Translate this page into:
Tuberculosis or Not Tuberculosis: Temporal Evolution of Patellar Tuberculosis

*Corresponding author: Suvinay Saxena, Department of Radiodiagnosis, Gujarat Imaging Center, Post Graduate Institute of Radiology and Imaging, Samved Hospital, Navrangpura, Ahmedabad - 580 034, Gujarat, India. suvinaysaxena@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saxena S, Patel P, Patel D, Shah A. Tuberculosis or Not Tuberculosis: Temporal Evolution of Patellar Tuberculosis. Indian J Musculoskelet Radiol 2020;2(1):62-5.
Abstract
Patellar tuberculosis (TB) is an uncommon occurrence and has been sparsely reported in the literature. Imaging plays a key role in its diagnosis, as clinical symptoms vary and are often unspecific. We present two cases of isolated patellar tuberculosis, its classical imaging features, and follow-up serial imaging.
Keywords
Tuberculosis
Patella
Magnetic resonance imaging
Imaging
INTRODUCTION
Osteoarticular tuberculosis accounts for 3–5% of cases of tuberculosis and 15% of extrapulmonary forms. The incidence of patellar tuberculosis is rare and has been reported sparsely in international literature ranging from 0.09% to 0.15%. Tuberculosis involving the knee has a predilection for synovial involvement with local extension eroding the adjacent bones. Isolated tuberculous patellar osteitis is rare and has been documented occasionally in reports.[1]
The clinical presentation of patellar tuberculosis is non-specific, ranging from subtle pain to mild swelling, and therefore can be a challenging diagnosis, especially during the early phase of the disease. Adolescent and young adult males are usually affected with no preceding risk factors in most occasions.[2,3]
CASE 1
A 24-year-old male presented with a history of trivial trauma and pain in the right knee joint. Initial X-rays (Figure 1, done outside) were found to be normal. The patient was referred to our hospital for magnetic resonance imaging (MRI) evaluation of the right knee joint. Institutional Ethics Committee Clearance was obtained for the case. First, MRI scan (Figure 2, dated January 11, 2018) revealed an ill-defined altered marrow signal lesion involving the patella. No evidence of synovitis, joint effusion, or articular erosions were noted. Complete blood analysis was unremarkable (Hemoglobin: 14.9 gm, and total leukocyte count 7900/cumm); but erythrocyte sedimentation rate (ESR) was on a higher side, i.e., 20 mm/h (Normal 0–10 mm/h). Findings were inconclusive and the patient was advised short interval follow-up and symptomatic treatment.

- Case 1 – X-ray: (a) Skyline view, (b) lateral projections and (c) frontal of the patella of the right knee do not reveal any significant cortical erosion or irregularity.
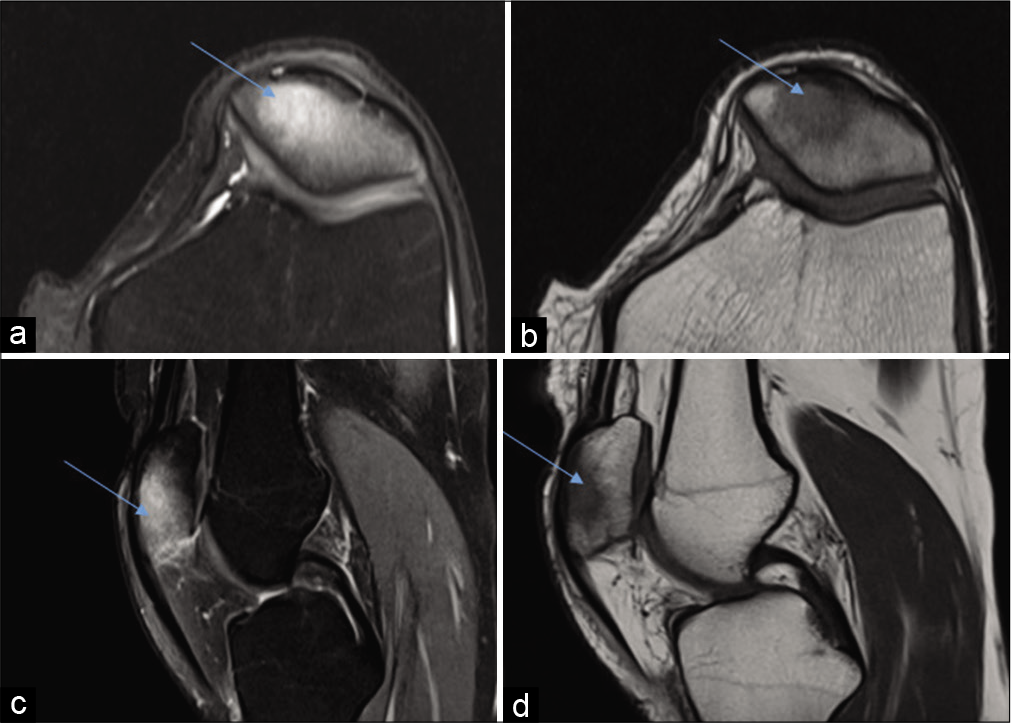
- Case 1 – Magnetic resonance imaging dated January 11, 2018 – PDFS axial (a) and sagittal (b) and sagittal (c) and images and T1 axial (d) images reveal altered marrow signal along patella which appears hyperintense on PDFS images and hypointense on T1 weighted image (arrows).
