Translate this page into:
Extraskeletal Osteosarcoma of Colon Mimicking Carcinoma of Colon – A Rare Entity

*Corresponding author: Dr. Birma Ram, Department of Radiodiagnosis, Command Hospital Kolkata, Kolkata, West Bengal - 700 027, India. innovativehooda@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Ram B, Sharma P, Gopinath M, Singh SK. Extraskeletal osteosarcoma of colon mimicking carcinoma of colon – A rare entity. Indian J Musculoskelet Radiol 2020;2(1):73-6.
Abstract
Extraskeletal osteosarcoma is a rare malignant mesenchymal tumor which typically affects elderly patients and the commonly affected sites are extremities, retroperitoneum, mesentery, and trunk. Extraskeletal osteosarcoma arising from colon or retroperitoneum can manifest as a large mass with features of intestinal or urinary tract obstruction. Local recurrence after excision and distant metastasis are common, so regular follow-up and surveillance of such patients are advisable after excision of the primary tumor.
Keywords
Extraskeletal osteosarcoma
Contrast-enhanced computed tomography
Mineralization/Calcification
Osteoid matrix
Immunohistochemistry
INTRODUCTION
Osteogenic osteosarcoma is the most common primary malignant bone tumor in young adults. The extraskeletal variety is, however, not so common but is histologically indistinguishable from osteogenic osteosarcoma.[1]
Extraskeletal osteosarcoma is a rare malignant mesenchymal soft-tissue neoplasm without any obvious osseous involvement. It accounts for 1% of soft-tissue sarcomas and 4% of osteogenic osteosarcoma.[1,2] Wilson in 1941 first described the extraskeletal osteosarcoma.[3] Later, Fine and Stout in 1956 suggested that it may show behavior similar to primary osteogenic osteosarcoma in bone.[4] Subsequent studies have elucidated that extraskeletal osteosarcoma should be considered clinically and therapeutically separate from osteogenic osteosarcoma.
Extraskeletal osteosarcomas usually affect elderly population in the 5th–7th decades with a slight male preponderance.[1,5] The commonly involved sites are thigh, upper extremities, retroperitoneum mesentery, mediastinum, omentum, and trunk.[6]
CASE REPORT
We present a rare case of extraskeletal osteosarcoma of colon in a 62-year-old male patient who presented with features of intestinal obstruction. On further enquiry, the patient had intermittent abdominal pain for 3 months and loss of appetite for 2 months. Abdominal pain was insidious in onset and gradually progressive in nature, localized to the epigastrium and left hypochondrium. It was associated with nausea which aggravated after taking meals. There was no history of fever, chills, vomiting, hematuria, hematemesis, or per rectal bleeding. There was no history of any antecedent trauma or any other comorbidities. Physical examination revealed a large firm abdominal mass in the left lumbar region.
Ultrasound of the abdomen had shown aperistaltic large bowel loops with an ill-defined hypoechoic mass in the left lumbar region, extending into the left iliac fossa with multiple hyperechoic foci showing posterior shadowing suggestive of calcification. Mild ascites was also present.
Computed tomography (CT) scanogram revealed an ill- defined soft-tissue mass in the left lumbar region with areas of coarse calcifications and dilated large bowel loops [Figure 1].
