Translate this page into:
Ultrasound acting as a guiding light in the diagnosis of posterior interosseous nerve entrapment at ligament of Frohse – A case report

*Corresponding author: Isha Gupta, Department of Radiology, Xpert’s Imaging and Diagnostic Clinic, Jaipur, Rajasthan, India. ishagupta2707@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta I, Jhanwar V. Ultrasound acting as a guiding light in the diagnosis of posterior interosseous nerve entrapment at ligament of Frohse – A case report Indian J Musculoskelet Radiol. 2024;6:111-5. doi: 10.25259/IJMSR_60_2023
Abstract
Posterior interosseous nerve (PIN) entrapment syndrome is a relatively rare compression neuropathy which leads to weakness of the extensor muscles of hand. This becomes a cause of morbidity to the patient with resultant difficulty in conducting day-to-day activities. Thickening of proximal edge of the superficial head of the supinator muscle which forms the ligament of Frohse can lead to compression of the PIN as it enters the supinator canal. Although nerve conduction studies can indicate the diagnosis, they cannot identify the exact site and cause of compression which is crucial for deciding the further management. Magnetic resonance imaging can identify the cause of entrapment in some cases; however, this is extremely difficult given the small size of the PIN and arcade of Frohse. Ultrasound overcomes these limitations and provides a cost and time effective, efficient, and sensitive diagnostic tool for detecting nerve entrapment. Here, we would like to emphasize the emerging importance of ultrasound by describing a case of ligament of Frohse thickening causing PIN entrapment which was effectively diagnosed by ultrasound and confirmed on surgical exploration, treated with surgical ligament release with a full recovery.
Keywords
Posterior interosseous nerve
Ligament of Frohse
Nerve entrapment
Nerve swelling
Ultrasound
INTRODUCTION
The posterior interosseous nerve (PIN) is the deep branch of the radial nerve in forearm which provides motor supply to the extensor muscles of the hand.[1] Radial nerve passes anterior to the lateral epicondyle of the humerus after exiting from the spiral groove, and then bifurcates into a superficial sensory branch and a deep motor branch called the PIN at the level of the radio-capitellar joint.[1] Entrapment of PIN as it passes between the two heads of the supinator muscle at the level of the elbow leads to PIN syndrome, which presents as weakness or paralysis of the digital and thumb extensor muscles without any sensory symptoms in the affected digits.[2] The causes of PIN syndrome may include intrinsic nerve abnormalities such as tumors or extrinsic compression due to a myriad of reasons.[2] Thickening of the arcade of Frohse, which is the fibrous semicircular arch at the entry of the supinator tunnel, is the most common cause of compressive neuropathy of the PIN and occurs at the site of its entry into the supinator tunnel.[1] Ultrasound imaging can help localize the site of compression as well as the cause and can help detect the thickening of ligament of Frohse which is very difficult to detect on magnetic resonance imaging (MRI) due to its small size. Ultrasound also allows comparison with the opposite normal site which increases its sensitivity. We present a case report of PIN syndrome due to entrapment at the entrance of supinator tunnel from a thickened ligament of Frohse- with clinical history, local examination, sonographic findings, and surgical correlation.
CASE REPORT
A 22-year-old woman presented with gradually progressive weakness in extension of all fingers and thumb of the right upper extremity for 6 months. She also complained of pain along the lateral aspect of proximal forearm. She did not complain of any other sensory abnormality or paresthesias in the involved digits. There was no history of trauma, infection, diabetes, or any neuromuscular disorders.
At physical examination, there was decrease in power of extension of all the digits and abduction of thumb; however, the bulk of muscles appeared normal. Flexion movements were normal, with normal reflexes and no sensory abnormality. Nerve conduction studies revealed motor neuropathy along the radial nerve and normal conduction velocities along the median and ulnar nerves.