Symptoms of the patient did not resolve and the patient was subsequently referred for a repeat MRI after 3 months (Figure 3 dated March 30, 2018), which revealed further progression in edema. Computed tomography (CT) scan of the knee was performed, which revealed focal lytic lesion involving medial aspect of patella; however, no discrete sequestrum could be identified. No evidence of sclerosis. The patient was advised to arthroscopic biopsy for confirmation of diagnosis.
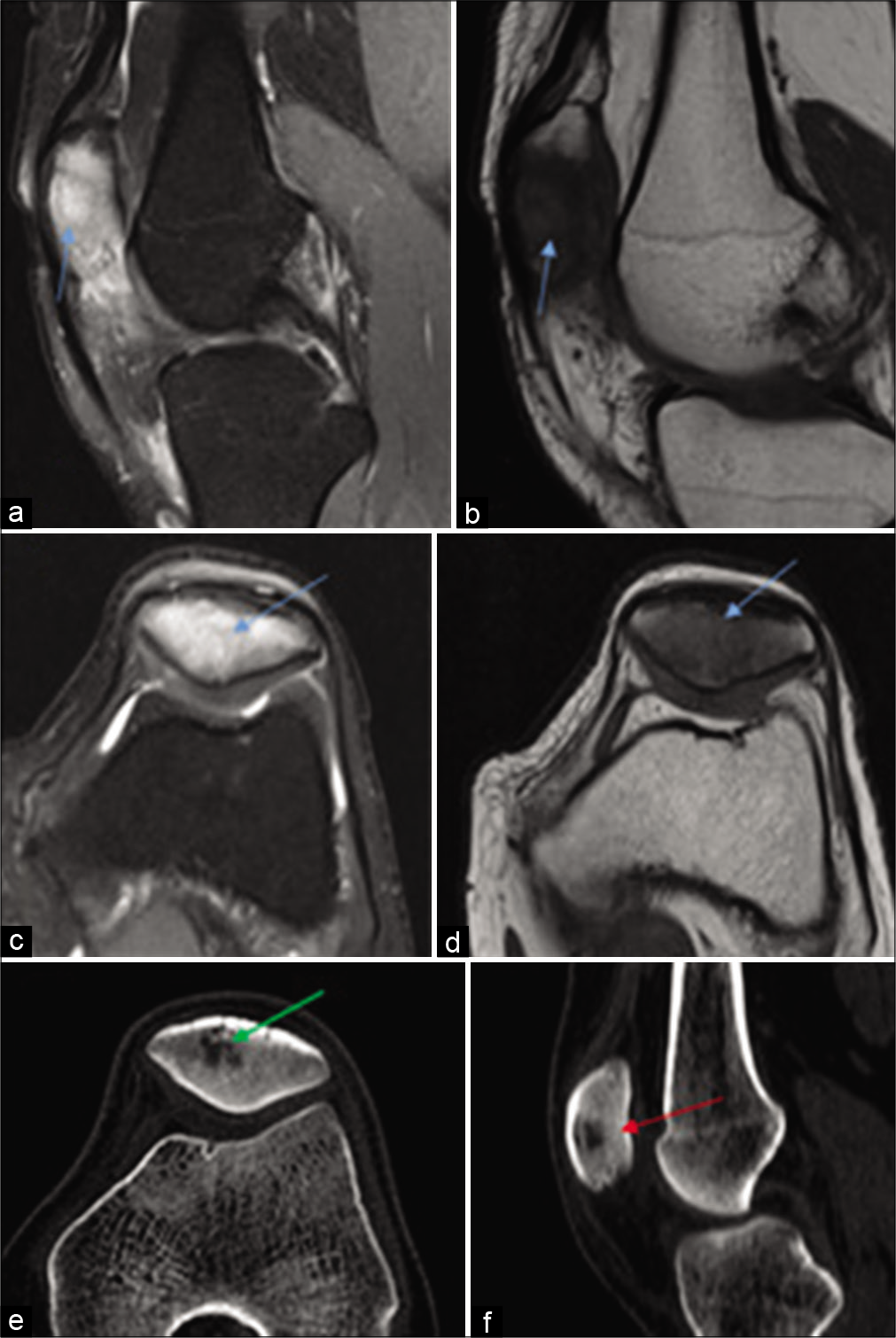
- Case 1 – Sagittal PDFS and T1 (a, b), axial PDFS (c) and T1 (d) and CT scan (bone window) axial (e) and sagittal sections (f) reveal progression, in the form of hyperintense marrow signals involving the entire patella (blue arrow a and b) and CT scan reveals the appearance of a focal lytic lesion involving the patella with fresh appearance of adjacent sclerosis (green and red arrow).
The patient was lost to follow-up and returned after 3 months and a pre-procedural MRI was again performed [Figure 4 dated June 2, 2018], which revealed an ill-defined altered signal intensity lesion involving the patella which appeared hyperintense on PDFS images, hypointense on T1 weighted image (T1WI) and showed central diffusion restriction on diffusion-weighted imaging/apparent diffusion coefficient images. The fresh appearance of a focal cortical breach was noted along medial patellar facet better appreciated on CT images, no e/o synovitis or joint effusion.