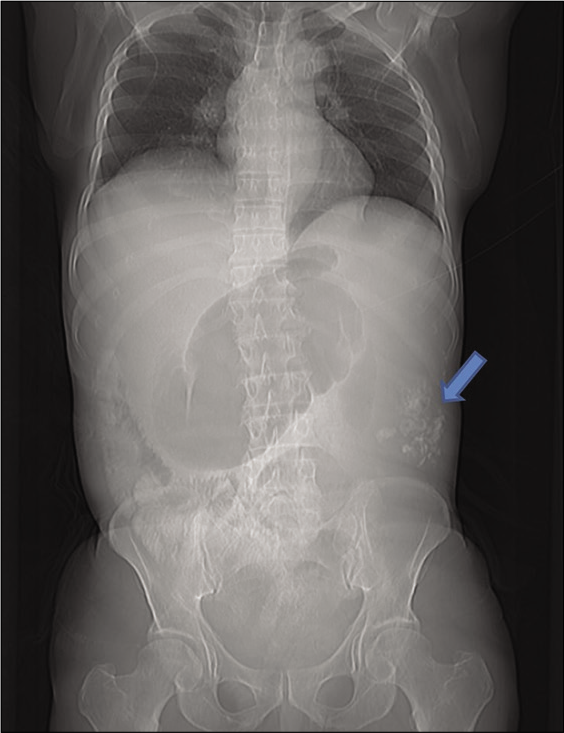
- Scanogram suggestive of foci of coarse calcifications (arrow) is the left lumbar region with dilated bowel loops proximally and absent bowel gas shadow in the pelvis.
Contrast-enhanced CT (CECT) of the abdomen with oral and IV contrast revealed large, irregularly marginated, lobulated exophytic soft-tissue density mass measuring 12 (anteroposterior) × 16 (transverse) × 18 (craniocaudal) cm adjacent to the descending colon with indistinct intervening fat planes, causing significant luminal compression. Multiple non-enhancing areas consistent with necrosis were noted within. Multiple coarse calcifications (likely osteoid matrix) were noted within the mass lesion [Figures 1 and 2]. Superiorly, the mass was extending up to the splenic flexure, displacing the spleen medially. Inferiorly, it was extending in the left iliac fossa [Figure 3]. Posteriorly, the mass was closely abutting the psoas muscle with maintained fat planes. Inferomedially, the mass was infiltrating into the mesentery and causing nodular thickening of the mesentery forming a heterogeneous mass. Ascending and TR colon were dilated. Moderate ascites was present. Based on imaging characteristics and clinical profile, provisional diagnosis was given as malignant growth of descending colon with differential diagnosis of extraskeletal osteosarcoma.

- Contrast-enhanced computed tomography of chest, abdomen, and pelvis suggestive of well-defined heterogeneously enhancing mass with coarse calcifications in the left lumbar region and extending into the left iliac fossa and causing mass effect by displacing the spleen medially and near complete luminal compression of the splenic flexure and descending colon causing dilatation of the large bowel loops proximally.

- Coronal and sagittal representative sections showing extent of the mass, distal part of the descending colon is partially collapsed (shown by arrow in right image), and cystic areas in the superior aspect of the mass in the image on the left.
The blood and biochemical investigations were within normal limits. Serum alanine aminotransferase, aspartate aminotransferase, and alkaline phosphatase were 14, 16, and 103 IU, respectively. Tumor markers, carcinoembryonic antigen and carbohydrate antigen 19- 9, were 2.37 and 19.9 U/ml, respectively. The patient was taken up for exploratory laparotomy. A large exophytic mass was encountered with extension into the lower pole of spleen along with a mesenteric lymph nodal mass. The mass was excised in toto and sent for histopathological examination (HPE).