High-resolution ultrasound examination was performed using hockey stick probe and revealed thickening of the ligament of Frohse which is formed by the superior edge of superficial head of supinator muscle [Figure 1]. The ligament was seen as an echogenic thickened band crossing anterior to the PIN in transverse plane. It measured 1.1 mm on the affected side and 0.4 mm on the normal side [Figure 2]. Furthermore, there was an abrupt change in the diameter of the PIN with focal swelling of the nerve proximal to its passage through the supinator tunnel [Figure 1]. The nerve also appeared hypoechoic at this level. However, no increase in internal vascularity of nerve was noted on color Doppler examination [Figure 3]. On comparing with the normal side, the diameter of the nerve was increased on the affected site. No discontinuity of fibers of PIN was noted and there was no evidence of any other external compressive lesion. The main radial nerve and its superficial branch were normal along their entire course.
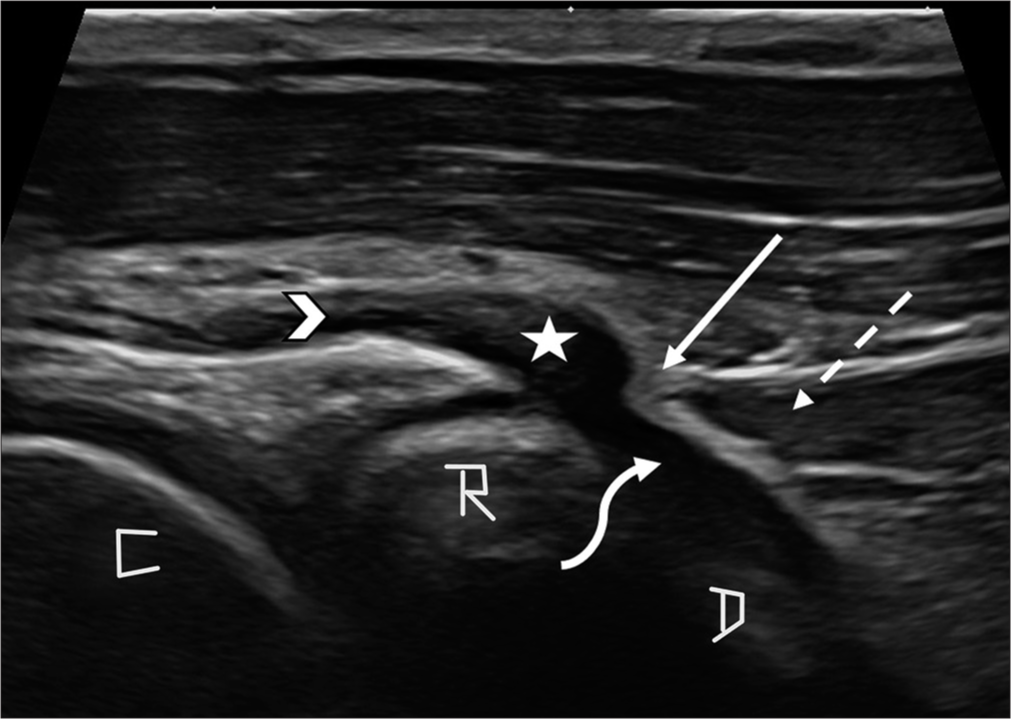
- Sagittal ultrasound scan at the level of proximal forearm showed focal swelling of the posterior interosseous nerve (star), proximal to the superior edge of superficial head of supinator muscle (dashed arrow). The nerve was normal in diameter proximal (arrowhead) and distal (curved arrow) to this location. Echogenic thickening of Ligament of Frohse (solid arrow) was also noted. C: Capitellum, D: Deep head of supinator muscle, R: Radius head.
