Translate this page into:
Magnetic resonance imaging in post-operative hip: Navigating the “Forbidden” landscape

*Corresponding author: Stanzin Spalkit, Department of Radiodiagnosis and Interventional Radiology, All India Institute of Medical Sciences, New Delhi, India. stanzn156@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Spalkit S, Pilania K, Chari R, Gupta A. Magnetic resonance imaging in post-operative hip: Navigating the “Forbidden” landscape. Indian J Musculoskelet Radiol. 2025;7:119-29. doi: 10.25259/IJMSR_3_2025
Abstract
The rising incidence of hip arthroplasty procedures, combined with demographic trends and concerns over metal-on-metal implant complications, has created an urgent need for accurate diagnostic methods for patients with hip replacements. While conventional radiography remains the initial investigation of choice, it often fails to detect or accurately assess the full extent of complications. Magnetic resonance imaging (MRI) has emerged as a vital diagnostic tool in post-arthroplasty evaluation, particularly through advances in conventional pulse sequences and metal artifact reduction techniques that enable better visualization of bone structures, implant-tissue interfaces, and surrounding soft tissues. This imaging modality effectively identifies various post-arthroplasty complications, including stress reactions and fractures, aseptic loosening and bone resorption, inflammatory responses to polyethylene wear, adverse local tissue reactions to metal debris, infections, and neuromuscular complications, which will be reviewed in this article. The enhanced capabilities of MRI with these optimized techniques provide crucial information that guides diagnosis, prognostic assessment, risk evaluation, and surgical planning, making it an indispensable tool in the post-arthroplasty care pathway.
Keywords
Complications
Hip replacement
Magnetic resonance imaging
Metal suppression
Post-operative hip
INTRODUCTION
Total hip arthroplasty (THA) has become the standard treatment for end-stage hip disease, providing pain relief and functional improvement in approximately 90% of patients. Its main indications include osteoarthritis, acute fractures, osteonecrosis of the femoral head, and hip dysplasia. However, post-operative groin and thigh pain affects up to 40% of patients, and despite advances in implant design, fixation techniques, and bearing materials, all implants eventually fail.[1] The increasing frequency of primary arthroplasty procedures and their performance in younger patients has led to a rise in revision surgeries, creating a greater need for accurate pre-operative diagnostic capabilities.[2]
Imaging in THA patients serves multiple purposes: Routine surveillance for complications, evaluation of symptomatic patients, guidance for interventional procedures, and pre-operative planning. Traditional imaging modalities, including conventional radiography, nuclear scintigraphy, arthrography, and computed tomography (CT), remain valuable but are limited by poor soft-tissue contrast, lower specificity, and cumulative radiation exposure during longitudinal follow-up. Magnetic resonance imaging (MRI) offers superior soft-tissue contrast and multiplanar capabilities without ionizing radiation, though metallic implants pose significant challenges requiring specialized techniques.[3]
This review aims to discuss MRI strategies for hip arthroplasty implants, including optimized conventional pulse sequences and metal artifact reduction techniques, review normal post-arthroplasty appearances, and illustrate the spectrum of complications and failure modes that can be evaluated using MRI.
TECHNICAL CONSIDERATIONS IN POSTOPERATIVE HIP MRI
Susceptibility artifacts
MRI has traditionally been considered to be of limited use in the presence of metallic implants due to susceptibility artifacts generated by the implant. Magnetic susceptibility is the tendency of a substance to become magnetized on exposure to an external magnetic field. The proportion of magnetization depends on the applied magnetic field (B0) and the susceptibility constant of the material within the magnetic field.[4]
Metallic implants create imaging artifacts due to the significant difference in magnetic susceptibility between the prosthetic components and surrounding human tissue. This susceptibility mismatch distorts the local magnetic field, causing two main effects: First, it alters the normal precessional frequencies of nearby protons, leading to spatial misregistration of signals, particularly in the frequency- and slice-encoding directions. This results in characteristic areas of signal void surrounded by regions of abnormally high-signal intensity, often called “signal pileup.”[5] Second, the field distortion causes accelerated dephasing of protons in tissues adjacent to the implant, resulting in signal loss in these regions. These artifacts are most prominent in the frequency-encoding direction and can significantly distort the appearance of surrounding anatomical structures.[4]
Impact of implant materials and geometry
The material composition of implants plays a crucial role, with increasing artifact severity observed from titanium (least) to cobalt-chromium to stainless steel (most). Implant geometry also significantly impacts artifact production – the curved surface of acetabular components generates more field inhomogeneity and, consequently, more artifacts compared to the relatively linear surface of femoral components. While ferromagnetic and paramagnetic materials cause substantial susceptibility artifacts, ceramic and polyethylene components produce minimal artifacts due to their favorable magnetic properties.[6]
Metal artifact reduction strategies
Table 1 compiles the various factors and parameter modifications needed to reduce metal artifacts.[7]
| Methods to reduce metal artifacts in MRI | ||
|---|---|---|
| 1. | Field Strength Selection | Utilize 1.5T rather than 3T imaging systems |
| 2 | Implant Orientation | Align implant’s long axis parallel to main magnetic field (B0) and frequency encoding direction |
| 3 | Sequence Selection | Prefer FSE sequences with long echo train length and short TE over GRE |
| 4 | Parameter Optimization | •Increase receiver bandwidth •Maximize matrix size • Optimize NEX |
| 5 | Geometric Parameters | • Minimize FOV • Reduce slice thickness |
| 6 | Fat Suppression Techniques | Favor STIR and Dixon-based methods over frequency-selective fat suppression |
FSE: Fast spin echo, GRE: Gradient echo, NEX: Number of excitations, FOV: Field of view, MRI: Magnetic resonance imaging, TE: Time to echo, STIR: Short tau inversion recovery
Metal artifact reduction sequences (MARS)
Figure 1 demonstrates how conventional MRI is limited by significant metal artifacts from prosthetic components, which obscure anatomical details. In contrast, MARS MRI provides enhanced visualization of the acetabulum and surrounding soft tissues by minimizing these artifacts, allowing for better clinical assessment of periprosthetic structures.Various MRI vendors offer different specialized MARS techniques, few examples are provided below.
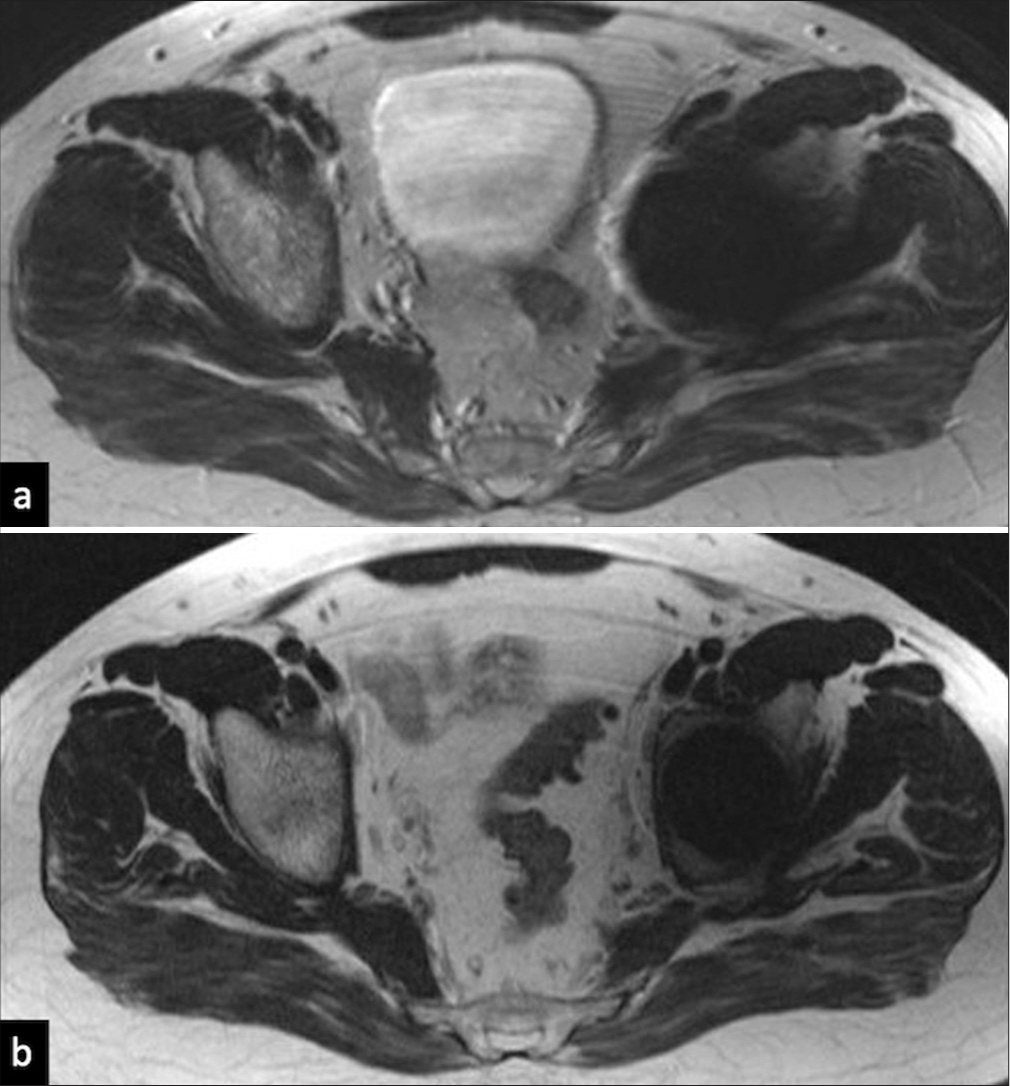
- MRI without and with metal artefact reduction sequence (MARS). (a) Axial T2 image without MARS: metallic artifact causing marked hypointensity around the prosthesis causing obscuration of the left hip joint and the adjacent soft tissue, (b) Axial T2 MARS MRI (showing improved visualization of the acetabulum as well as the surrounding soft tissue.
