they underwent high-resolution ultrasonography after the clinical examination (Phalen’s test) done in hypothyroidism patients. The total number of females was 53 and the males were 9. The ages ranged from 20 to70 years with a mean age of 42 years.
The observations made during the study are summarized in Tables 1-7 and images are shown in Figures 1-8.
| Duration of disease (months) | Number of patients | % age |
|---|---|---|
| ≤24 | 15 | 46.88 |
| 24–48 | 11 | 34.38 |
| >48 | 6 | 18.75 |
| Total | 32 | 100.00 |
| Mean duration of disease | 29.09±19.29 |
| Group | Cross-sectional area (cm2) | |||||
|---|---|---|---|---|---|---|
| Right forearm | P-value | Left forearm | P-value | |||
| Mean | SD | Mean | SD | |||
| Hypothyroidism | 0.064 | 0.053 | 0.031 | 0.062 | 0.022 | 0.042 |
| Healthy | 0.053 | 0.015 | 0.052 | 0.014 | ||
| Maximum nerve fascicle thickness (cm) | ||||||
| Hypothyroidism | 0.029 | 0.011 | 0.102 | 0.032 | 0.010 | 0.106 |
| Healthy | 0.025 | 0.007 | 0.024 | 0.006 | ||
| Thickness/width ratio | ||||||
| Hypothyroidism | 3.417 | 0.927 | 0.872 | 3.605 | 0.872 | 0.932 |
