Translate this page into:
USG-guided Hydrodissection for Recurrent Ulnar Neuropathy in a Patient with Anteriorly Transposed Nerve

*Corresponding author: Aakanksha Agarwal, Department of Radiodiagnosis, SMS Hospital, JLN Marg, Jaipur - 302 004, Rajasthan, India. a.agarwal.1992@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jhanwar V, Agarwal A, Chandra A, Bagarhatta M. USG-guided Hydrodissection for Recurrent Ulnar Neuropathy in a Patient with Anteriorly Transposed Nerve. Indian J Musculoskelet Radiol 2020;2(2):125-7.
Abstract
Imaging of peripheral nerves by ultrasound has come into vogue with availability of higher frequency linear transducers and variable sizes of footprints allowing better spatial resolution. Hydrodissection is a novel technique which was elaborated in the literature, not long ago, in 2008. This case report elaborates hydrodissection done for a patient with recurrent symptoms of ulnar neuropathy 4 years after anterior transposition of the nerve. Ultrasound-guided perineural injections of saline and steroid were given 2 months apart and the patient was followed up for 6 months thereafter. Ultrasound-guided hydrodissection technique has gained significant attention in the recent times but it still lacks large studies or trials to validate its safety, establish guidelines on techniques and solutions, thus necessitating exploration in this field.
Keywords
Hydrodissection
Neuropathy
Neuropathic pain
Ultrasound-guided procedure
INTRODUCTION
With wide availability of ultrasound and accompanying technical advancements, ultrasound evaluation of nerves is becoming commonplace.[1] Ultrasound helps to identify the exact site, possible type, and etiology of nerve injury. Compressive neuropathies are the most common cause of nerve pathology in adults, with post-operative adhesions being a major cause of surgical failure.[2,3] Adhesions can develop due to intraoperative nerve injury, excessive bleeding or postoperative scarring. Secondary surgical neurolysis along with nerve exploration is the conventional procedure done for suspected neural adhesions. Hydrodissection is a novel technique which employs instillation of anesthetic or solution such as saline or 5% dextrose solution to separate the nerve from the surrounding tissue, fascia, or adjacent structures. Conventionally, this technique has been used for dissecting myofascial planes in surgeries and remove adhesions by creating non-existent surgical planes. With regard to its use in neuropathic pain, Smith et al.[4] described their experience with hydrodissection in the management of carpal tunnel syndrome (CTS). We describe the case of a patient with recurrent pain along the distribution of ulnar nerve 4 years after anterior transposition of the nerve done for the same indication.
CASE REPORT
A 28-year-old male patient presented with complaints of pain and numbness along the medial aspect of his right forearm radiating into the medial one and a half digits. The pain was fairly constant throughout the day with numbness leading to a discomforting sleep. On examination, there was no loss of motor or sensory function with a strength of 5/5 in flexors and lumbricals of the hand. The patient gave a score of 9 to his pain on visual assessment score (VAS) card. He had a history of anterior transposition of ulnar nerve of the right arm done for similar complaints 4 years back and was reluctant for a repeat surgery.
On ultrasound evaluation of the nerve, the ulnar nerve was transposed anteriorly and intramuscularly. The nerve was of normal fascicular architecture with a caliber of 2 mm in distal arm. At the site of anterior transposition, the nerve was mildly hypoechoic and had a caliber of 3.4 mm [Figure 1] suggestive of focal neuropathic change consistent with axonotmesis.[5] As the patient was apprehensive for a repeat surgical procedure, he was offered ultrasound guided hydrodissection. After taking his consent, hydrodissection of the nerve was carried out under complete asepsis. The patient was made to lie in a right lateral position allowing the affected right arm to lie on his side which was then draped with a sterile surgical sheet. Following a thorough local site cleansing with betadine and alcohol swab, 4–5 mL local anesthetic agent (2% lignocaine) was instilled in the skin at the pre-determined site corresponding to the site of focal nerve thickening. A 25-gauge 2 inch needle was used with a 5 mL syringe. The solution used was 1 mL of 40 mg/mL methylprednisolone with 4 mL of 0.9% saline. By an in-plane approach, fluid was instilled all around the ulnar epineurium separating it from the surrounding soft tissue, as evident by a thin hypoechoic layer of fluid all around the nerve [Figures 2-4].[5] Care was taken to ensure no damage to the nerve by the needle.