Multi-acquisition variable resonance image combination
It splits the imaging volume into multiple frequency bins to capture off-resonance signals caused by metal, then combines them into a final image. It also enables 3D imaging with isotropic resolution.[5]
Slice encoding for metal artifact correction
It corrects slice distortions through additional encoding, aligning displaced slices caused by metal. It is suitable for large implants.[8]
View angle tilting
It tilts the readout gradient to reduce in-plane distortions by aligning with the magnetic field inhomogeneity. It is relatively faster and works well for small implants.[3]
ARTHROPLASTY TYPES AND HARDWARE
Tables 2 and 3 compiles the typss of hip arthroplasties based on the part of the hip joint that is replaced and based on the fixation technique used respectively.
| S.no. | Type of replacement | Part replaced | Patient profile |
|---|---|---|---|
| 1. | Total hip arthroplasty (THR) | Acetabulum, Femoral head and neck | Osteoarthritis- both primary and secondary Younger and more active patients |
| 2. | Hemiarthroplasty | Femoral head and neck | Unstable femoral neck fractures Older, co-morbid patients that cannot undergo THR |
| 3. | Resurfacing arthroplasty | Acetabulum and part of femoral head | Young and active patients with good bone density |
| S. No. | Type of fixation | Patient profile | ||
|---|---|---|---|---|
| 1. | Cementless | Implant’s porous and textured surface allows | Patients with good | |
| new bone to grow into the implant | bone density | |||
| 2. | Cemented | Hybrid: | Femoral stem -cemented | Older patients |
| Acetabular cup-cementless | Low bone density | |||
| Reverse Hybrid: | Femoral stem -cementless | |||
| Acetabular cup-cemented |
Types of surgeries
THA: Replacement of the femoral head, neck, and acetabulum with prosthetic components.
Hemiarthroplasty: Replacement of only the femoral head and neck commonly performed in femoral neck fractures.
Hip rsurfacing: Involves capping the femoral head with a metal prosthesis, preserving more bone.[9]
Prosthesis types
Cemented Prostheses: Fixed with bone cement for immediate stability, often used in elderly patients with poor bone quality.
Uncemented Prostheses: Achieve fixation through bone ingrowth into porous surfaces, ideal for younger patients with good bone stock.
Ceramic Prostheses: Durable and low-wear components often used in younger or active patients.
Hybrid Prostheses: Combine cemented and uncemented components for optimal stability.[10]
POST-ARTHROPLASTY COMPLICATIONS
Periprosthetic osteolysis/aseptic loosening
Periprosthetic osteolysis begins with wear-induced inflammation, where implant debris triggers an immune response that disrupts normal bone homeostasis, leading to bone resorption [Figure 2]. While normal osseous integration shows direct contact between the implant and surrounding bone, pathological changes manifest as abnormal signal intensity patterns on MRI [Figure 3]. The condition poses a diagnostic challenge as patients often remain asymptomatic despite significant bone loss. MRI has emerged as the most sensitive imaging modality for detecting and quantifying osteolysis, surpassing both conventional radiographs and CT.[11] On MRI, osteolysis appears as well-defined areas of intermediate signal intensity surrounded by a characteristic low-signal rim, contrasting with the high signal of normal marrow fat [Figures 4 and 5]. This pattern helps differentiate osteolysis from infection or tumoral involvement. Implant “loosening,” as a term should be used when there is extensive or circumferential bone resorption, especially when accompanied by implant displacement or rotation. Serial MRI examinations allow quantitative monitoring of osteolysis progression, with fibrous membrane formation indicated by 1–2 mm hyperintense signal thickness and bone resorption suggested by irregular areas exceeding 2 mm[12] [Figures 6 and 7].
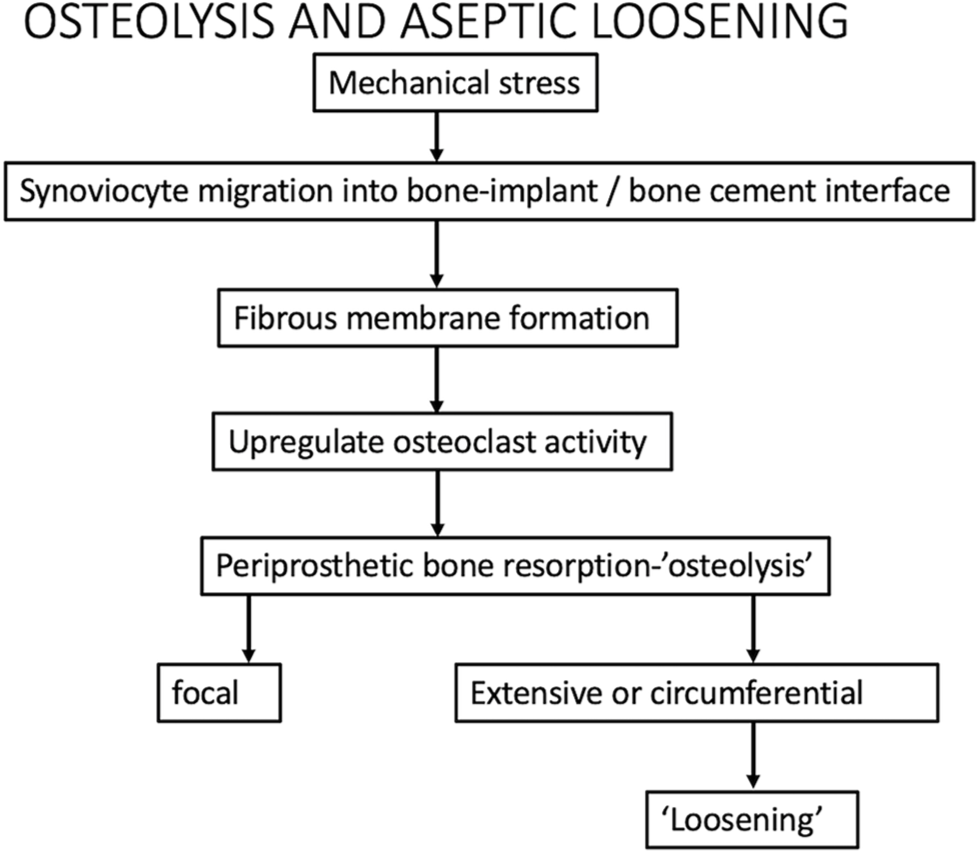
- Flowchart showing the pathogenesis of osteolysis and loosening.
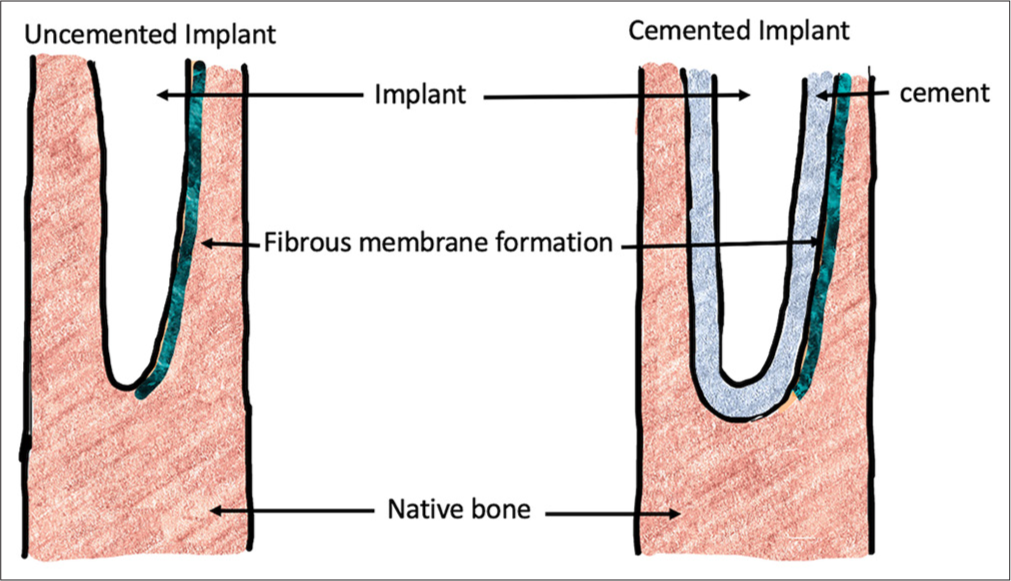
- Periprosthetic bone resorption: Schematic showing fibrous membrane formation at the implant bone interface and cement bone interface in uncemented and cemented implants.
