Translate this page into:
Traumatic Musculocutaneous Nerve Injury Diagnosed Using High-Resolution Ultrasonography

*Corresponding author: Jatinder Pal Singh, Department of Radiology, Medanta-The Medicity, Gurugram - 122 001, Haryana, India. sinjatin@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ghosh S, Nischal N, Singh H, Singh JP. Traumatic Musculocutaneous Nerve Injury Diagnosed Using High-Resolution Ultrasonography. Indian J Musculoskelet Radiol 2020;2(2):149-51.
Abstract
Peripheral nerve pathology may occur due to a number of causes. Physicians rely primarily on the information gained by the non-anatomical tests such as clinical examination, neurophysiological testing, and on clinical history for evaluation and management of peripheral nerve pathologies. Magnetic resonance imaging (MRI) is a favored investigation for the evaluation of peripheral nerve pathologies among the clinicians. We report a case of a traumatic injury to the musculocutaneous nerve causing weakness in elbow flexion, with normal imaging on MRI but diagnosis being made using high-resolution ultrasonography, following which the Oberlin nerve transfer procedure was undertaken, leading to resolution of muscle weakness post-procedure.
Keywords
Magnetic resonance imaging
High-resolution ultrasound
Musculocutaneous nerve
Trauma
Injury
INTRODUCTION
Peripheral nerve pathology may occur due to a number of causes, of which traumatic nerve injury remains a major one, often leading to residual disability, pain, or sensory loss. The diagnostic modalities for peripheral neuropathies include thorough physical examination and neurophysiological testing, but its accuracy may be influenced by factors such as age and body mass index.[1] Imaging methods often provide a more direct visualization of peripheral nerve pathology. Magnetic resonance imaging (MRI) is a favored investigation for the evaluation of peripheral nerve pathologies among the clinicians. High-resolution ultrasonography (HRUS) reveals the status of innervated musculature, localization of disease pathology, and recognition of the extent of nerve damage.[2,3] HRUS has the advantage for easier availability, maneuvrability, dynamic, low cost, and real-time imaging of a nerve along its course. Here, we report the case of a traumatic injury to the musculocutaneous nerve causing weakness in elbow flexion, with normal imaging on MRI but diagnosis being made using HRUS, following which the Oberlin nerve transfer procedure[4] was undertaken, leading to resolution of muscle weakness post-procedure. This case highlights the utility of HRUS as a sensitive modality to diagnose peripheral nerve injuries.
CASE REPORT
A 26-year-old female presented to the emergency department after a road traffic accident, with multiple lacerations on her arm and trunk. However, her main complaint was the inability to lift her right upper limb, with associated decreased sensation in the lateral aspect of her right forearm. MRI of her right brachial plexus was done the next day, which was normal, and plain radiographs revealed no fractures. Repairs for her lacerations were done, but she was otherwise managed conservatively, with physiotherapy and analgesics. Her muscle weakness improved gradually, and at 3 months, she had complete recovery of muscle power in the right upper limb apart from flexion of elbow in supination. She was pronating the forearm and flexing the elbow, suggestive of the use of her brachioradialis muscle [Video 1 (please visit the article in HTML to watch the video at https://dx.doi.org/10.25259/ IJMSR_23_2020)]. At this point, HRUS was performed on her right arm [Figure 1a], positioning the ultrasonography (USG) transducer transverse to the axillary artery with the arm in abducted position, which revealed selective injury to the muscular branches of the musculocutaneous nerve within the coracobrachialis [Figure 1b and c], supplying the biceps and brachialis muscles. USG revealed the loss of normal fascicular pattern, and a diagnosis of right musculocutaneous nerve injury was made.