| Healthy | 3.455 | 0.931 | 3.586 | 0.902 | ||
| Group | Cross-sectional area (cm2) | |||||
|---|---|---|---|---|---|---|
| Right forearm | P-value | Left forearm | P-value | |||
| Mean | SD | Mean | SD | |||
| Hypothyroidism | 0.074 | 0.022 | 0.014 | 0.073 | 0.024 | 0.034 |
| Healthy | 0.061 | 0.016 | 0.061 | 0.017 | ||
| Maximum nerve fascicle thickness (cm) | ||||||
| Hypothyroidism | 0.027 | 0.008 | 0.362 | 0.032 | 0.009 | 0.378 |
| Healthy | 0.025 | 0.007 | 0.024 | 0.006 | ||
| Thickness/width ratio | ||||||
| Hypothyroidism | 3.081 | 0.721 | 0.872 | 3.057 | 0.889 | 0.847 |
| Healthy | 3.057 | 0.428 | 3.021 | 0.481 | ||
| Group | Cross-sectional area (cm2) | |||||
|---|---|---|---|---|---|---|
| Right forearm | P-value | Left forearm | P-value | |||
| Mean | SD | Mean | SD | |||
| Hypothyroidism | 0.073 | 0.023 | 0.021 | 0.084 | 0.023 | 0.001 |
| Healthy | 0.061 | 0.016 | 0.067 | 0.015 | ||
| Maximum nerve fascicle thickness (cm) | ||||||
| Hypothyroidism | 0.031 | 0.010 | 0.371 | 0.032 | 0.009 | 0.506 |