![Case 1 – Axial PDFS (a), axial T1-weighted (b), diffusion-weighted imaging and apparent diffusion coefficient (c,d), sagittal PDFS and T1-weighted (e and f) images and CT scan (bone window axial [g] and sagittal [h]) reveals the presence of an altered signal intensity focal lesion involving patella with central restriction (blue arrows), focal cortical breach along patellar facet (green arrow) seen clearly on CT images (red arrow).](/content/107/2020/2/1/img/IJMSR-2-062-g004.png)
- Case 1 – Axial PDFS (a), axial T1-weighted (b), diffusion-weighted imaging and apparent diffusion coefficient (c,d), sagittal PDFS and T1-weighted (e and f) images and CT scan (bone window axial [g] and sagittal [h]) reveals the presence of an altered signal intensity focal lesion involving patella with central restriction (blue arrows), focal cortical breach along patellar facet (green arrow) seen clearly on CT images (red arrow).
Arthroscopic biopsy and aspiration were performed which revealed the presence of Rifampicin Resistance in Mycobacterium tuberculosis on GeneXpert© test and confirmed the diagnosis of tuberculosis of patella.
CASE 2
A 30-year-old male presented with complaints of pain in the right knee joint with difficulty in walking stairs. No history of trauma or sports injury was presented. MRI [Figure 5] of the right knee joint was performed for further evaluation, which revealed a well-defined lytic lesion involving the lateral half of patella with associated chondral loss, cortical breach with coexisting synovitis along the lateral aspect of knee joint. Ultrasound-guided aspiration was performed, which revealed Acid-fast bacilli in Ziehl-Neelsen stain confirming the diagnosis of tuberculosis.