Video 1:
Video 1:Video shows patient pronating the forearm and flexing the elbow, suggestive of the use of her brachioradialis muscle. (https://dx.doi.org/10.25259/IJMSR_23_2020).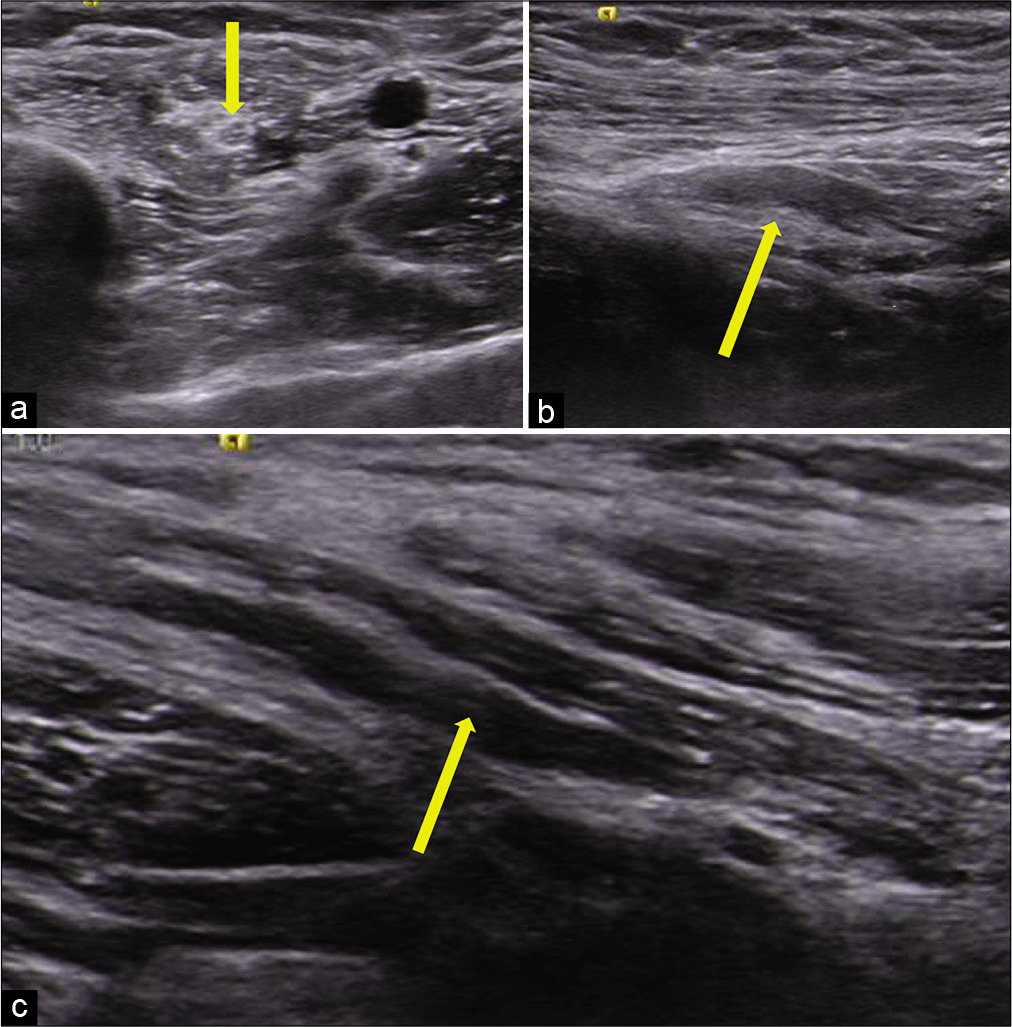
- High-resolution ultrasonography of the right arm reveals (a) normal intramuscular portion of musculocutaneous nerve (arrow) within the coracobrachialis. (b and c) Selective injury to the muscular branch of the musculocutaneous nerve, supplying the biceps and brachialis muscles with thickening of nerve and loss of normal fascicular pattern (arrow).
She then underwent the Oberlin nerve transfer procedure, in which one of the fascicles each from median and ulnar nerve was coapted with the nerves to biceps and brachialis, and had a very good recovery in the coming months and by 7 months, she was able to lift a weight of around 1 kg while flexing the elbow in supination [Video 2 (please visit the article in HTML to watch the video at https://dx.doi.org/10.25259/IJMSR_23_2020)]. This is a rare case of selective injury to the muscular branches of the musculocutaneous nerve, not involving other nerves of brachial plexus, picked up very nicely by HRUS.