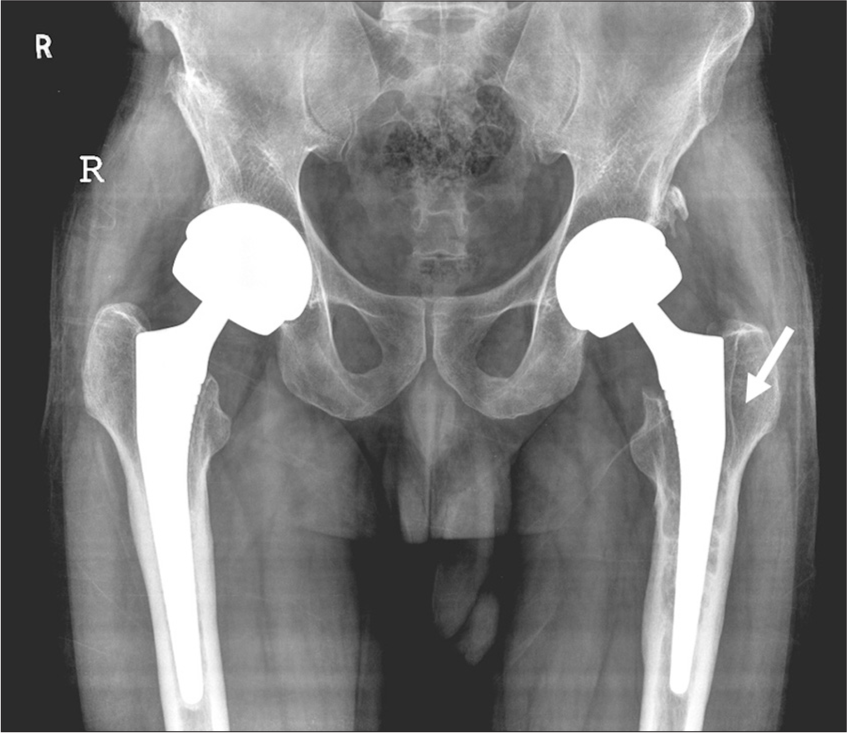
- Osteolysis. Plain radiograph of the pelvis with both hips, showing linear lucency (white arrow) at the bone prosthesis interface of the left femur.
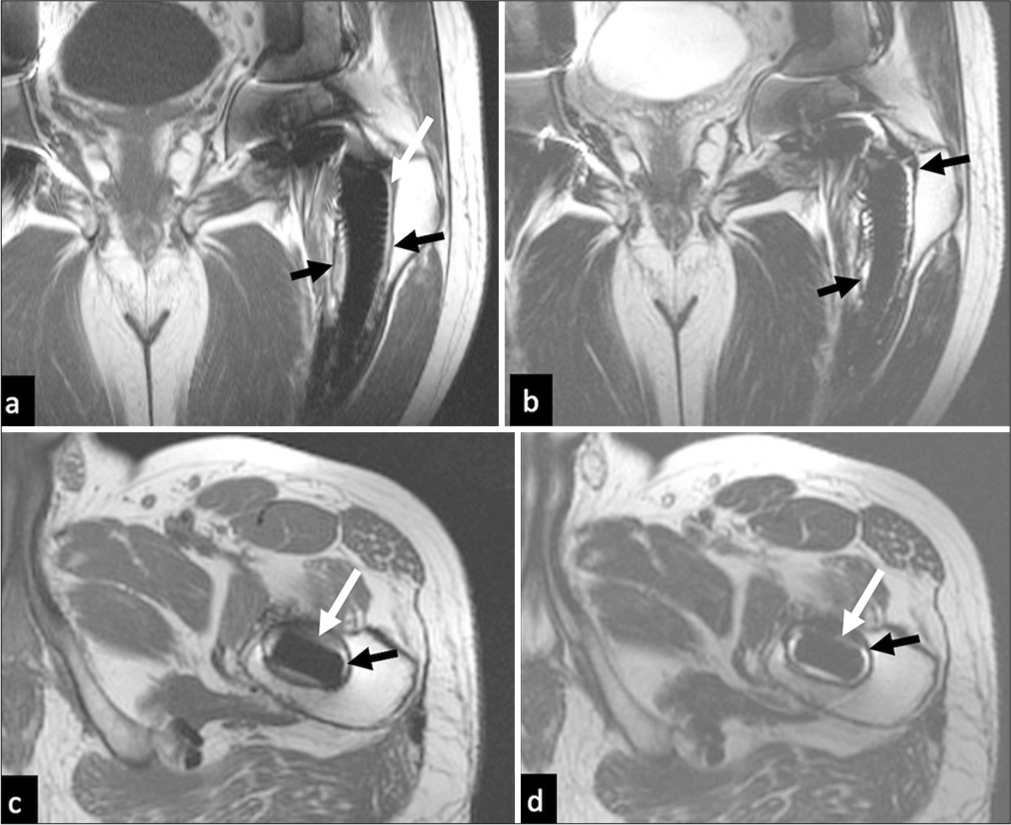
- Osteolysis. MRI (a) Coronal T1, (b) T2, (c ) axial T1, and (d) T2 images show circumferential intermediate signal (white arrows in a-d) surrounded by a characteristic low-signal rim (black arrows in a-d) at the bone prosthesis interface encasing the stem of the prosthesis.
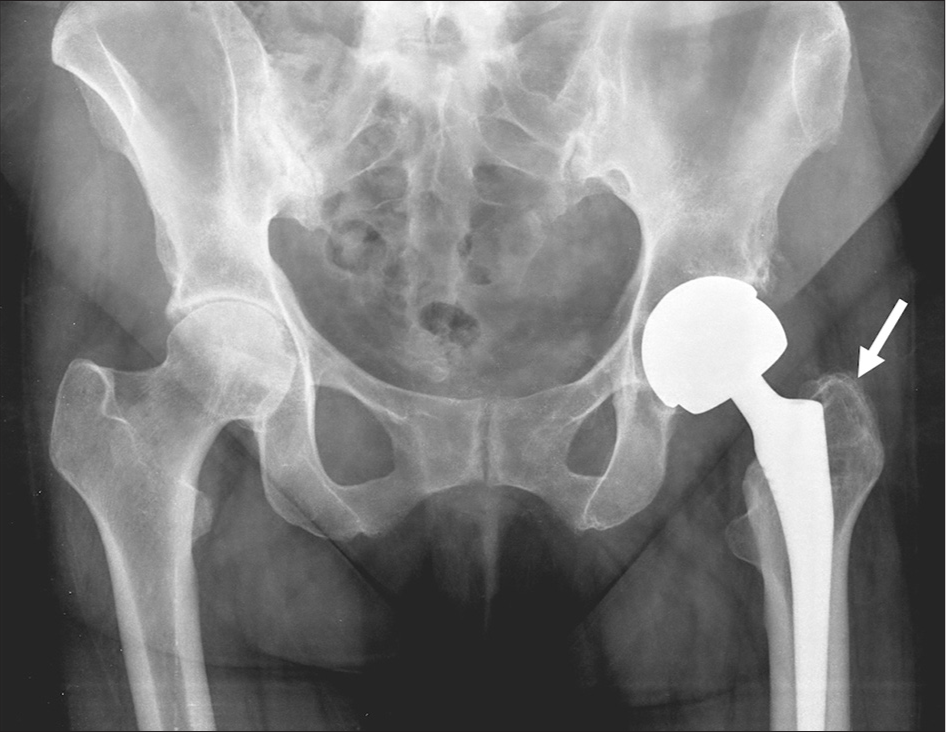
- Focal osteolysis. Plain radiographs of the pelvis with both hips show focal osteolysis (white arrow) at the bone prosthesis interface of the left femur
- MRI (a) Coronal T1 and (b) T2, images demonstrate well- circumscribed focal lobulated areas of intraosseous increased T2-weighted signal change (black arrow) without any peri-osseous collection consistent with focal osteolysis.