Pathological examination of the specimen revealed large exophytic mass arising from the serosa of the descending colon. On cut sections, it was heterogeneous in gross appearance with cystic areas and foci of bone within. Sections of the descending colon revealed tumor arising from subserosa and composed predominately of malignant spindle-shaped cells arranged in fascicles, whorls, and storiform pattern at places. These cells were markedly pleomorphic, having high nuclear cytoplasmic ratio (N: C ratio) with irregular nuclear contour, vesicular chromatin, and prominent nucleoli. Multinucleated and atypical bizarre cells interspersed in a fibrocollagenous background with myxoid changes and hyalinization at places. Osseous metaplasia was noted in the form of thin lacy and thick trabecular osteoid deposition with atypical osteoid cells within. Foci of necrosis and hemorrhage were also evident. Multiple tumor deposits were noted in the mesocolon. On immunohistochemistry, the tumor was immunopositive for vimentin and immunonegative for CD117, CD34, epithelial membrane antigen, desmin, myogenin, CD68, calretinin, S100, HMB-45, and leukocyte common antigen. HPE features were diagnostic of malignant mesenchymal neoplastic mass, extraskeletal osteosarcoma [Figure 4].[6]
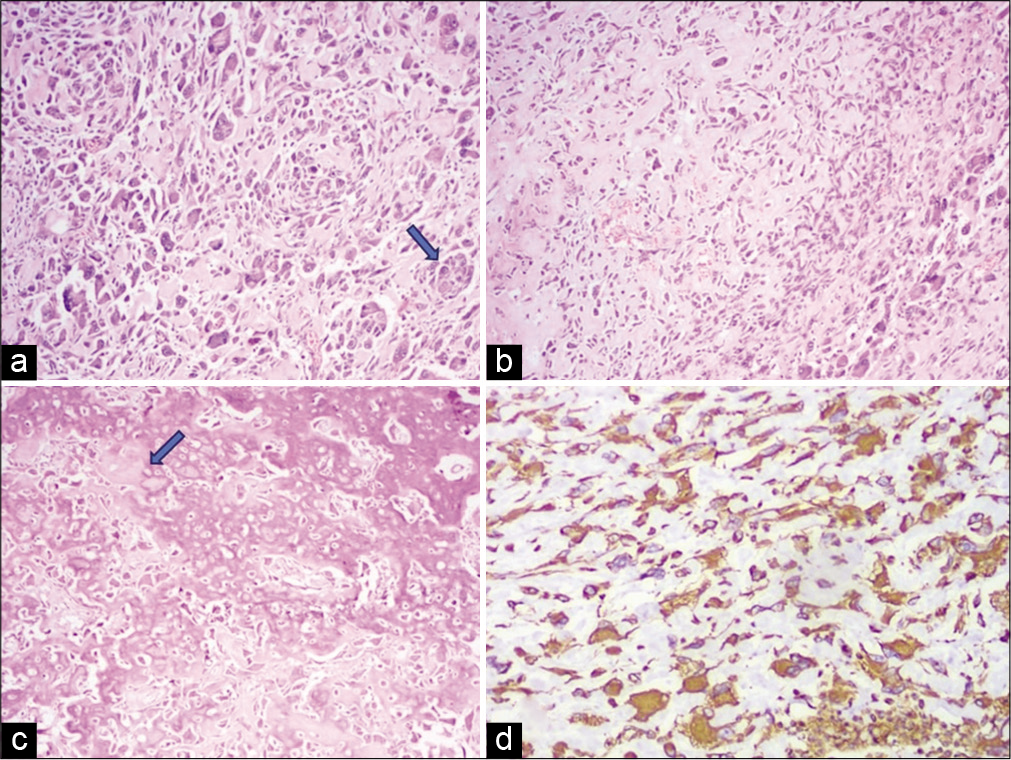
- Histopathological examination images of the resected mass – hematoxylin and eosin stain, Image a (20×) and Image b (10×) showing malignant pleomorphic bizarre cells (shown by arrow) with intervening areas of dense hyalinized fibrocollagenous stroma and osteoid material. Image c is showing malignant osteoid cells laying in the form of lacy and thick trabecular osteoid material with hyperchromatic atypical cells within. Image d on immunohistochemistry the cells was immunopositive for vimentin and immunonegative for CD117, CD34, epithelial membrane antigen, desmin, myogenin, CD68, calretinin, S100, HMB-45, and leukocyte common antigen.
DISCUSSION
Extraskeletal osteosarcomas generally affect the elderly population in contrast to conventional osteosarcoma which affects the younger individuals in the age group of 20– 30 years.[1] Typical presentation is a slow-growing firm mass with or without pain.
Chung and Enzinger in a retrospective study of 88 patients of extraskeletal osteosarcomas revealed that it affects predominantly elderly patients, older than 50 years with slight male preponderance.[7] The tumor manifested mainly as a soft-tissue mass in the extremities, with a predilection for the thighs (lower extremity, 46.6%; upper extremity, 20.5%) and the retroperitoneum (17%). Most of the patients presented with an insidiously growing mass with minimal pain or tenderness.