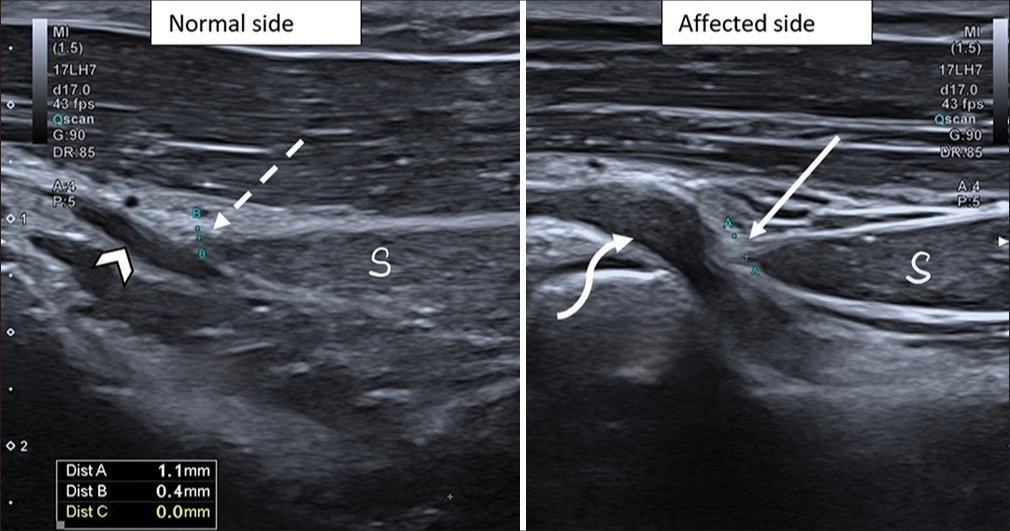
- Comparative sagittal ultrasound scan of bilateral forearms at the level of entry of supinator tunnel was performed – the posterior interosseous nerve appeared significantly thickened on the affected side (curved arrow) in comparison to the contralateral normal side (arrowhead).Thickness of the ligament of Frohse was compared – it measured 0.4 mm on the normal side (dashed arrow) but was significantly thickened on the affected side and measured 1.1 mm (solid arrow). S: Superficial head of supinator muscle.
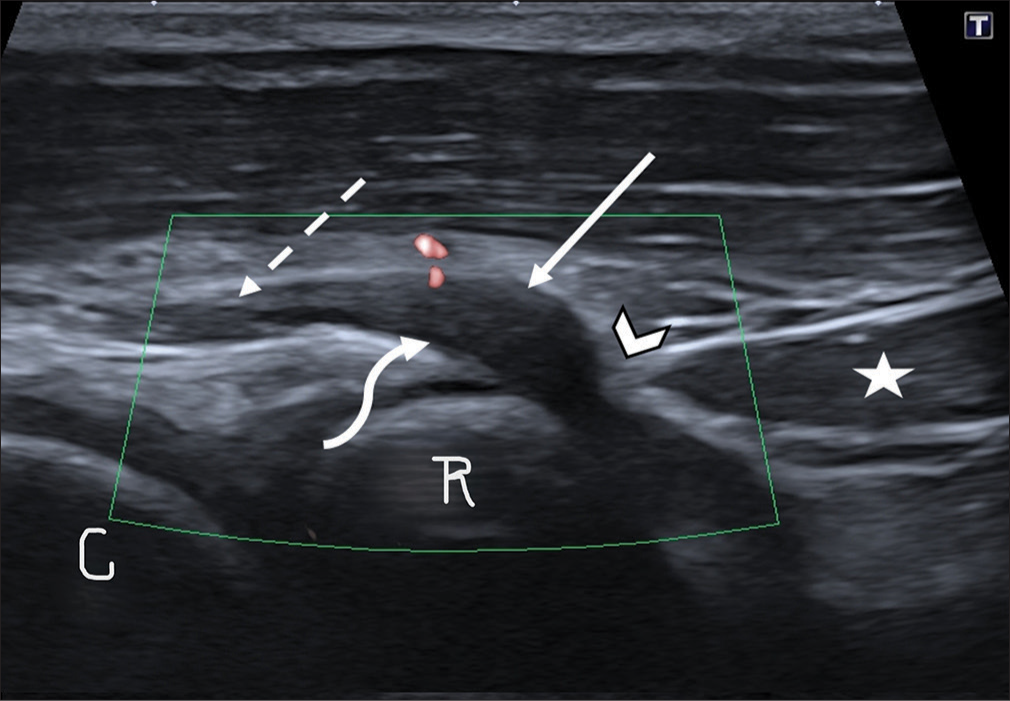
- Ultrasound examination revealed a hypoechoic posterior interosseous nerve at the site of focal swelling (solid arrow), just proximal to the site of compression by ligament of Frohse (arrowhead). No increase in internal vascularity of nerve was noted on color Doppler examination (curved arrow). Normal echogenicity and diameter of nerve were noted proximal to the site of swelling (dashed arrow). Star: Superficial head of supinator muscle, C: Capitellum, R: Radius head.