| Healthy | 0.029 | 0.008 | 0.030 | 0.009 | ||
| Thickness/width ratio | ||||||
| Hypothyroidism | 2.699 | 1.031 | 0.504 | 2.606 | 0.908 | 0.973 |
| Healthy | 2.624 | 0.396 | 2.612 | 0.360 | ||
| Group | Flexor retinaculum (cm) | |||||
|---|---|---|---|---|---|---|
| Right forearm | P-value | Left forearm | P-value | |||
| Mean | SD | Mean | SD | |||
| Hypothyroidism | 0.058 | 0.013 | 0.001 | 0.059 | 0.012 | 0.022 |
| Controls | 0.048 | 0.010 | 0.051 | 0.014 | ||
| Group | Inlet/outlet CSA ratio | |||||
|---|---|---|---|---|---|---|
| Right forearm | P-value | Left forearm | P-value | |||
| Mean | SD | Mean | SD | |||
| Hypothyroidism | 0.975 | 0.185 | 0.009 | 0.932 | 0.141 | 0.001 |
| Controls | 0.865 | 0.132 | 0.821 | 0.124 | ||
| Phalen’s test | Inlet/outlet CSA ratio | |||||
|---|---|---|---|---|---|---|
| Right forearm | P-value | Left forearm | P-value | |||
| Mean | SD | Mean | SD | |||
| Positive | 0.988 | 0.213 | 0.029 | 0.928 | 0.160 | 0.032 |
| Negative | 0.884 | 0.135 | 0.816 | 0.122 | ||
![Anatomy of median nerve and flexor retinaculum.[4]](/content/107/2020/2/1/img/IJMSR-2-036-g002.png)