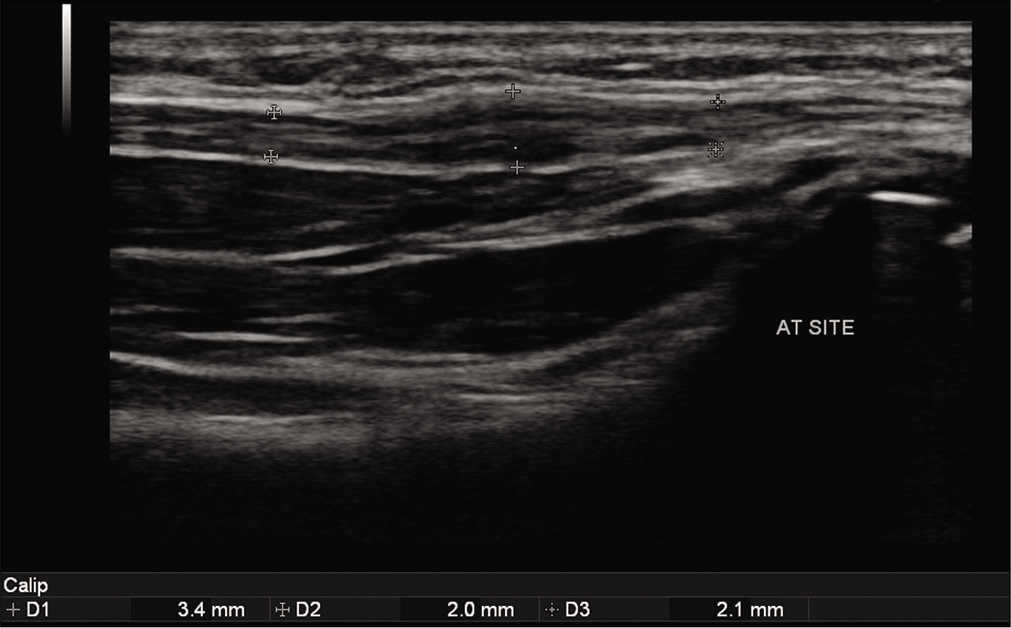
- Gray scale ultrasound image showing thickened hypoechoic ulnar nerve measuring 3.4 mm (between calipers) at the site of anterior transposition. Proximally and distally, the nerve is normal and measures 2.0 mm and 2.1 mm, respectively.
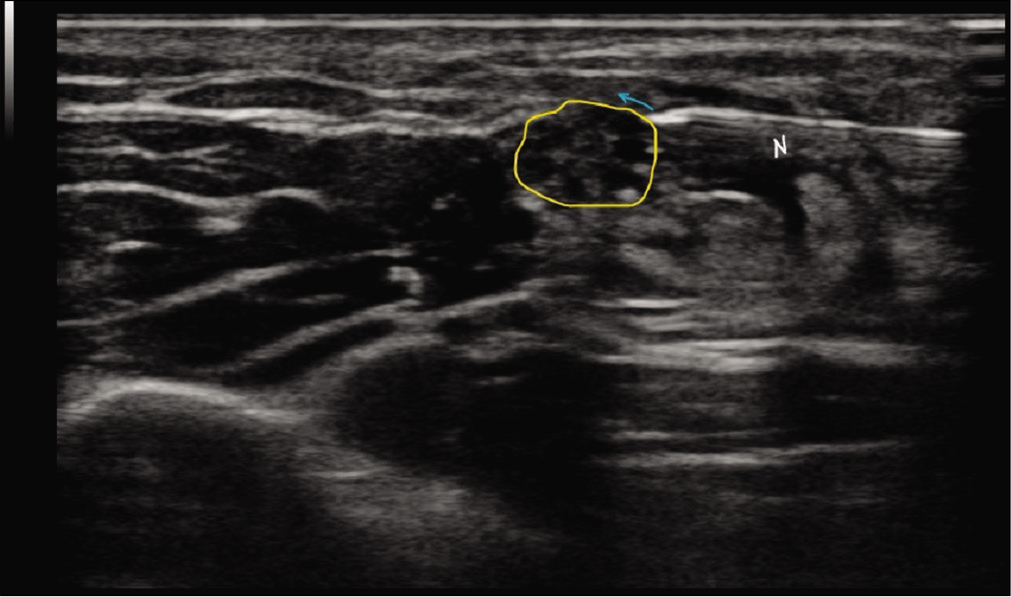
- Transverse section of the nerve at the site of pathology (outlined in yellow) showing the needle (N) in place just before injecting the solution. The blue arrow depicts the projected trajectory of the solution in a bevel up position.