Periprosthetic fracture and stress reaction
Periprosthetic fractures predominantly affect the femoral component, while the acetabular aspect is less commonly affected but difficult to assess on MRI due to significant artifacts produced by virtue of its shape and orientation along the magnetic field. There are several predisposing factors, including varus positioning of components, previous fracture history, and osteolysis. On MRI, normal periprosthetic cortex and periosteum appear hypointense on both short tau inversion recovery and intermediate weighted fast spin echo sequences. A stress reaction manifests as a localized hyperintense signal in the marrow cavity and endosteum, accompanied by cortical thickening and hyperintensity without a discrete fracture line, often associated with periosteal changes and adjacent soft-tissue edema. The key feature of a fracture is the presence of a linear hypointense signal disrupting the cortex, which is absent in stress reactions. Non-displaced periprosthetic fractures are often occult on radiographs as well as CT scans but are a source of significant pain. Insufficiency fractures of the sacrum or pubic rami may also be a source of post-arthroplasty pain. Thus, it is essential to keep this differential in mind and use a large field of view as part of the routine protocol for imaging hip arthroplasties.[13]
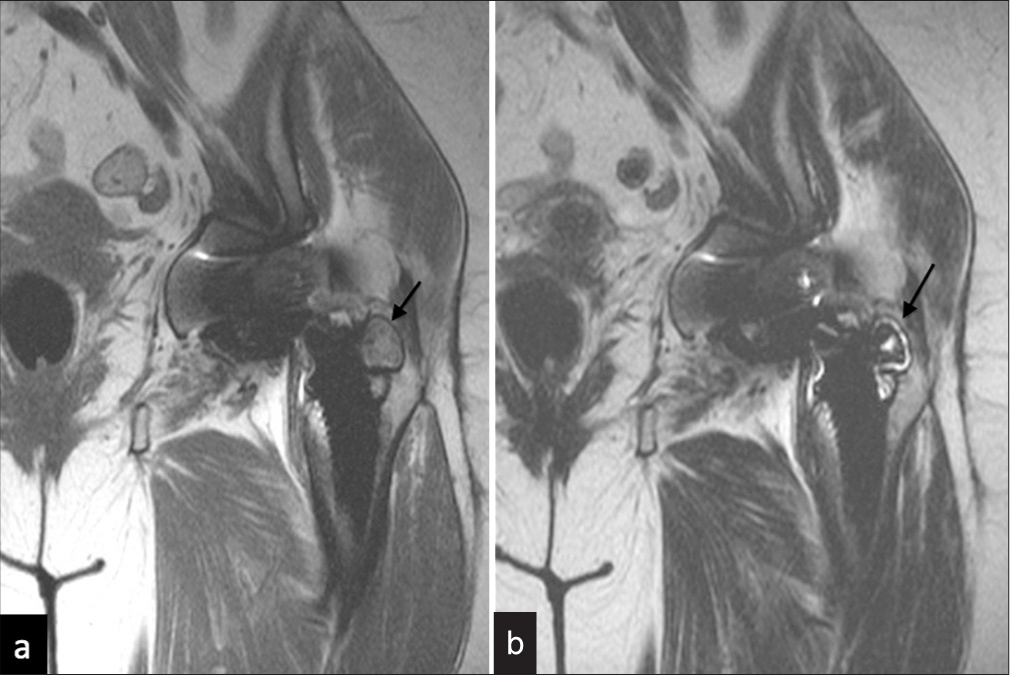
Periprosthetic infection
Periprosthetic infection represents one of the most challenging complications in hip arthroplasty, demanding prompt recognition and management to avert complications such as implant failure or systemic infection. MRI demonstrates characteristic features that parallel those seen in other skeletal infections, including enhanced synovial inflammation, fluid accumulation within the joint, and inflammatory changes in the subchondral bone marrow with abnormal enhancement patterns.[14] Additional findings encompass osseous destruction, osteolysis around the prosthesis, inflammatory reaction of the periosteum, inflammatory changes in surrounding soft tissues, fluid collections with potential cutaneous fistulae, and enlarged regional lymph nodes. A distinctive imaging pattern suggesting infection is the presence of layered thickening of the synovium with increased signal intensity[7] [Figures 8-10].

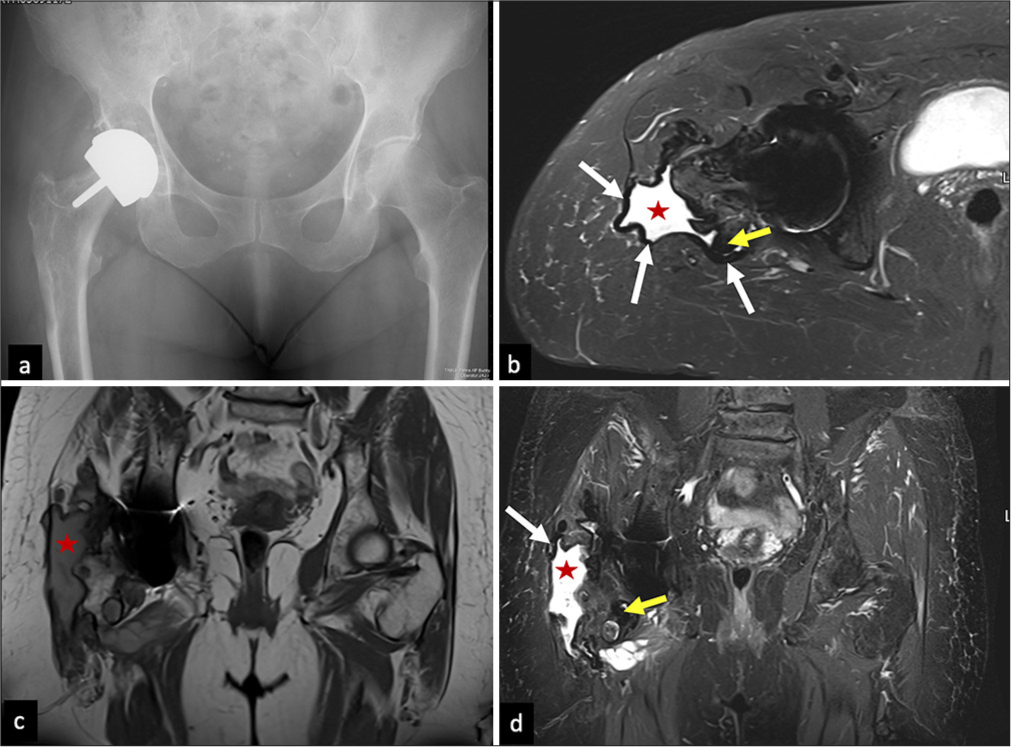
- Infection. Plain radiographs of the pelvis with both hips, showing focal osteolysis (white arrow) at the bone prosthesis interface of the left femur with cortical irregularity.
- Infection. MRI (a) Coronal T1, (b) T2, (c) axial T1, and (d) T2 images show multiple pockets and a large loculated collection surrounding the left hip (red stars in a-d).
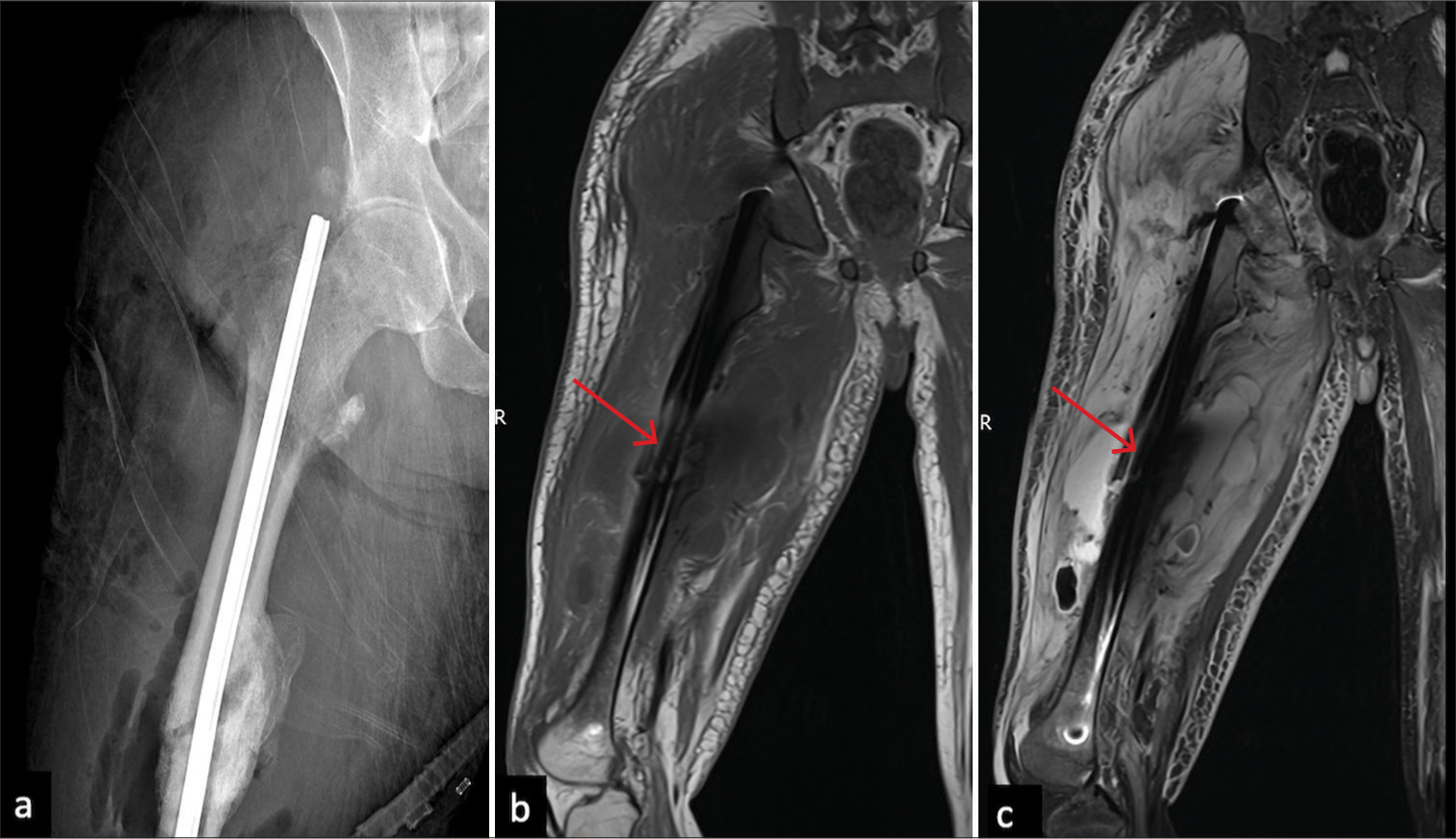
- Infection. (a) Radiograph of the right femur showing an intramedullary nail for an oblique shaft fracture showing cortical thickening and solid periosteal reaction in the mid shaft around the fracture site, blurring of surrounding fat planes. (b) MRI Coronal T1 non-FS (Fat Suppressed) and (c) T2 FS reveals intermediate signal along the anterolateral cortex on T1 (red arrow in b) and linear fluid signal just deep to it on T2FS (red arrow in c) which is contiguous with large collection in the peri osseous soft tissue with surrounding extensive soft tissue edema. There is associated marrow edema in the proximal femoral shaft and right subchondral location of the right hip joint involvement.