- Anatomy of median nerve and flexor retinaculum.[4]
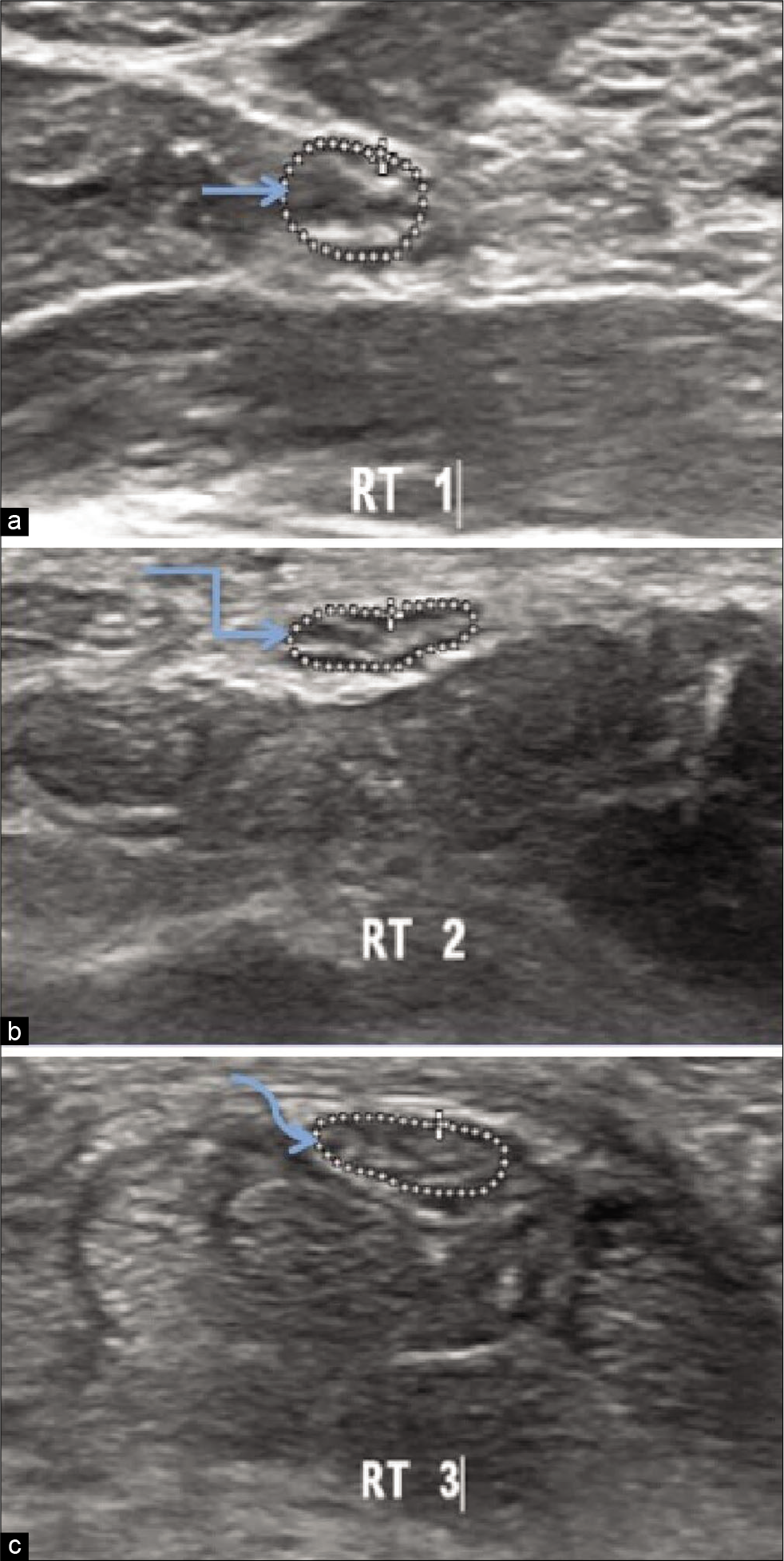
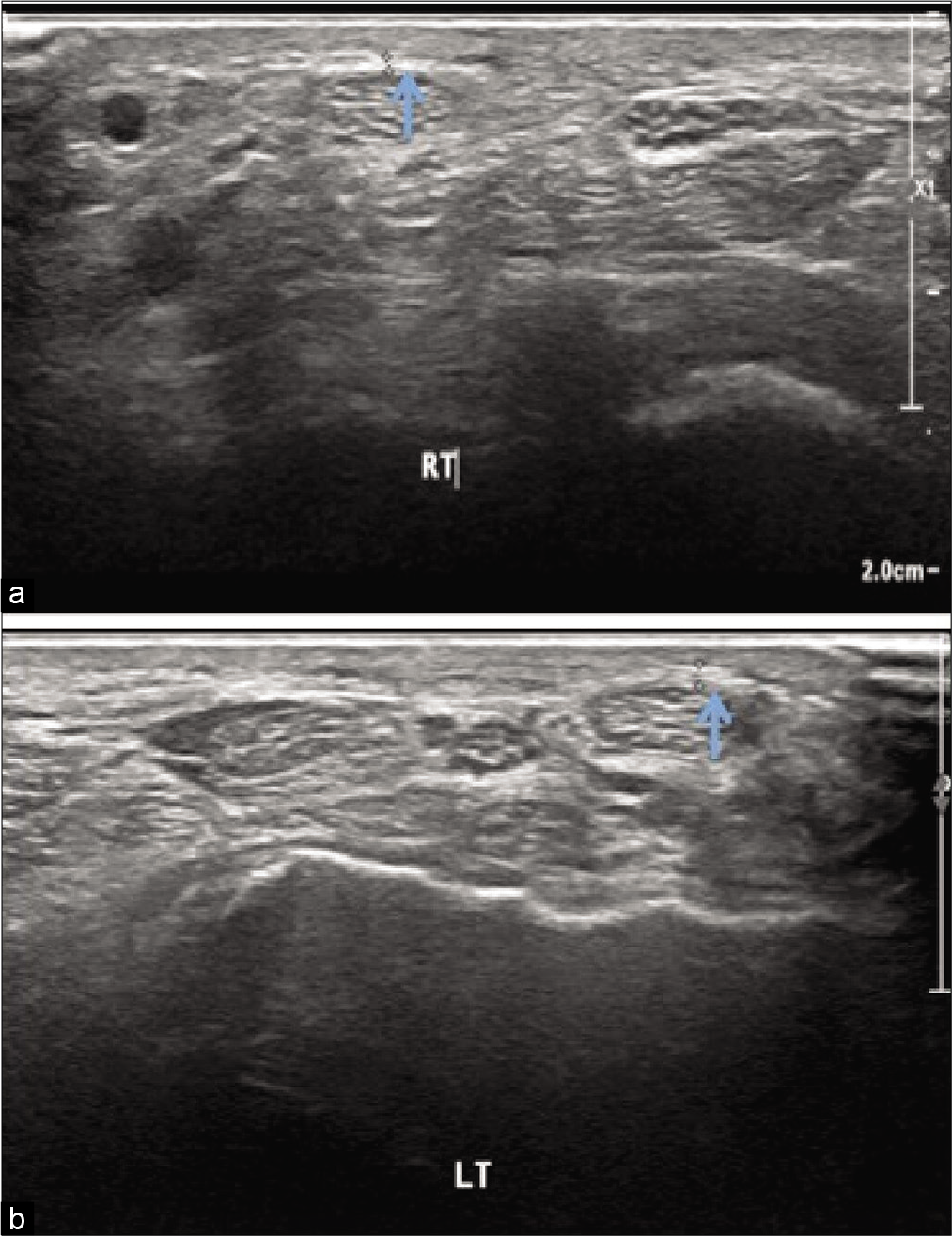
- Ultrasonography image of the right median nerve of hypothyroidism patient at three levels in distal forearm showing (a) cross sectional area 0.060 cm2 at the level of pronator quadratus (straight arrow). (b) cross sectional area 0.057 cm2 proximal to the carpal tunnel inlet.(bent arrow) (c) cross sectional area 0.053 cm2 distal to the carpal tunnel outlet (curved arrow).
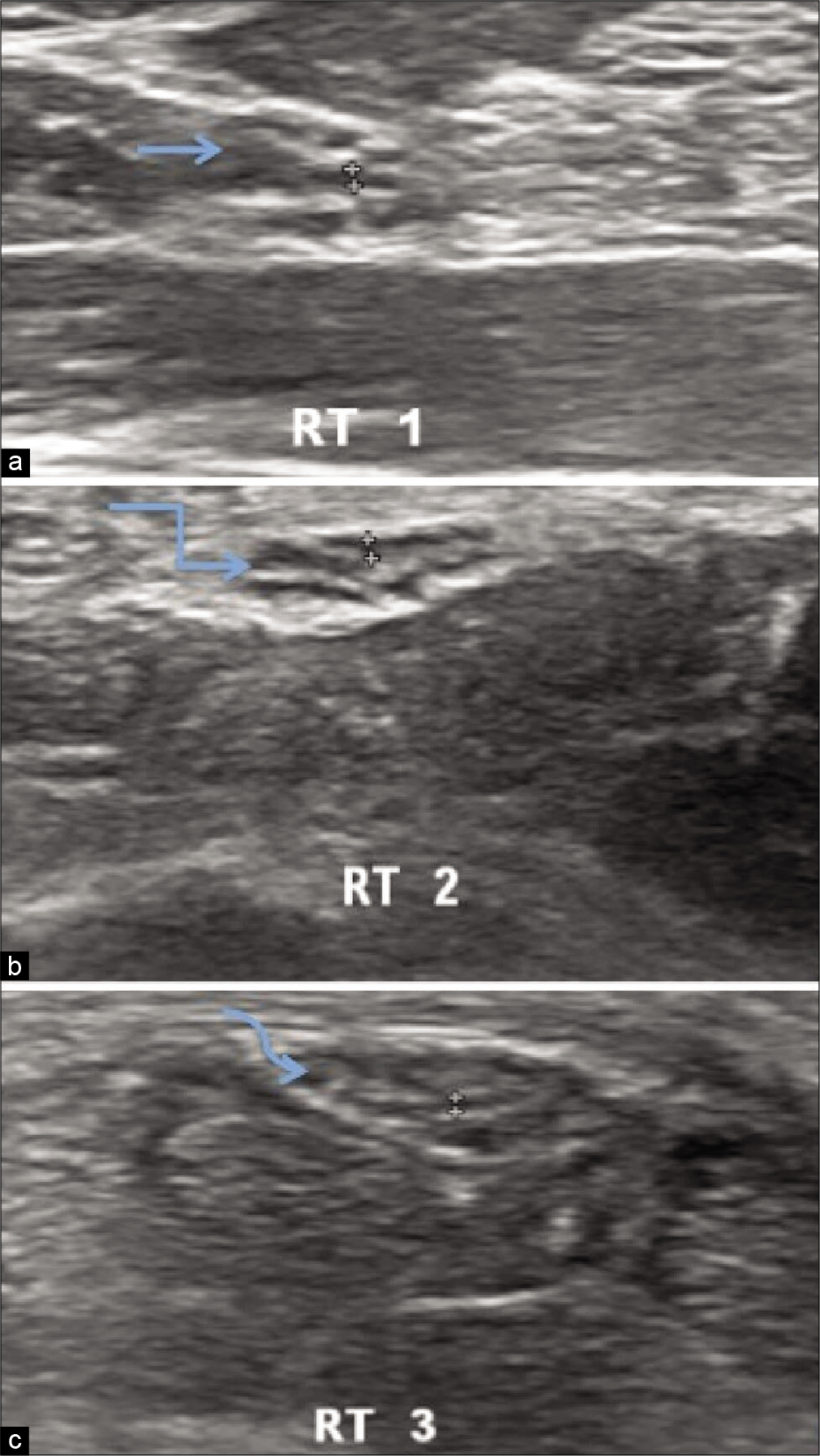
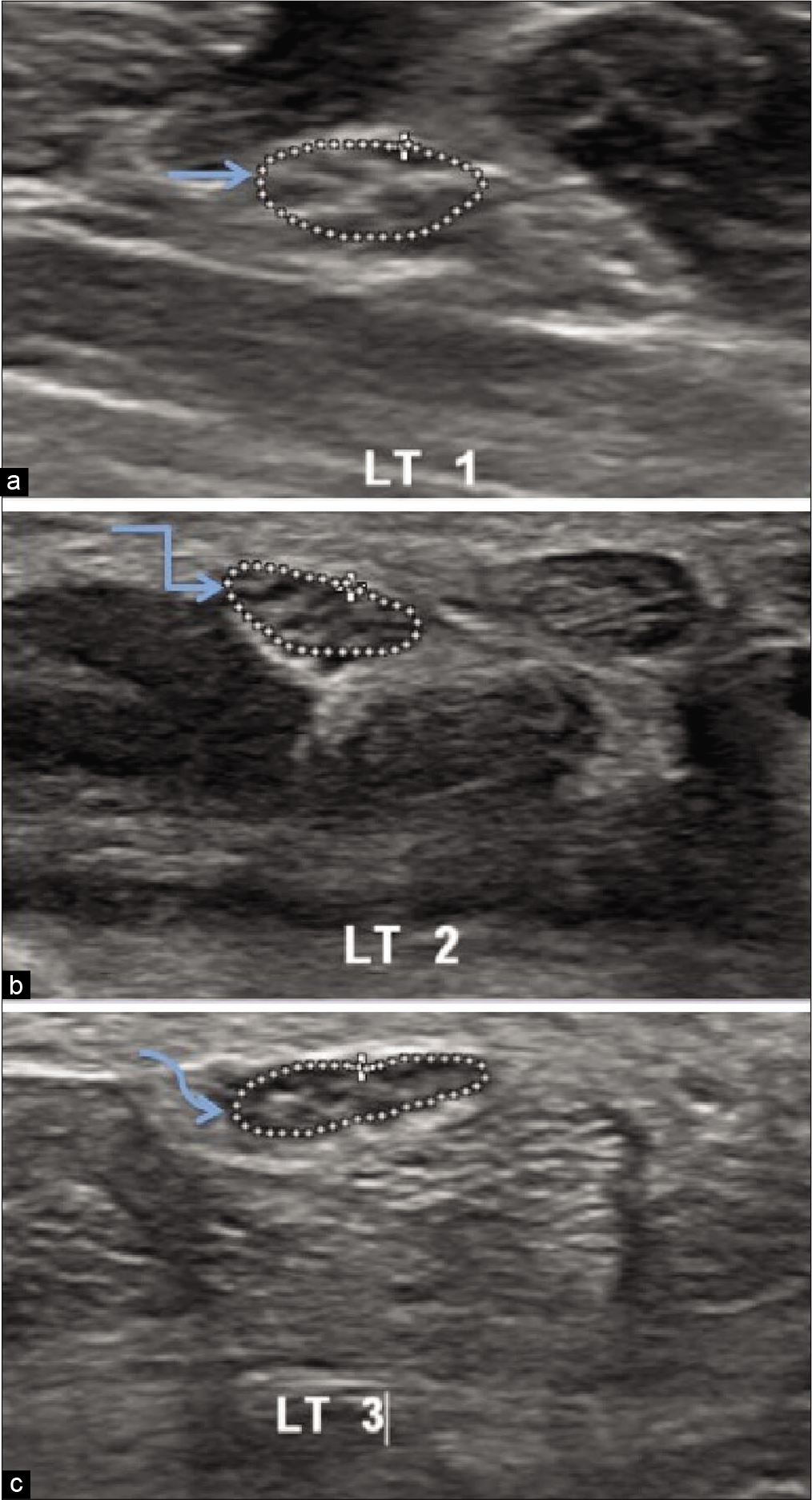
- Ultrasonography of the Right median nerve of hypothyroidism patient showing hypoechoic median nerve fascicle thickness at three levels in distal forearm (a) Maximum thickness of nerve fascicle 0.035 cm at the level of pronator quadratus(straight arrow), (b) maximum thickness of nerve fascicle 0.043 cm proximal to carpal tunnel inlet(bent arrow), (c) maximum nerve fascicle thickness 0.033 cm distal to carpal tunnel outlet(curved arrow).