At surgical exploration, the supinator muscle was identified and a thickened fibrous band – the ligament of Frohse, was found compressing the nerve, crossing anteriorly and obliquely to the nerve causing focal swelling of PIN proximally. There was no additional compression. The fibrous band was then surgically released. The patient was followed up with weekly ultrasound examinations which showed progressive decrease in the diameter of the PIN on the affected side which reached to 0.6 mm at the end of 1 month which was very close to the diameter on the normal side (0.4 mm). This correlated with clinical improvement and partial return of motor functions 1 week after surgical decompression and almost full recovery after 1 month.
DISCUSSION
PIN entrapment is a rare neuropathy with a very low incidence of about 0.03%.[3] The radial nerve bifurcates into a superficial sensory branch and a deep motor branch called the PIN which passes between the superficial and deep heads of the supinator muscle along the lateral antebrachial region, just distal to the cubital fossa.[3] PIN branches to supply the finger and thumb extensors, extensor carpi ulnaris, and the abductor pollicis longus muscles. PIN syndrome is an entrapment of the PIN just distal to the elbow joint, which may result in paresis or paralysis of the digital and thumb extensor muscles.[2] PIN syndrome can occur due to intrinsic nerve abnormalities or structures/lesions causing extrinsic nerve compression and imaging plays an important role to localize and characterize these abnormalities.[2]
PIN can be compressed at five extrinsic locations [Figure 4] – most proximal being the fibrous band of the radial head, followed by the radial recurrent vessels, referred to as the leash of Henry at the level of the radial neck.[1] The third location is marked by the tendinous margin of the extensor carpi radialis brevis muscle. The thickened proximal edge of supinator muscle also called the arcade of Frohse forms the fourth point. The most distal location is compression at the distal margin of the supinator muscle.[1] Other space-occupying lesions such as – Ganglion cysts, lipoma, and radial head fracture, may also cause compression of the PIN.[4] Repetitive supination and pronation movements, as has been reported in swimmers, Frisbee players, tennis players, violinists, etc., can also cause chronic stress on PIN and lead to PIN syndrome.[2]
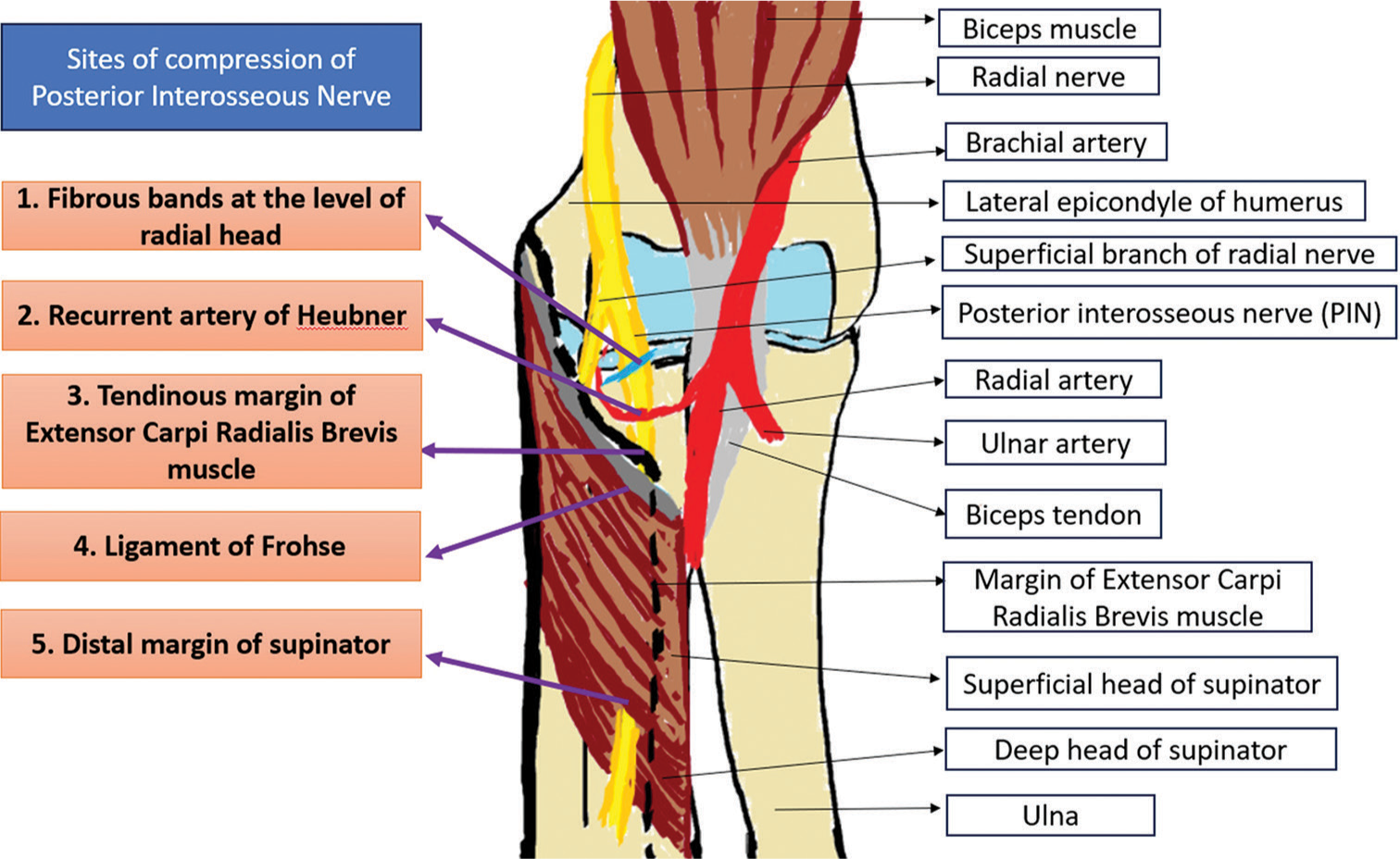
- Schematic diagram showing the possible sites of compression of posterior interosseous nerve around the elbow joint.
Patient with PIN syndrome presents with weakness in the extension of the fingers, pain along lateral aspect of proximal forearm which may or may not be associated with atrophy of the forearm muscles.[1] This manifests as an inability to extend the metacarpophalangeal joints of the finger and thumb with weakness of thumb extension at the interphalangeal joint. Wrist extension is usually preserved due to radial nerve innervation of the extensor carpi radialis longus proximal to the origin of PIN.[3] Repetitive pronation and supination of the forearm can cause aggravation of symptoms caused by compression of PIN by arcade of Frohse.[5] Although nerve conduction studies and clinical examination may indicate the diagnosis of PIN syndrome, they cannot identify the cause, for which ultrasound plays a crucial role.