However, diagnostic challenges arise as similar imaging patterns can be observed in cases of wear debris reaction, implant-related adverse tissue responses, and underlying inflammatory arthropathies. These conditions may coexist with infection, creating complex imaging presentations. Definitive diagnosis of infection typically requires joint fluid analysis through image-guided aspiration. The infectious process can subsequently lead to implant loosening. MRI demonstrates superior capability in distinguishing infectious from non-infectious loosening by better visualizing inflammatory changes, fluid collections, and periosteal reactions, thereby facilitating appropriate therapeutic planning, whether surgical cleaning or antimicrobial therapy.[15]
Synovitis
Synovial inflammation frequently occurs within the joint capsule following hip surgery and can arise from multiple etiologies. MRI stands as the imaging technique of choice for evaluating both the extent and characterization of synovitis.[9] Careful assessment of several key features aids in determining the underlying cause: The degree and pattern of synovial thickening, its signal characteristics, the volume of fluid accumulation within the joint space, and the signal properties of the joint fluid itself. In addition, evaluating associated changes in the surrounding bone and soft tissues adjacent to the prosthesis helps clinicians narrow down the differential diagnosis and determine the specific pathological process.[7] In the presence of extensive synovitis and joint fluid distension, it can decompress into the iliopsoas bursa anteriorly and the trochanteric bursa posteriorly if there is a posterior pseudocapsule dehiscence[6,7,16] [Table 4].
| Imaging finding | Non-specific synovitis | Polyethylene wear-induced synovitis | ALVAL | Metallosis | Infection | |
|---|---|---|---|---|---|---|
| 1 | Joint effusion | |||||
| Volume | Small | Moderate-large | Usually large | Variable | Variable | |
| Signal intensity | Uniformly hyperintense | Intermediate | Hyperintense | Hypointense with susceptibility artifact | Hyperintense with debris | |
| 2 | Synovial thickening | |||||
| Thickness | Thin | Mild thickening | Mild-moderate thickening | Mild thickening | Lamellated thickening | |
| Signal intensity | low | Low to intermediate | hyperintense | Hypointense with susceptibility artifact | Hyperintense (hypointense in Tuberculosis) | |
| 3 | Bone involvement | Absent | Common and typically bulky osteolysis, with intermediate signal intensity (SI) content | Not a dominant feature, except for pressure erosion from the distended pseudocapsule | Common, genographic with hypointense SI content | Common, aggressive pattern |
| 4 | Periprosthetic soft tissue | |||||
| Pseudocapsule dehiscence | Absent | Common | Common | Common | Common | |
| Necrosis of soft tissue | Absent | Absent | Common | Uncommon | Common | |
| Associated findings | Normal tissue planes | Intermediate SI debris | Soft-tissue edema, pseudotumor formation and lymphadenopathy | Intermediate SI debri | Soft-tissue edema, collection, lymphadenopathy, and sinus tract formation | |
MRI: Magnetic resonance imaging, ALVAL: Aseptic lymphocyte-dominant vasculitis-associated lesions, SI: Signal intensity
Non-specific synovitis
In normal conditions, the pseudocapsule presents as a thin, continuous structure with low-signal intensity that closely adheres to the implant neck. The presence of minimal joint fluid with a thin synovial lining, without evidence of debris, is a common finding and can be classified as a routine postoperative effusion without synovial inflammation. The diagnosis of nonspecific synovitis is specifically applied when MRI reveals joint fluid with uniform signal intensity accompanied by mild synovial wall thickening.[15] Although such synovial irritation may occur with both properly aligned and misaligned prosthetic components, this condition typically does not require intervention and does not constitute grounds for revision surgery.[6]
Polyethylene wear-induced synovitis
Polyethylene wear-induced synovitis develops from the degradation of acetabular polyethylene liners in metal-onpolyethylene and ceramic-on-polyethylene implants. This occurs when mechanical stress between the femoral head and polyethylene component results in particle release into the joint space. These particles trigger a histiocytic inflammatory response in the synovium and lead to progressive osteolysis.[17]
On MRI, characteristic findings include intermediate signal debris within joint fluid and osteolytic regions. The hip pseudocapsule typically demonstrates expansion with thick, particulate synovitis showing low-to-intermediate signal intensity (comparable to muscle signal), interspersed with variable fluid content. In advanced cases, the inflammatory process may extend into surrounding bursae, including the greater trochanteric bursa posteriorly or the iliopsoas and subiliac bursae anteriorly. Due to its similar signal characteristics to muscle, careful evaluation is necessary to detect this extension. Diagnostic considerations include the presence of a polyethylene liner, implant longevity, and distinctive synovitis patterns. Associated osteolysis typically presents as bulky lesions where particulate debris replaces normal periprosthetic bone marrow signal[7] [Figure 11].
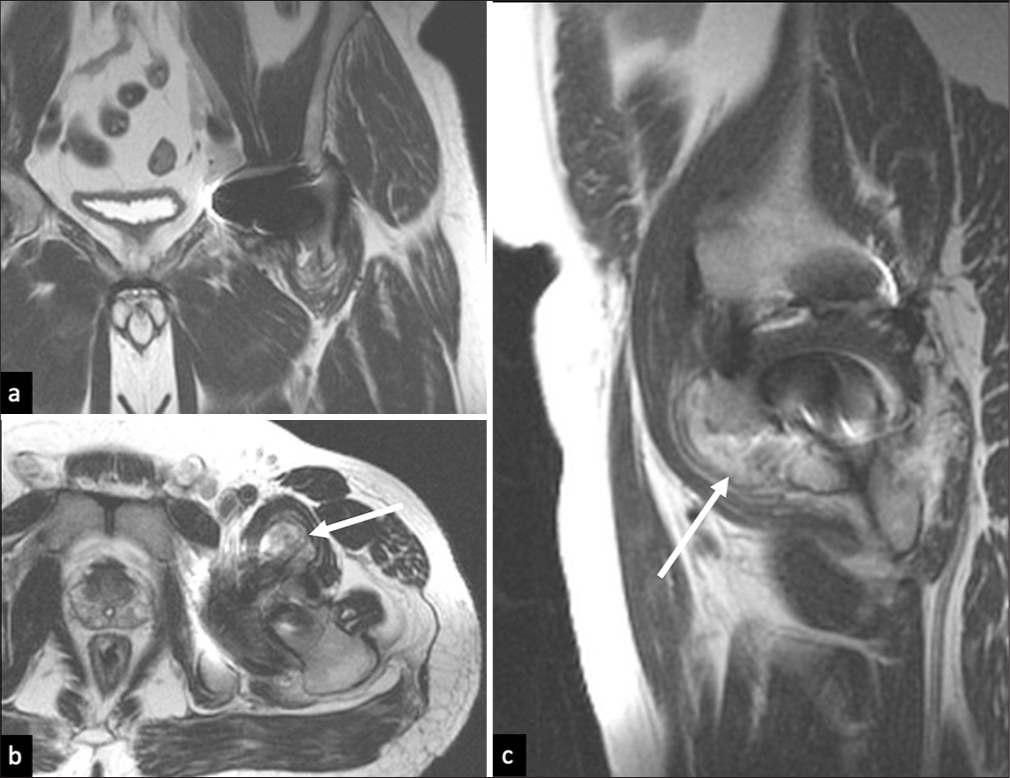
- Polyethylene wear induced synovitis. (a) T2 nonfs Coronal, (b) axial, and (c) sagittal images show pseudo capsule distension with low to intermediate thick-walled synovial lining and heterogeneous intermediate signal intensity debris that has decompressed into the left iliopsoas bursa (white arrows).