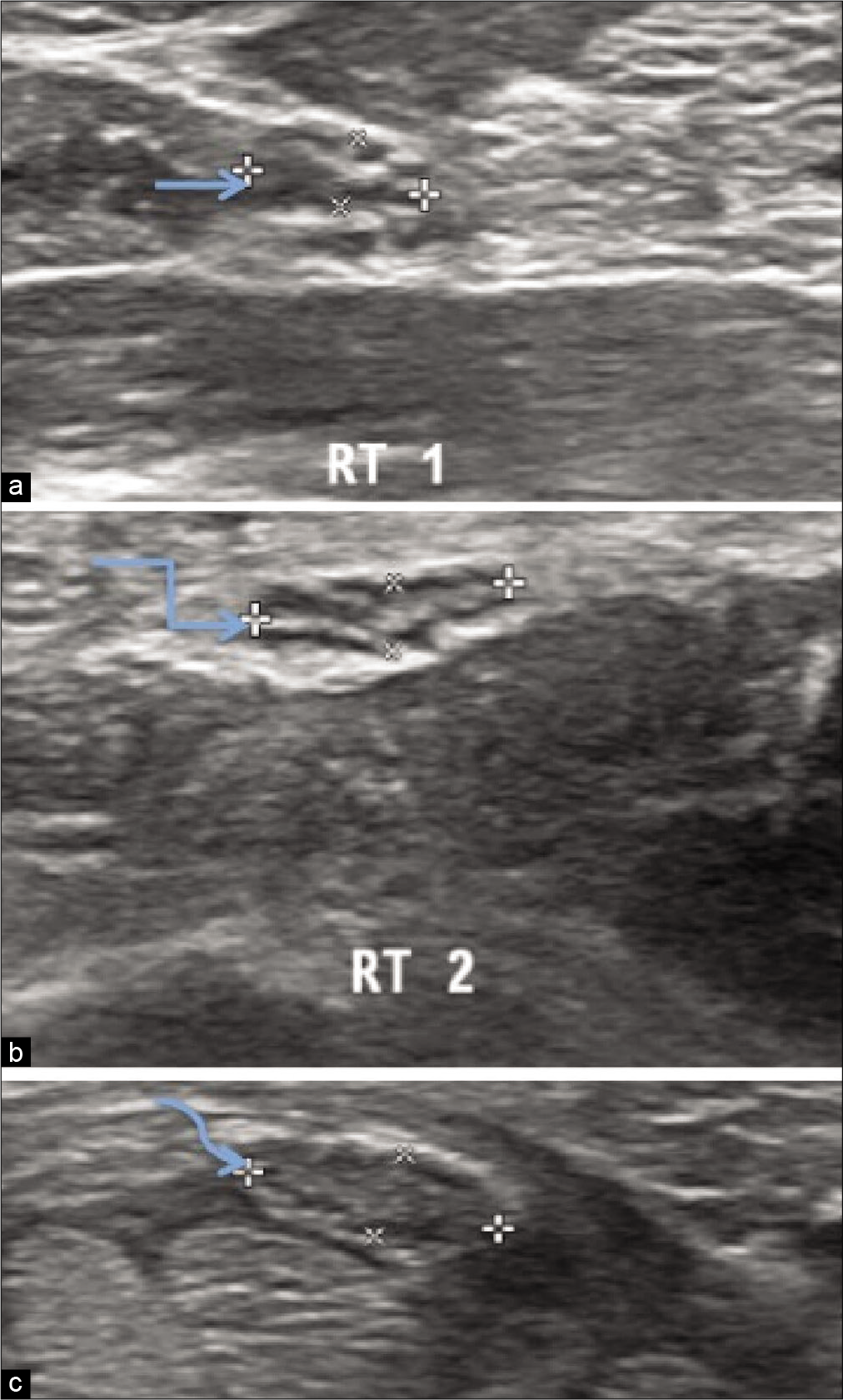
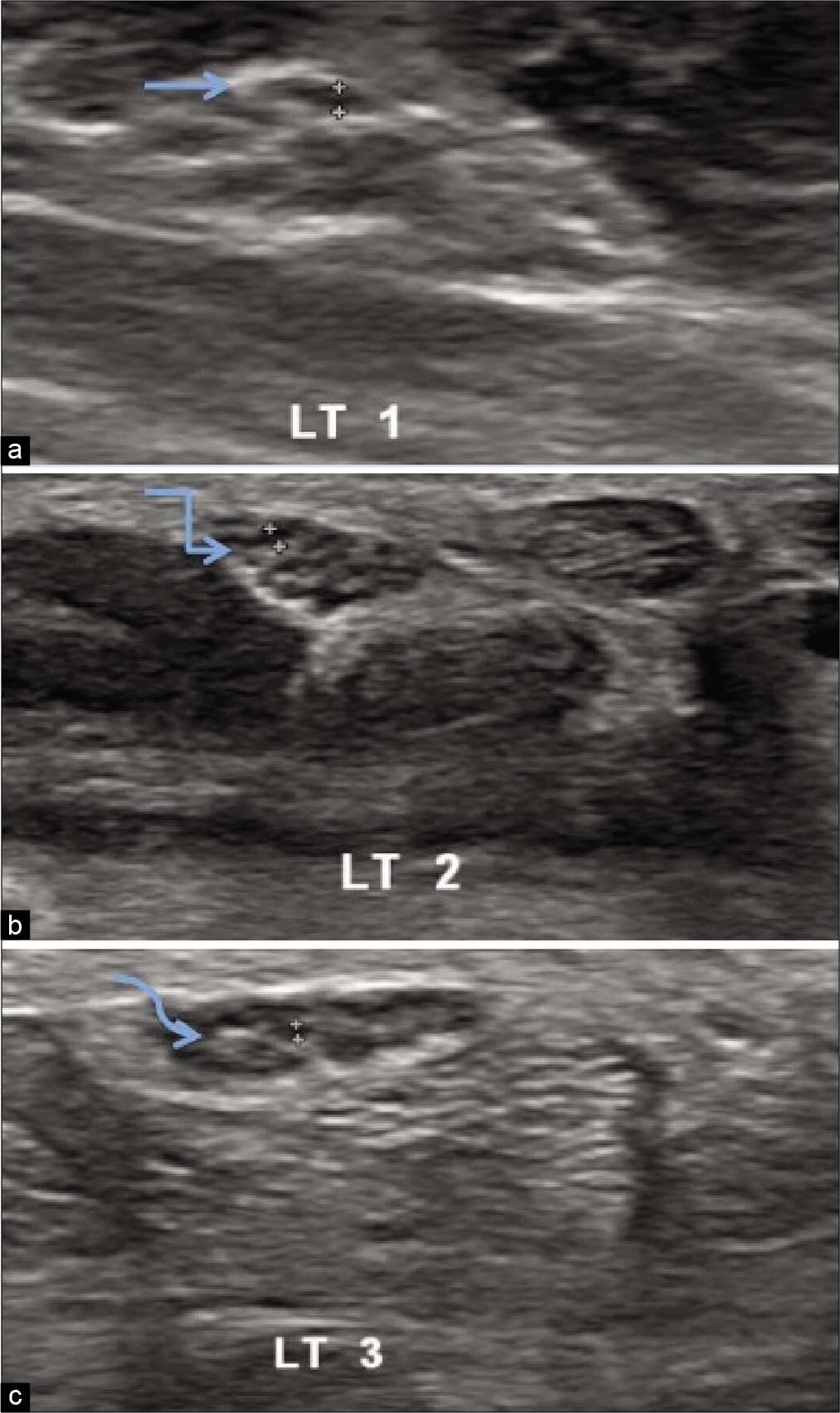
- Ultrasonography of the Right median nerve of hypothyroidism patient showing thickness /width ratio at three levels in distal forearm (a) thickness/width ratio 2.59 at the level of pronator quadratus,(straight arrow) (b) thickness/width ratio 3.23 