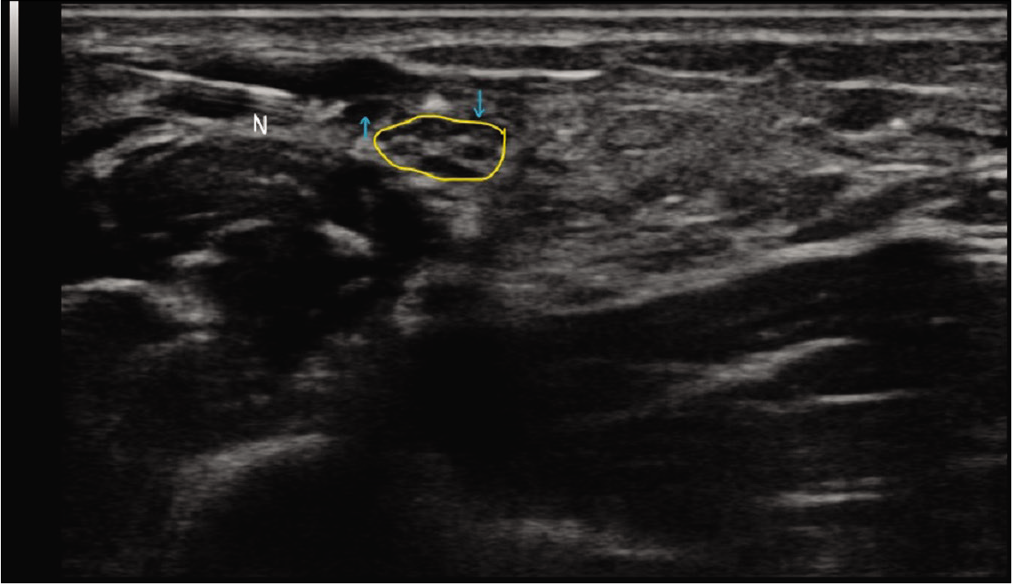
- Transverse section of the nerve at the site of pathology (outlined in yellow) showing the needle (N) and the injected solution (blue arrows) as an anechoic sliver of fluid around the nerve epineurium.
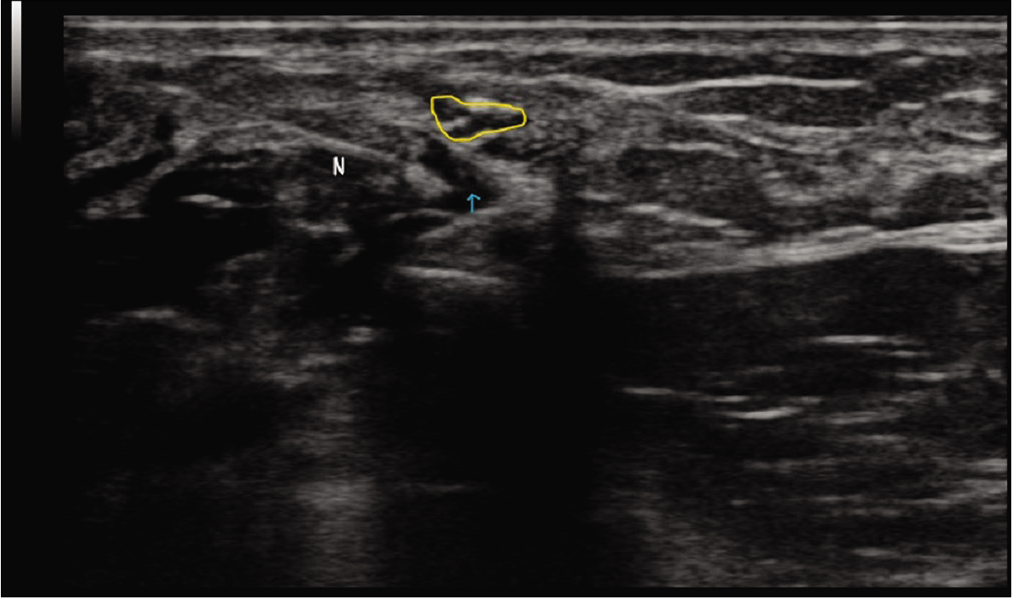
- Transverse section of the nerve at the site of pathology (outlined in yellow) showing the needle (N) and the injected solution (blue arrow) below the nerve, thus separating it from the surrounding tissues from all sides.