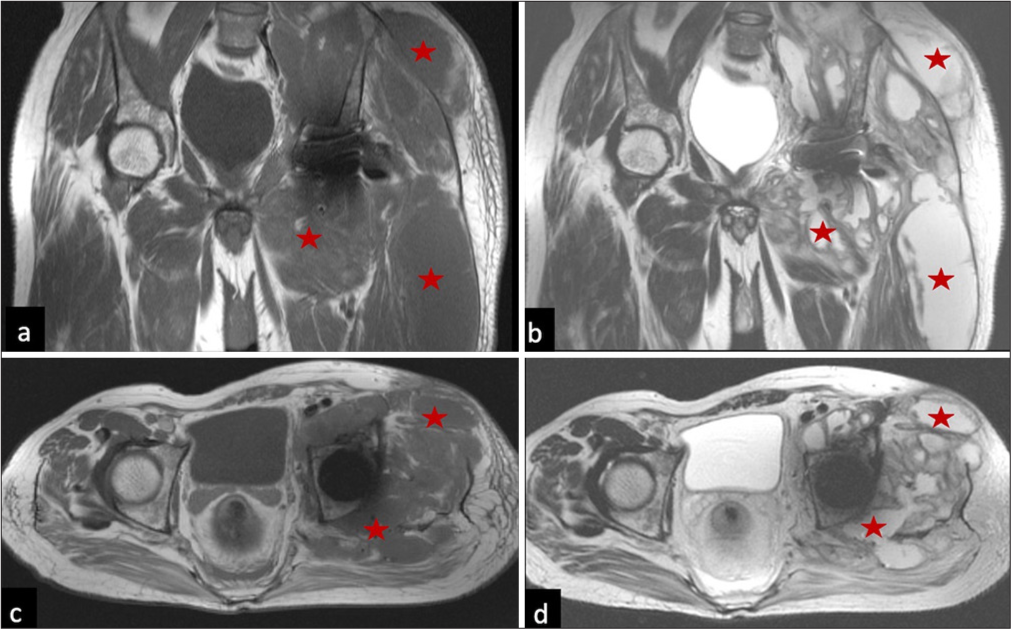
Adverse local tissue reaction (ALTR)
Metal-related complications following arthroplasty encompass a spectrum of conditions collectively termed ALTR. These pathologies arise from various metal products, including particulate debris, ionic forms, and corrosion byproducts. While high wear rates typically correlate with metallosis and low wear rates with hypersensitivity reactions, these conditions frequently overlap.[18]
The clinical significance of ALTR lies in its potential for extensive soft-tissue destruction. Notably, symptom severity does not reliably correspond with metal ion concentrations. MRI has emerged as a crucial diagnostic tool, with synovial signal characteristics proving more reliable than lesion size in predicting tissue damage. Several imaging markers indicate moderate to severe ALTR, including synovial thickening exceeding 7 mm, mixed solid-cystic synovial patterns, and pseudocapsular disruption with synovial fluid extravasation.[3,6]
Aseptic lymphocyte-dominant vasculitis-associated lesions (ALVAL)
ALVAL represents a distinct subset of ALTR characterized by type IV hypersensitivity response to metal ions and corrosion products. The histopathological hallmarks include variable degrees of tissue necrosis and infarction.[19] MRI typically reveals synovial proliferation and joint distension with hyperintense fluid forming pseudotumors [Figure 12]. Posterior pseudocapsular dehiscence commonly results in fluid decompression into the greater trochanteric bursa, potentially compromising adjacent structures including abductor tendons and sciatic nerve complexes. Anterior decompressions may affect the iliopsoas mechanism and femoral neurovascular structures [Figure 13]. Associated findings include periprosthetic edema and lymphadenopathy.[16]
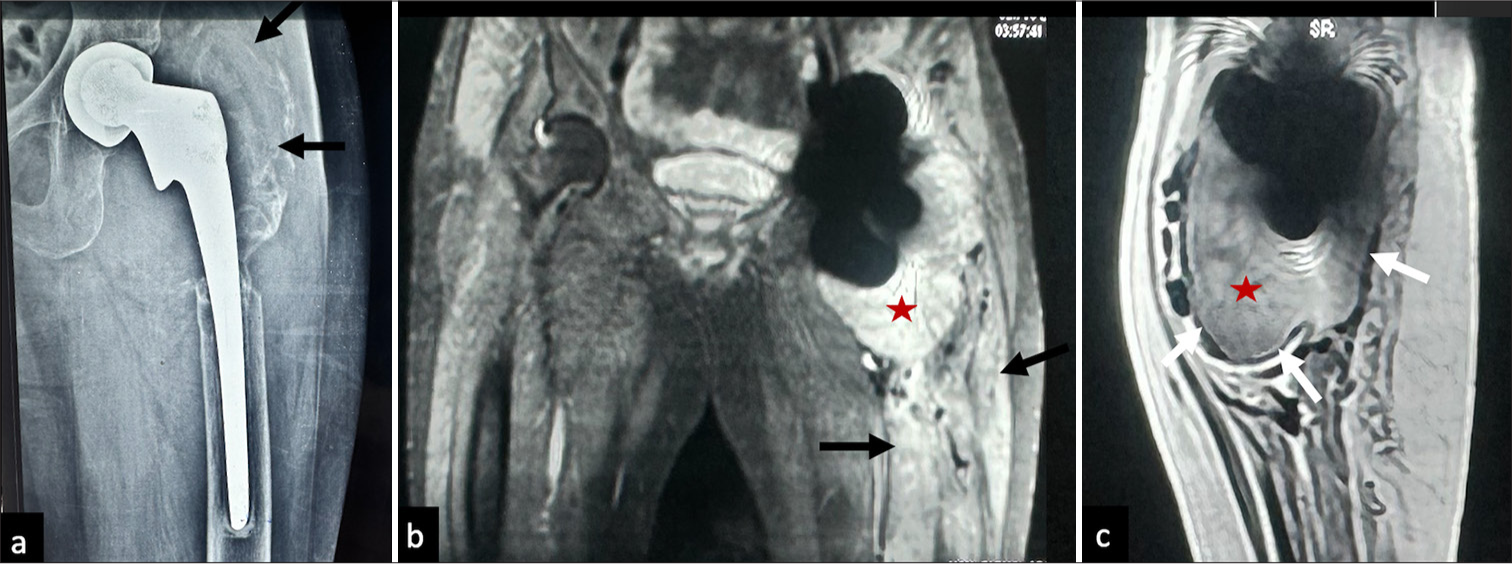
- Adverse local tissue reactions caused by hypersensitivity to metal products (ALVAL) (a) Anteriorposterior radiograph left hip joint showing marked osteolysis around the femoral component involving the greater trochanter (black arrows). (b) Coronal STIR and (c) sagittal T2 non fs MR image of the same patient showing marked distension of pseudo capsule with thin hypointense lining (white arrows) and intermediate to hyperintense signal fluid content (red star in b and c), there is marked periprosthetic soft tissue edema in the visualized left proximal left thigh (black arrows in a-c).
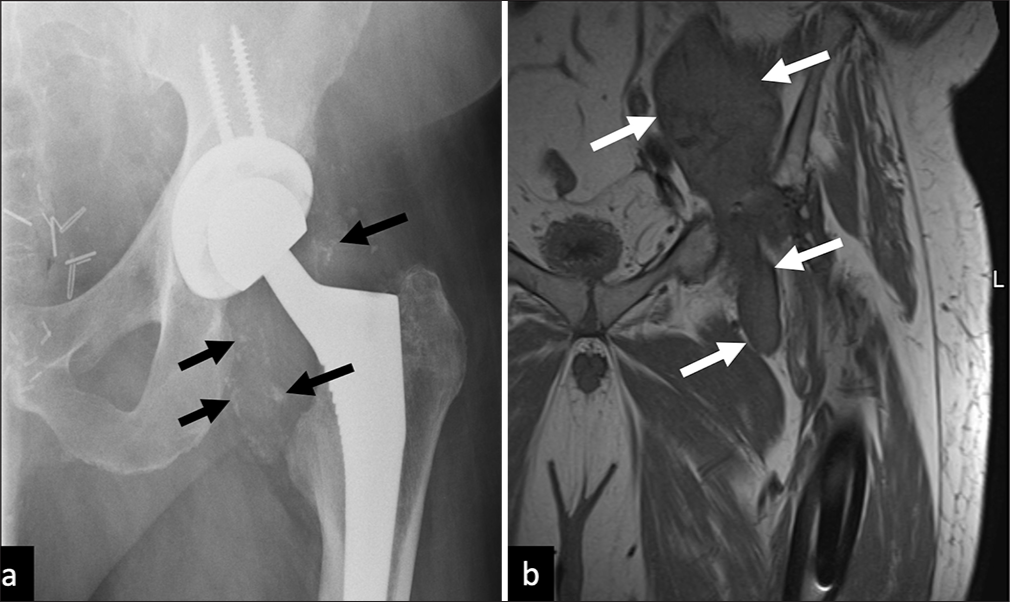
- Adverse local tissue reactions caused by hypersensitivity to metal products (ALVAL) in a metal-on-metal hip replacement patient. (a) Plain AP radiograph of the left hip shows metallic debris within the joint capsule (black arrows), and (b) Coronal T1 non FS MRI image demonstrates soft tissue extending along the left iliac and common femoral neurovascular bundle bursa (white arrow) in keeping with ALVAL. FS: Fat saturation, MRI: Magnetic resonance imaging, AP: Anterior-posterior.