proximal to carpal tunnel inlet, (bent arrow) (c) thickness/width ratio 2.75 distal to carpal tunnel outlet.(curved arrow).
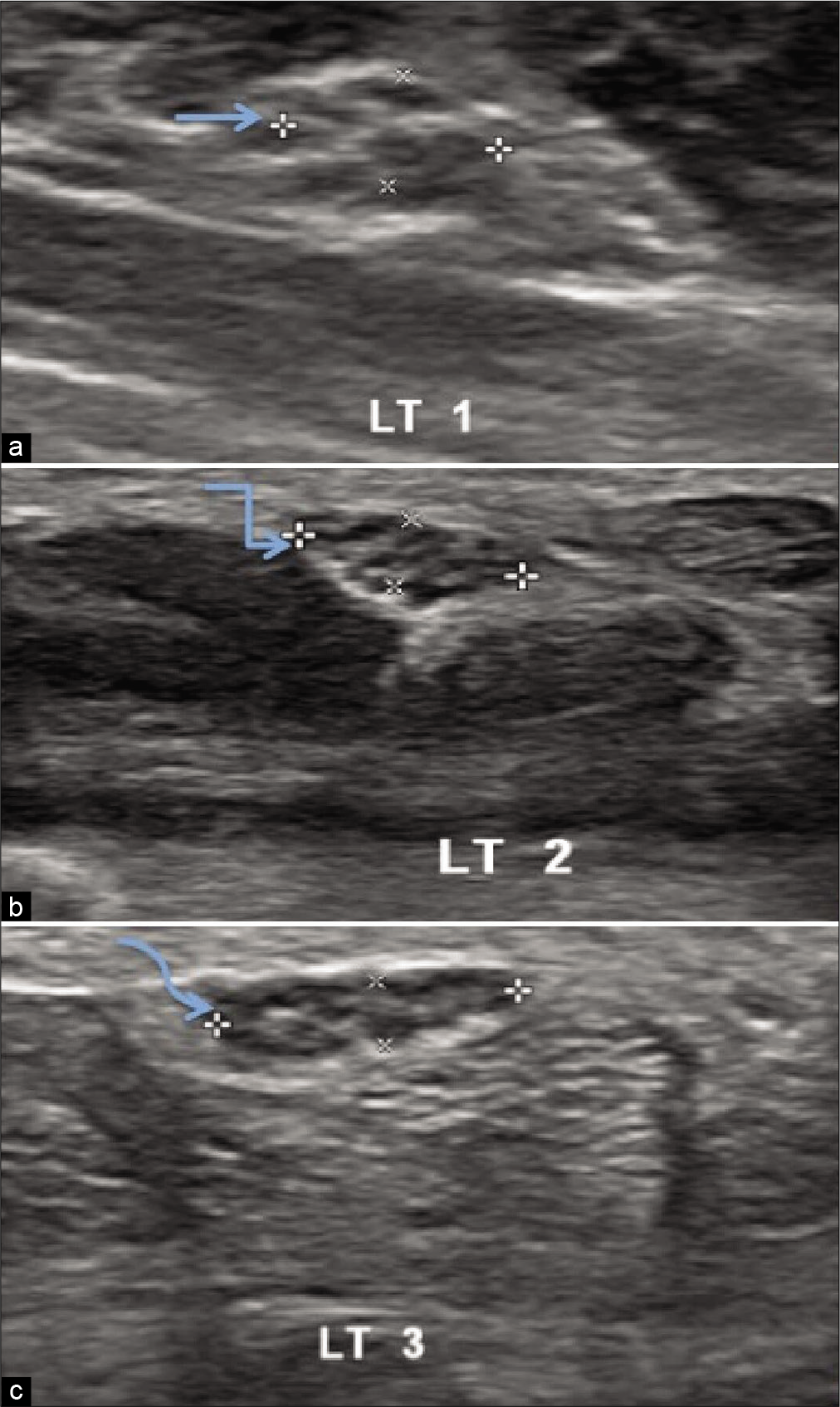
- Ultrasonography image of the flexor retinaculum of hypothyroidism patient showing (a) thickness 0.07 cm on right side(arrow) and (b) 0.052 cm on left side(arrow).