The patient was immediately relieved of his symptoms with no loss of motor/sensory function of the ulnar nerve with transient tingling along the ulnar nerve distribution. On follow-up at 1 month, the patient had unwavering improvement in his symptoms with an improvement of VAS score from 9 to 7. Another injection of 3–4 mL saline without steroid was given in a similar manner after discussion with the referring orthopedic surgeon and the patient was kept on follow-up.
At 6 months follow-up, the patient has a VAS score of 5 with considerable improvement in his symptoms. He has mild discomfort only on heavy weight lifting but is otherwise free of pain and there is no complaint of numbness/tingling during sleep.
DISCUSSION
A detailed description of the technique of hydrodissection of peripheral nerves was given by Smith et al.[4] for CTS. Kim et al.[6] described the utility of hydrodissection in cadaveric ulnar nerves to dissect it from soft tissues in the cubital tunnel. Another study of hydrodissection on 10 patients with cubital tunnel syndrome was carried out by Choi et al.[7] which resulted in significant improvement with no neurological injuries.
Our patient was not a case of cubital tunnel syndrome as he was operated for a similar indication with anterior transposition of ulnar nerve and presented with recurrent symptoms postoperatively. The postulated cause for his recurring symptom seems to be post-operative perineural adhesions at the site of transposition as evident by focal thickening at the site of transposition.
We used a combination of steroids and 0.9% saline in the first setting followed by 0.9% saline alone in the next sitting. Literature review displays certain articles like those by Wu et al.[8] which propose the use of 5% dextrose in hydrodissection of median nerve in patients with CTS with promising results. DeLea et al.[9] used 3 mL of 1% lidocaine for hydrodissection of carpal tunnel in patients with scleroderma. Malone et al.[10] treated 44 wrists with CTS by hydrodissection using 9 cc of sterile saline, 1 cc of 1% lidocaine, and 1 cc of 40 mg/ml triamcinolone acetonide.
Experience with varied solutions is limited with available literature limited to case reports and small group studies, warranting further research in this field. The choice of the solution remains an institutional preference with no set guidelines at present.
CONCLUSION
Hydrodissection is a low cost, minimally invasive technique for discomforting neuropathic symptoms. It is highly accurate under ultrasound guidance with no or minimal transient neurological injury under experienced hands requiring basic infrastructure. However, as this technique is relatively new, there are no published guidelines on the technique and solutions to be used in specific clinical settings. Literature review did not reveal any large-scale studies of this technique, thus warranting further extensive research in this field.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Can imaging be the new yardstick for diagnosing peripheral neuropathy? A comparison between high resolution ultrasound and MR neurography with an approach to diagnosis. Insights Imaging. 2019;10:104.
- [CrossRef] [PubMed] [Google Scholar]
- Intraneural tissue reactions induced by internal neurolysis. An experimental study on the blood-nerve barrier connective tissues and nerve fibres of rabbit tibial nerve. Scand J Plast Reconstr Surg. 1976;10:3-8.
- [CrossRef] [PubMed] [Google Scholar]
- The nerve lesion in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1976;39:615-26.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographically guided carpal tunnel injections: The ulnar approach. J Ultrasound Med. 2008;27:1485-90.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging in the diagnosis of ulnar nerve pathologies-a neoteric approach. Insights Imaging. 2019;10:37.
- [CrossRef] [PubMed] [Google Scholar]
- Real-time visualization of ultrasonography guided cubital tunnel injection: A cadaveric study. Ann Rehabil Med. 2012;36:496-500.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical implications of real-time visualized ultrasound-guided injection for the treatment of ulnar neuropathy at the elbow: A pilot study. Ann Rehabil Med. 2015;39:176-82.
- [CrossRef] [PubMed] [Google Scholar]
- Nerve hydrodissection for carpal tunnel syndrome: A prospective, randomized, double-blind, controlled trial. Muscle Nerve. 2019;59:174-80.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographically guided hydrodissection and corticosteroid injection for scleroderma hand. Clin Rheumatol. 2011;30:805-13.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided percutaneous injection, hydrodissection, and fenestration for carpal tunnel syndrome: Description of a new technique. J Appl Res. 2010;10:116-23.
- [Google Scholar]