Metallosis
It results from the shedding of larger metallic debris that triggers a macrophage-mediated response distinct from ALVAL.[20] The MRI signature includes low-signal synovitis with susceptibility artifacts and a characteristic pattern of progressive osteolysis, leading to implant failure. Metal accumulation may manifest as susceptibility artifacts within soft-tissue deposits and in the pelvic lymph nodes. While osteolysis can occur in both metallosis and hypersensitivity reactions, it is more characteristic of metallosis. Hypersensitivity reactions typically present with predominant soft-tissue involvement and necrosis. The coexistence of both conditions results in overlapping imaging features[21] [Figure 14].
- Metallosis: (a) AP pelvis with bilateral hip radiograph of a metal-on-metal right hip resurfacing arthroplasty system. (b) Axial STIR, (c) coronal T1 non FS, and (d) STIR MR images show dehiscence of the posterior pseudo capsule with fluid extending into the trochanteric bursa (red star in b-d), note the markedly hypointense synovial lining (white arrows in b and d) and few hypointense debris (yellow arrows in b and d). FS: Fat saturation, AP: Anteroposterior, STIR: Short tau inversion recovery, MR: Magnetic resonance.
While MRI generally enables accurate diagnosis of post-arthroplasty complications when interpreted in the appropriate clinical context, certain conditions require particular attention due to their potentially catastrophic consequences if misdiagnosed. Of special concern are vascular lesions, which can mimic pseudocapsular distension on imaging. This is particularly true in cases of pseudoaneurysms, where turbulent arterial flow can create flow voids that may be mistaken for pseudotumors containing metallic debris on standard MRI sequences. Such distinctions are crucial for proper patient management and avoiding adverse outcomes and ultrasound correlation becomes crucial [Figure 15].
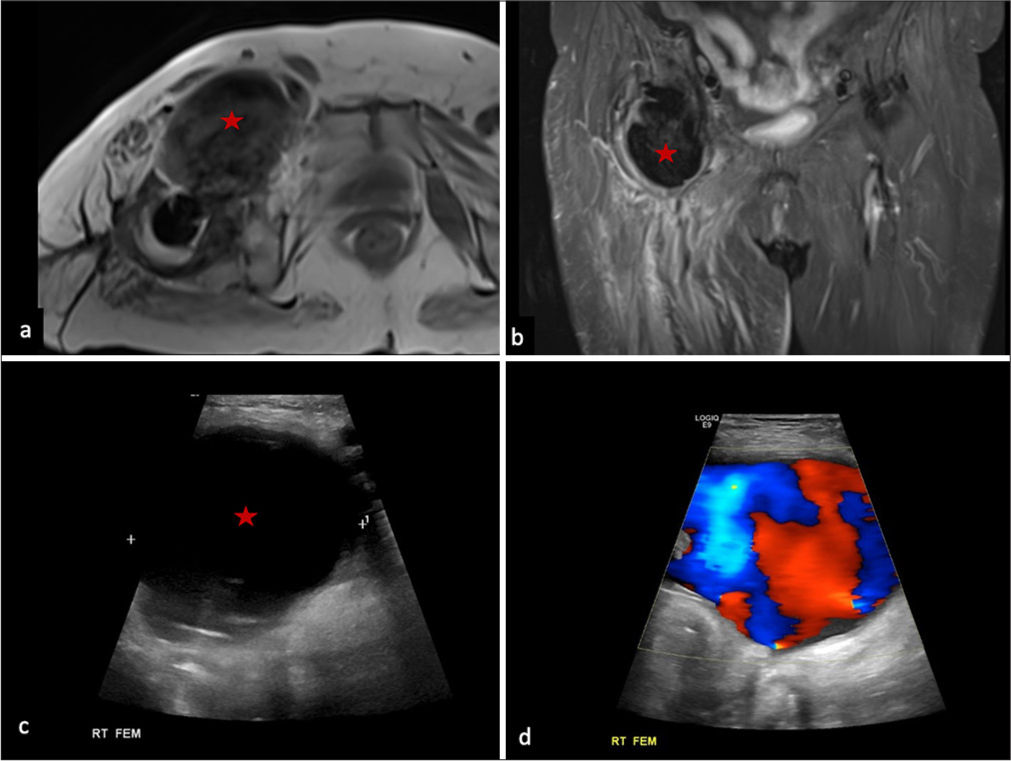
- Pseudotumor mimic: (a) T1 non-fs axial and (b) T2 fs coronal MRI in a patient of right total hip arthroplasty showing a large mass-like lesion with T1/T2 hypointense signal anterior to the right hip joint (red star in a and b), based on the MRI findings, a suspicion of pseudotumor formation with hypointense metallic debris within and causing decompression into the iliopsoas bursa can be raised. On ultrasound correlation of the lesion, (c) transverse view greyscale showed a large collection with anechoic internal content with a thin outline (red star), (d) on color doppler image, turbulent flow showing ‘to and fro’ pattern was seen suggesting pseudoaneurysm arising from the right femoral artery.
Muscle atrophy
Commonly seen in the gluteal group of muscles or piriformis due to altered biomechanics or nerve injury, post-surgery muscle atrophy is often asymptomatic and seen as an incidental finding unrelated to post-arthroplasty pain [Figure 16].
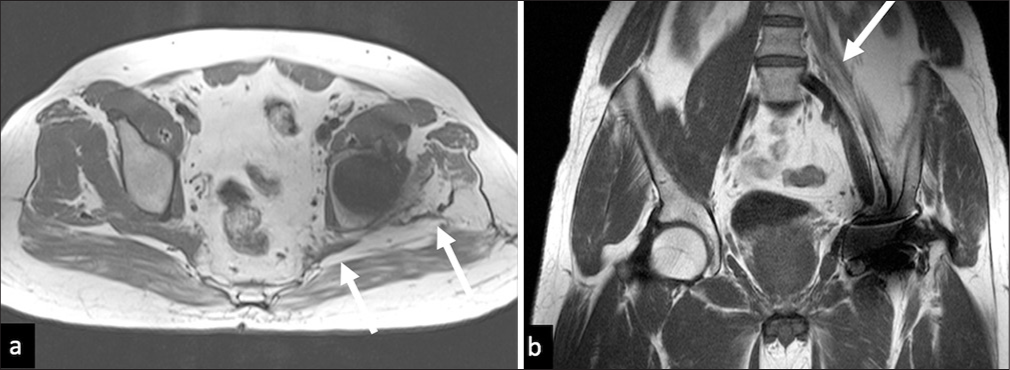
- Muscle atrophy. (a) Axial T2W showing severe atrophy of the left Gluteus medius and left piriformis (white arrows) and (b) coronal T1 W image in a different patient showing severe atrophy of the left iliopsoas (white arrow).
Muscle/tendon tear
Muscle/tendon tears and tendinopathy around the hip joint are also common causes of post-arthroplasty pain and gait abnormalities. These may be due to acute injuries or may be due to chronic repetitive injuries due to altered biomechanics and impingements. As muscle/tendon tears elsewhere in the body, these are best visualized on MRI.[15] On MRI, tendinopathy is seen as increased signal intensity with thickening or thinning (seen with chronic repetitive insult) of the involved tendon. Tears are seen as a discontinuity in the tendon fibrils, which may be partial or full thickness [Figure 17]. Acute tendon tears usually cause painful hips, while chronic tears often cause gait abnormalities.[2,7]
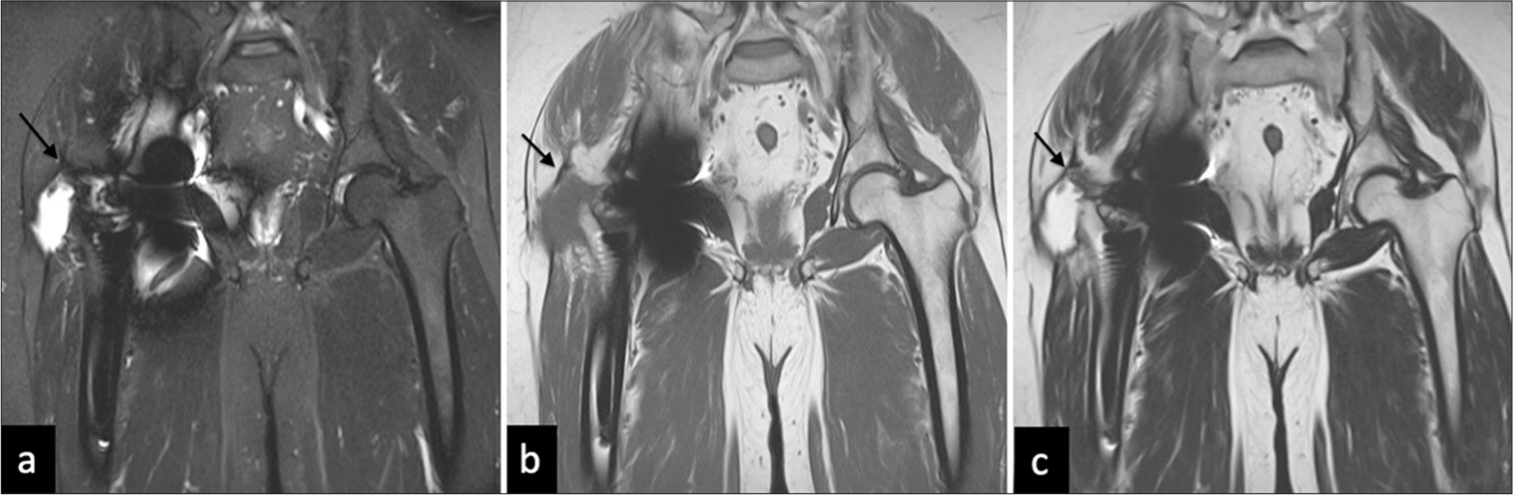
- Tendon tear. (a) Coronal STIR, (b) T1W, and (c) T2W images showing avulsion of the right Gluteus medius tendinous insertion from greater tuberosity insertion, with fluid in the trochanteric bursa (black arrows in a-c).