- Ultrasonography image of the left median nerve of a healthy volunteer at three levels in distal forearm showing (a) cross sectional area 0.064 cm2 at the level of pronator quadratus.(straight arrow) (b) cross sectional area 0.067 cm2 proximal to the carpal tunnel inlet.(bent arrow) (c) cross sectional area 0.069 cm2 distal to the carpal tunnel outlet.(curved arrow).
- Ultrasonography of the left median nerve of healthy volunteer showing hypoechoic median nerve fascicle thickness at three levels in distal forearm (a) Maximum thickness 0.041 cm at the level of pronator quadratus(straight arrow), (b) maximum thickness 0.050 cm proximal to carpal tunnel inlet(bent arrow), (c) maximum thickness 0.033 cm distal to carpal tunnel outlet (curved arrow).
- Ultrasonography of the left median nerve of healthy volunteer showing thickness /width ratio at three levels in distal forearm (a) thickness/width ratio 2.59 at the level of pronator quadratus,(straight arrow) (b) thickness/width ratio 3.03 proximal to carpal tunnel inlet, (bent arrow) (c) thickness/width ratio 2.89 distal to carpal tunnel outlet. (curved arrow).
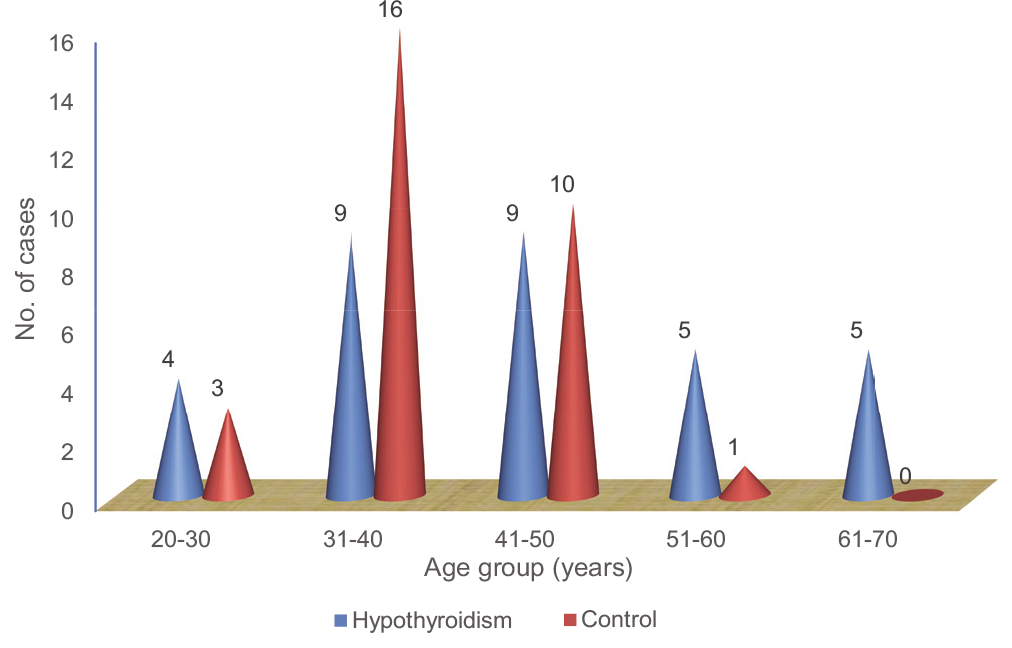
Age-wise distribution of the subjects
Our study group consisted of both male and female patients with female preponderance.
Distribution of subjects according to sex
The mean duration of disease was 29.09±19.29 years. Majority of the subjects were in the range of <24 months, as shown in Table 1.