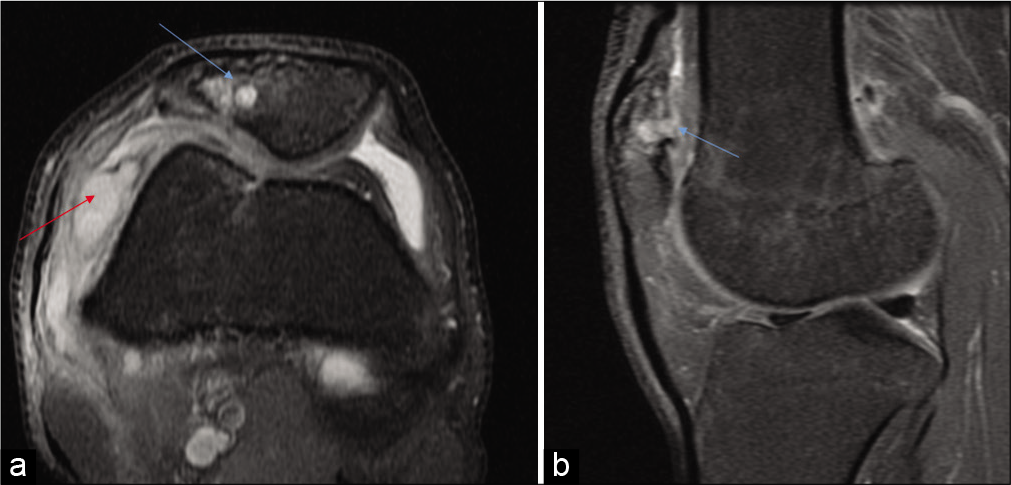
- Axial PDFS (a), sagittal (b) PDFS images reveal well defined lytic lesion involving lateral half of patella with loss of articular cartilage and breach in cortical surface (marked by red arrow). Associated changes of synovitis are apparent along the lateral aspect of the knee joint.
DISCUSSION
Tuberculosis of the knee joint is regarded as the third most commonly involved joint; however, isolated tuberculosis of patella is a rare phenomenon. It was first reported by D. Mccrae Aitken in 1933. Most of the cases have been reported in the age group of 5–15 years as the patella is predominantly cartilaginous in nature before 5 years.[1]
Common routes of infection of acquiring the infection are direct transmission following post-injury, through hematogenous route and may extend from the prepatellar bursa.[2,3]
As patellar tuberculosis is an unfamiliar and rare entity, with subtle findings on the radiograph, MRI imaging becomes essential to localize, identify, and pinpoint the diagnosis. Radiographs in initial stages can be normal, however keeping a high index of suspicion, MRI can help in the assessment of soft-tissue involvement, including bursae around knee joint, synovium, and also aid in characterizing bone involvement of patella and adjacent bones. In cases of patellar tuberculosis, MRI may depict abnormal marrow signals involving patella (hyperintense on STIR/T2W and isointense on T1W), focal altered signal intensity lesions-developing abscesses, associated synovial thickening, and rarely joint effusion. Post-contrast TIW images may reveal enhancing synovial thickening and heterogeneous enhancement of the marrow changes. There is a delayed appearance of focal lytic lesions. Sequential follow-up imaging can ascertain and aid in diagnosis.[4,5]
Imaging differentials include post-traumatic marrow edema, prepatellar bursitis, inflammatory arthritis, and crystal deposition disease.[6] Serological parameters (complete blood count and ESR) are inconclusive. Fluid aspirate for bacteriological evaluation may be equivocal, and tissue diagnosis is essential for confirmation.[7,8] CT scan can help if osteolytic or sclerotic lesions develop, which is often delayed in most of the cases and may be associated with the formation of sequestrum in chronic cases. Treatment is based on the degree of involvement, bone erosion, and associated inflammation and ranges from anti-tuberculous therapy to bone curettage and debridement.[9-11]
SUMMARY
A presumptive diagnosis of tuberculosis of patella can be surmised if MRI of knee depicts abnormal marrow signal involving the patella without history of significant trauma, synovitis or joint effusion and absence of radiographic features like cortical irregularity in patients with incognizable knee pain.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Tuberculosis of the patella. Arch Orthop Trauma Surg. 2003;123:192-4.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar tuberculosis: A case report. Orthop Traumatol. 2009;95:649-51.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis involving the patella. AJR Am J Roentgenol. 1992;159:677.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis of the patella masquerading as prepatellar bursitis. Ann R Coll Surg Engl. 2013;95:e17-9.
- [CrossRef] [PubMed] [Google Scholar]
- Extra pulmonary tuberculosis: Rapid identification of Mycobacterium tuberculosis and simultaneous detection of rifampicin resistance by genexpert assay. Int J Contemp Microbiol. 2018;4:31-7.
- [CrossRef] [Google Scholar]
- Tuberculosis of the knee: A case report and literature review. Joints. 2017;5:180-3.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculous synovitis of the knee in a 65-year-old man. Vojnosanit Pregl. 2009;66:1019-22.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar tuberculosis presenting as an osteolytic lesion. J Postgrad Med Educ Res. 2013;47:221-2.
- [CrossRef] [Google Scholar]