The arcade of Frohse which is the thickened proximal edge of the superficial head of supinator muscle is the most common site of extrinsic compression of PIN.[1] The two forearm supinator muscle layers, superficial and deep, form the supinator canal and the fibrous semicircular arch formed at its entrance is called “the arcade of Frohse.”[6]
To identify the PIN on ultrasound, one must trace the radial nerve in the spiral groove on posterior aspect of humerus or deeper to the brachioradialis muscle.[2] Distally, it bifurcates into superficial and deep branches and the deep branch passes through the supinator tunnel and continues as the PIN. Similar anatomic landmarks are used on MRI.[2]
On sonography, normal peripheral nerves show hypoechoic nerve fascicles and hyperechoic connective tissue.[7] In the transverse plane, a peripheral nerve has a speckled appearance also called the honeycomb appearance and is relatively hyperechoic compared with surrounding muscle. In the longitudinal plane, a peripheral nerve exhibits a linear fascicular appearance resembling a bundle of cords.[2] An increase in diameter of PIN with hypoechoic changes compared to more proximal aspect of the nerve or the contralateral nerve at the same level suggests presence of swelling which is commonly seen proximal to the site of compression.[1]
Ligament of Frohse is seen as the echogenic superior margin of the superficial head of the supinator muscle on ultrasound examination. Its thickening may be noted in PIN entrapment cases when comparing with the opposite normal side. Sonography can also detect space-occupying lesions such as lipomas or ganglion cysts causing nerve entrapment or intrinsic nerve abnormalities like peripheral nerve sheath tumors.[8] In the latter cases, the mass is seen in continuity with the peripheral nerve, which indicates origin from the nerve itself rather than an adjacent extrinsic mass.[2]
Denervation atrophy of a muscle can be visualized as a diffuse hyperechoic or mixed echogenic change of a muscle echotexture on ultrasound. Loss of perineural fat, which is normally seen as a thin hyperechoic layer circumferentially surrounding the PIN, can make the nerve prone to compression.[1]
Although nerve conduction studies can help diagnose nerve entrapment syndromes, they lack spatial information and cannot identify the cause of entrapment, which can be done with ultrasonography (USG).[1] Other benefits of ultrasound include – lower cost, ease of repeatability, comparison to contralateral side can be done, wide availability, etc. Due to these benefits, USG has become the initial imaging modality for pathologies involving the peripheral nerves.[1] Another pitfall is that abnormal activity on electromyography may be missed in cases studied earlier than 3 weeks or after more than 12 weeks of onset of neuropathy.[9] Ultrasound can identify the cases of PIN entrapment that fall in this window period.[1]