Video 2:
Video 2:Video shows very good recovery and the patient was able to lift a weight of around 1 kg while flexing the elbow in supination. (https://dx.doi.org/10.25259/IJMSR_23_2020).DISCUSSION
The musculocutaneous nerve is a branch of the lateral cord of the brachial plexus, supplying the coracobrachialis, biceps brachii, and brachialis muscles, with the main function being forearm flexion at the elbow. The supination component of the forearm is aided by the brachioradialis, supplied by the radial nerve. Isolated musculocutaneous nerve injury has less associated disability than that of any other major upper extremity nerve injury and is a rare condition, leading mainly to weakness of elbow flexion with pain and numbness along the lateral forearm.
The use of sonography to detect peripheral nerve lesions dates as far back as 1988, when Fornage first described the normal echoanatomy of the peripheral nerves.[5] Since then, the use of HRUS, combined with clinical experience, has allowed the use of USG as an effective method to diagnose peripheral nerve pathologies. On long-axis images in USG, nerves show narrow, elongated structures with a fascicular appearance due to alternating hypoechoic and hyperechoic bands that represent the fascicles (including the perineurium). On histological examination, the hypoechoic areas corresponded to the neuronal fascicles. USG has a high negative predictive value in excluding structural nerve damage.[6] High-resolution sonography has also been useful in the evaluation of brachial plexus and traumatic peripheral nerve pathologies.[7,8]
Our case highlights the importance of sonography for detecting peripheral nerve pathology, in cases undiagnosed on MRI. This happened because the MRI was performed only of the Brachial plexus, as requested by the clinician and it missed the musculocutaneous nerve injury that was located in proximal portion of the arm and was not included in the field of view of MR scan. More interesting from the patient’s point of view, of course, is the fact that this led to the subsequent nerve transfer procedure. A common and successful nerve transfer is the classical Oberlin procedure[4] to restore elbow flexion, which in this case was modified as the “double” Oberlin nerve transfer, taking a fascicle each from the ulnar and the median nerves, and innervating the biceps brachii.
The timely intervention for this patient, leading to recovery of flexion of her elbow (as documented in the videos [please visit the article in HTML to watch the video at https://dx.doi.org/10.25259/Cytojournal_31_2020]), was dependent on the accurate sonographic diagnosis of musculocutaneous nerve pathology that went undiagnosed on MRI scanning. This makes it an interesting case in the domain of radiology, with HRUS assisting a successful nerve transfer in a young female.
CONCLUSION
HRUS is a powerful problem-solving tool that may be used for evaluation of peripheral nerve pathologies, in cases where MRI may have failed to diagnose the problem.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on:
References
- Individual attributes versus composite scores of nerve conduction abnormality: Sensitivity, reproducibility, and concordance with impairment. Muscle Nerve. 2003;27:202-10.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonography of the peripheral nervous system. Perspect Med. 2012;1:417-21.
- [CrossRef] [Google Scholar]
- Ultrasound of the peripheral nerves. Joint Bone Spine. 2008;75:643-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: Anatomical study and report of four cases. J Hand Surg Am. 1994;19:232-7.
- [CrossRef] [Google Scholar]
- Peripheral nerves of the extremities: Imaging with US. Radiology. 1988;167:179-82.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical validation of high-resolution ultrasonography in detection of missed tendon and nerve injuries after penetrating wounds of hand and wrist. Turk Plast. 2020;28:44-50.
- [Google Scholar]
- Sonographic evaluation of brachial plexus pathology. Eur Radiol. 2004;14:193-200.
- [CrossRef] [PubMed] [Google Scholar]
- High Resolution ultrasound in the evaluation and management of traumatic peripheral nerve injuries: Review of the literature. Oman Med J. 2014;29:314-9.
- [CrossRef] [PubMed] [Google Scholar]