DISCUSSION
Ultrasound is effective in confirming the diagnosis of CTS. First, other lesions that display symptoms similar to CTS may be excluded from examination, and these include tenosynovitis, mass lesions, and anatomic defects. The use of US can be recommended as the first-line method in the diagnosis of CTS.[5-7]
In our study, CSA of the median nerve has shown statistically significant at all three levels in both forearms in hypothyroid patients in correlation with healthy volunteers. Meyer et al. stated that an additional cross-sectional measurement at the distal forearm with a calculation of the difference improves the diagnostic accuracy of US.[8] Wanitwattanarumlug et al. demonstrated that a quantitative assessment of the median nerve provides an accurate diagnostic test, with an area larger than 9 mm2 being highly predictive of CTS.[9] Dana Holovacova et al. demonstrated the effect of hypothyroidism on the enlargement of the median nerve CSA.[10]
In the present study, the maximum thickness of the nerve fascicle was calculated by the largest anteroposterior dimension of the largest hypoechoic area in the short axis view of the median nerve.[11] The maximum nerve fascicle thickness and thickness/width ratio of the median nerve have not shown statistically significance in the right or left forearm in hypothyroid patients and healthy volunteers.
In the present study, the thickness of flexor retinaculum shows statistical significance in both forearms in hypothyroid patients in correlation to healthy volunteers. Hence, ultrasound is valuable for future studies to detect subtle morphological changes of the flexor retinaculum thickness in that occur in hypothyroid patients. Shen and Li also demonstrate that ultrasound is useful in the assessment of flexor retinaculum.[12]
In the present study, the diagnostic value of the inlet/outlet CSA ratio of the median nerve was evaluated in patients with hypothyroidism and healthy volunteers in both forearms. The mean value was higher in hypothyroidism patients than healthy volunteers in the right and left forearms (P = 0.009 in the right and 0.001 in the left forearm). The inlet/outlet CSA ratio of the median nerve promises to be an effective means in the diagnosis of the CTS in hypothyroidism patients. Similar results were shown in a study by Fu et al.,in which they demonstrated that the inlet/outlet CSA ratio improves the diagnostic accuracy of ultrasound for the diagnosis of CTS.[13]
In our study, we also find that the mean value of the inlet/ outlet CSA ratio of the median nerve was higher in Phalen’s test positive patients than the Phalen’s test negative patients in hypothyroidism group (P = 0.029 in the right forearm and 0.032 in the left forearm). When the inlet/outlet CSA ratio was evaluated in hypothyroidism patients in correlation with healthy volunteers, P value was 0.009 and 0.001 in the right and left forearms, respectively, which was statistically significant. Hence, ultrasonography has a superior diagnostic value compared to Phalen’s test in hypothyroidism patients.
Hence, CSA, inlet/outlet CSA of the median nerve, and thickness of flexor retinaculum in patients with hypothyroidism and healthy volunteers can be correlated. The maximum nerve fascicle thickness of median nerve and thickness/width ratio of the median nerve parameters are not of much useful parameter. Therefore, the CSA and inlet/ outlet ratio of CSA came out to be significant in Phalen’s test positive > Phalen’s test negative hypothyroid patients > healthy volunteers.
CONCLUSION
Ultrasound can be used for evaluation of the median nerve at three levels, inlet/outlet CSA ratio, and thickness of flexor retinaculum in hypothyroid patients. The high-resolution US allows direct imaging of the involved nerves, in addition to documentation of nerve shape changes that occur in compressive syndromes. It may be preferred by patients since it is easily accessible, non-invasive, shorter examination time, and of lower cost.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Ultrasonography of median nerve in carpal tunnel syndrome before and after hormone replacement in patients with hypothyroidism. Int J Radiol. 2015;2:66-71.
- [CrossRef] [Google Scholar]
- A comparison of ultrasound and MRI measurements of the cross-sectional area of the median nerve at the wrist. Hand (NY). 2018;14:746-50.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of hypothyroidism on strength-duration properties of peripheral nerve. J Neurol Sci. 2010;294:89-91.
- [CrossRef] [PubMed] [Google Scholar]
- Carpal tunnel syndrome physiology In: Encyclopaedia Britannica. United Kingdom: Encyclopædia Britannica, Inc; 2007.
- [Google Scholar]
- Ultrasonography in the evaluation of carpal tunnel syndrome: Diagnostic criteria and comparison with nerve conduction studies. Neurol Asia. 2011;16:57-64.
- [Google Scholar]
- A handy review of carpal tunnel syndrome: From anatomy to diagnosis and treatment. World J Radiol. 2014;6:284-300.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic value of median nerve ultrasonography for screening of carpal tunnel syndrome in hypothyroid patients: A cross-sectional study. Iran J Neurol. 2016;15:70-4.
- [Google Scholar]
- The median nerve at the carpal tunnel and elsewhere. J Belg Soc Radiol. 2018;102:17.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating the Cross-Sectional Area (CSA) of the Median Nerve by Use of Ultrasound in carpal tunnel syndrome (CTS) Nakhon Nayok: European Society of Radiology; 2011. p. :1-6.
- [Google Scholar]
- Cross-sectional area of the median nerve is increased in primary autoimmune hypothyroidism and decreases upon treatment with thyroxine. Eur J Endocrniol. 2016;175:265-71.
- [CrossRef] [PubMed] [Google Scholar]
- High resolution ultrasonography of the tibial nerve in diabetic peripheral neuropathy. J Ultrason. 2017;17:246-52.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound assessment of transverse carpal ligament thickness: A validity and reliability study. Ultrasound Med Biol. 2012;38:982-8.
- [CrossRef] [PubMed] [Google Scholar]
- Carpal tunnel syndrome assessment with ultrasonography: Value of inlet-to-outlet median nerve area ratio in patients versus healthy volunteers. PLoS One. 2015;10:e0116777.
- [CrossRef] [PubMed] [Google Scholar]