Extraskeletal osteosarcomas typically show a heterogeneous soft-tissue mass with necrosis and variable amounts of coarse and amorphous calcifications similar to osteoid matrix. CECT shows heterogeneous enhancement due to necrosis, mineralization, and hypervascularity of the mass. Osteoid matrix or mineralization can be seen in approximately 50% of patients with primary lesion and can appear during course of the disease progression. On cross-sectional imaging, tumors generally show a pseudocapsule and appear separate from the adjacent bony structures.[1,2]
On magnetic resonance imaging (MRI), the tumor typically appears as a well-circumscribed heterogeneous mass, isointense to the skeletal muscle on T1 weighted (T1 WI) and iso to mildly hyperintense on T2 weighted (T2 WI). Hemorrhage and necrosis are quite common, giving it a heterogeneous appearance on cross-sectional imaging. Hemorrhage may appear hyperintense on T1 and T2 WI and shows blooming on susceptibility sequences. Excessive hemorrhage within the mass may mimic a hematoma.[8]
Differential diagnosis of such a mass includes number of benign and malignant pathologies. Benign non- neoplastic conditions include old calcified hematoma, myositis ossificans, and foreign body granulomas. Benign conditions are typically associated with a history of prior surgery or antecedent trauma.[9] Myositis ossification characteristically shows zoning phenomena which means gradual mineralization from periphery to the center, whereas extraskeletal osteosarcoma shows reversed zoning phenomenon with dense calcification in the center compared to the periphery of the lesion.[5,10]
Neoplastic (benign) mass lesions of retroperitoneum include teratomas, vascular lesions like hemangioma, and neurogenic tumors such as schwannoma and paragangliomas. The malignant calcified mass includes undifferentiated pleomorphic sarcomas (previously known as malignant fibrous histiocytoma), mesenchymal sarcomas, liposarcomas, extraskeletal chondrosarcoma, and extraskeletal osteosarcoma.
Local recurrence after excision and distant metastasis is common and accounts for approximately 90% of cases with an interval up to 10 years from primary tumor detection and treatment.[7]
Summary
Extraskeletal osteosarcoma is rare mesenchymal tumor which typically affects elderly patients. The commonly affected sites are extremities (particularly thigh region), retroperitoneum, mesentery, colon, and trunk. Extraskeletal osteosarcoma of colon can manifest with features of intestinal or urinary obstruction. Typical imaging characteristics of tumor are that of a heterogeneous mass with osteoid matrix or coarse mineralization. MRI is advisable with such imaging characteristics on CECT for better tissue characterization and proper extent of the mass as well as to look for skip lesions or distant metastasis.[8]
As per available literature, overall prognosis is poor. Local recurrence after excision and distant metastasis in patients with extraskeletal osteosarcomas are common, so regular follow-up and surveillance of such patients are advisable after excision of the primary tumor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Extraskeletal osteosarcoma: Spectrum of imaging findings. AJR Am J Roentgenol. 2012;198:W31-7.
- [CrossRef] [PubMed] [Google Scholar]
- Osteogenic sarcoma of the somatic soft tissues. Clinicopathologic study of 26 cases and review of literature. Cancer. 1971;27:1121-33.
- [CrossRef] [Google Scholar]
- Osteogenic sarcoma of the extraskeletal soft tissues. Cancer. 1956;9:1027-43.
- [CrossRef] [Google Scholar]
- A review of 40 patients with extraskeletal osteosarcoma. Cancer. 1995;76:2253-9.
- [CrossRef] [Google Scholar]
- Enzinger and Weiss's Soft Tissue Tumors (6th ed). Philadelphia, PA: Saunders; 2013.
- [Google Scholar]
- Retroperitoneal extraskeletal osteosarcoma: CT and MR imaging of a case report. J Radiol Sci. 2013;38:139-42.
- [Google Scholar]
- Retroperitoneal extraskeletal osteosarcoma. AJR Am J Roentgenol. 1990;155:1139-40.
- [CrossRef] [PubMed] [Google Scholar]