MRI can also be used for identifying cases with PIN entrapment, but this can be challenging given the small size of the PIN and arcade of Frohse.[3] Often, muscle atrophy involving abductor pollicis longus and extensor muscles of digits such as – extensor digiti minimi, extensor indicis, extensor pollicis brevis, extensor carpi ulnaris, extensor digitorum, and extensor pollicis longus is the most detected finding on MRI.[6] Other findings which may be detected on MRI include focal thickening of the affected segment of the nerve with bright signal on T2-weighted sequence.[3]
Identifying the cause of PIN entrapment is as important as making the diagnosis of presence of entrapment, as surgical release of the nerve from the site of entrapment by ligament of Frohse can relieve the patient from his symptoms and facilitate rapid recovery of motor symptoms, as seen in our case. USG can also be used to monitor the recovery after surgery which can be seen as decrease in swelling of the nerve. Advances in interventional radiology have made it possible to use non-surgical, USG-guided nerve hydrodissection to relieve compression of PIN by ligament of Frohse by creating a sleeve of fluid around the nerve using ultrasound-guided injection.
CONCLUSION
PIN syndrome is a rare neuropathy which occurs due to compression of the motor branch of radial nerve. Although nerve conduction studies can identify the presence of compression, they cannot identify the etiology. Ultrasound can effectively identify the intrinsic and extrinsic nerve abnormalities and guide further management, as seen in our case. We conclude that sonography, with its wide availability, high spatial resolution, lack of ionizing radiation, control of the imaging plane of orientation, and easy applicability can act as an effective tool for the diagnosis of PIN syndrome.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ultrasonographic findings of posterior interosseous nerve syndrome. Ultrasonography. 2017;36:363-9.
- [CrossRef] [PubMed] [Google Scholar]
- Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. Am J Roentgenol. 2003;181:219-21.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior interosseous nerve entrapment-an uncommon entity. 2022. Eurorad. Available from: https://www.eurorad.org/case/17960 [Last accessed on 2023 Nov 01]
- [Google Scholar]
- The two locations of ganglions causing radial nerve palsy. J Hand Surg Eur Vol. 2007;32:341-5.
- [CrossRef] [PubMed] [Google Scholar]
- Frohse's arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. 2009;95:114-8.
- [CrossRef] [PubMed] [Google Scholar]
- The arcade of Frohse: A systematic review and meta-analysis. Surg Radiol Anat. 2021;43:703-11.
- [CrossRef] [PubMed] [Google Scholar]
- Echotexture of peripheral nerves: Correlation between US and histologic findings and criteria to differentiate tendons. Radiology. 1995;197:291-6.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic appearances of nerve tumors. J Clin Ultrasound. 1999;27:363-8.
- [CrossRef] [Google Scholar]
- Mononeuropathies of the radial nerve: Clinical and neurographic findings in 91 consecutive cases. J Electromyogr Kinesiol. 2005;15:377-83.
- [CrossRef] [PubMed] [Google Scholar]