Impingement
Various impingement syndromes can happen surrounding the hip joint, especially after the THR, due to altered biomechanics. The more common ones are –
Ischiofemoral impingement
This is seen as reduced ischiofemoral distance or the quadratus femoris space and is best seen on axial images [Figure 18]. There are no definite criteria, but ischiofemoral space <1.5 cm with associated edema or atrophy of the quadratus femoris muscle belly should be considered with suspicion for ischiofemoral impingement. In these patients, radiographs are usually normal.[22]
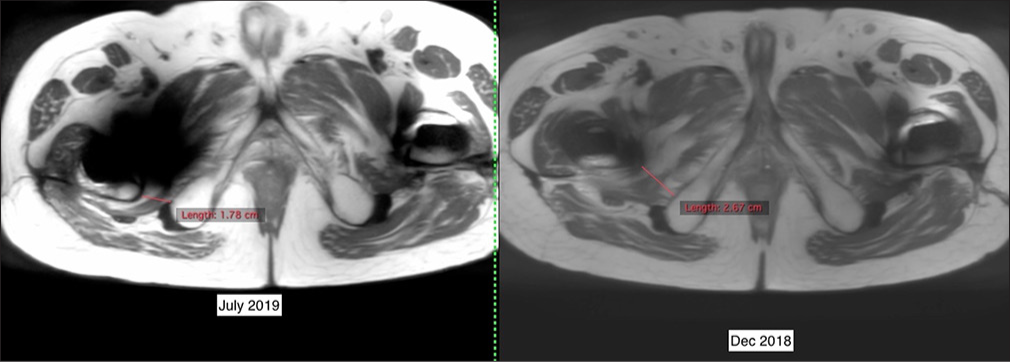
- Ischiofemoral Impingement. Axial T2 images obtained a year apart show a narrowing of the ischiofemoral space from December 2018 to July 2019.
Trochanteric-pelvic impingement
It is an extra-articular hip impingement caused between the greater trochanter and the ilium or posterior rim of the acetabulum, often due to loosening or any other structural malalignment [Figure 19].[23]
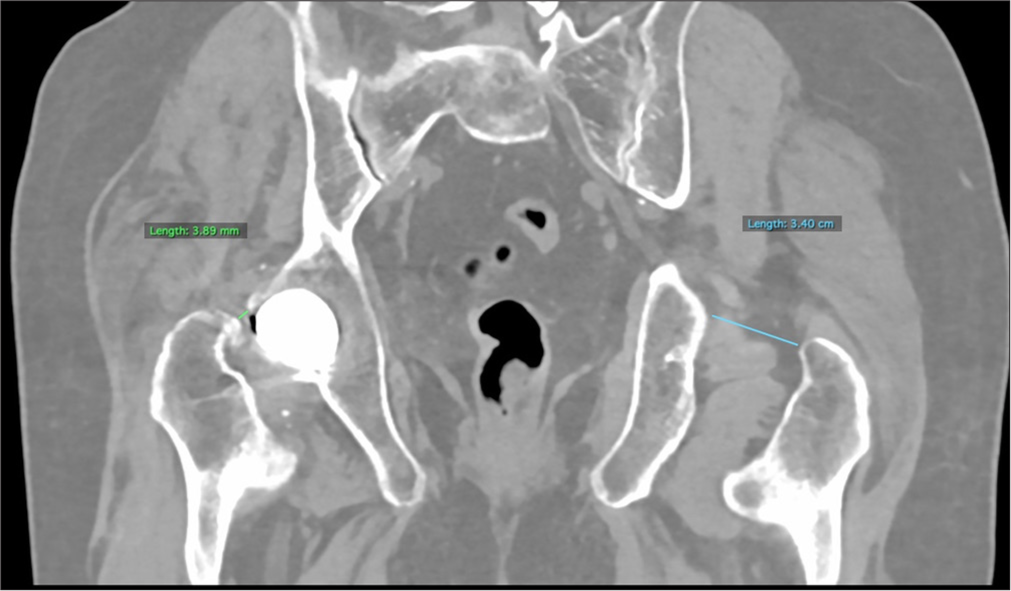
- Trochanteric-pelvic impingement. Reconstructed coronal computed tomography images shows decreased trochanteric-acetabulum distance on the right as compared to left – this is consistent with trochanteric pelvic impingement.
Take home points
MRI can be done even in the presence of metal, it allows detailed evaluation of periprosthetic bone, implant-tissue interfaces, and soft tissues, including the pseudocapsule and synovium, tendons, bursae, and nerves.
Use MARS or optimize the MRI study by altering parameters [Table 1].
ALTR-common term for any reactions to arthroplasty-related metal products, including metallosis and ALVAL.
Metallosis is caused by the shedding of larger metallic debris while ALVAL is a reaction to metal ions in solution and corrosion products.
Close monitoring of the synovial thickness, signal characteristics can give strong clues to the underlying pathology.
CONCLUSION
Imaging the post-operative hip is both an art and a science. Newer imaging technologies have made it possible to evaluate patients with metallic implants more effectively using MRI, reducing the limitations imposed by artifacts. Understanding the strengths and limitations of each imaging modality, along with the appropriate sequences and parameters to use, allows radiologists to provide critical diagnostic insights into post-arthroplasty complications. Appropriate use of MARSs, altering the bandwidth and frequency encoding direction is crucial to reduce the field inhomogeneity.
Knowledge of commonly encountered pathology around the prosthesis is vital, as imaging is only effective with a knowledge of the context or clinical situation in question. When in doubt, a correlation with other imaging modalities such as CT or Ultrasound is important, while the plain radiograph remains the basic and key imaging modality.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Persistent pain after joint replacement: Prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566-72.
- [CrossRef] [PubMed] [Google Scholar]
- A review of the clinical approach to persistent pain following total hip replacement. Hong Kong Med J Xianggang Yi Xue Za Zhi. 2016;22:600-7.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging of joint arthroplasty. Orthop Clin North Am. 2006;37:361-73, vi-vii
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of susceptibility-induced magnetic field inhomogeneities. Radiology. 1988;168:837-41.
- [CrossRef] [PubMed] [Google Scholar]
- Metal artifact reduction sequence: Early clinical applications. Radiogr Rev Publ Radiol Soc N Am Inc. 2000;20:699-712.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging in hip arthroplasty management part 2: Postoperative diagnostic imaging strategy. J Clin Med. 2022;11:4416.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of hip arthroplasty implants. RadioGraphics. 2014;34:E106-32.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction of metal artifacts in patients with total hip arthroplasty with slice-encoding metal artifact correction and view-angle tilting MR imaging. Radiology. 2012;265:204-14.
- [CrossRef] [PubMed] [Google Scholar]
- Metal Artefact Reduction Sequences (MARS) in Magnetic Resonance Imaging (MRI) after Total Hip Arthroplasty (THA): A non-invasive approach for preoperative differentiation between periprosthetic joint infection (PJI) and aseptic complications? BMC Musculoskelet Disord. 2022;23:620.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging in the evaluation of periprosthetic acetabular osteolysis: A cadaveric study. J Orthop Res. 2005;23:713-9.
- [CrossRef] [PubMed] [Google Scholar]
- The role of MRI in the diagnosis of aseptic loosening following total hip arthroplasty. Arch Orthop Trauma Surg. 2024;144:4989-93.
- [CrossRef] [PubMed] [Google Scholar]
- Periprosthetic insufficiency fracture around radiographically loose cemented stem: A report of two cases. Hip Pelvis. 2015;27:183-6.
- [CrossRef] [PubMed] [Google Scholar]
- Periprosthetic infection in joint replacement. 2017. Deutsches Ärzteblatt. Available from: https://www.aerzteblatt.de/int/archive/article?id=188637 [Last accessed on 2025 Jan 21]
- [Google Scholar]
- Magnetic resonance imaging of the postoperative hip. J Magn Reson Imaging. 2012;35:1013-25.
- [CrossRef] [PubMed] [Google Scholar]
- Total knee arthroplasty: Diagnostic accuracy of patterns of synovitis at MR imaging. Radiology. 2016;281:499-506.
- [CrossRef] [PubMed] [Google Scholar]
- Frondlike synovitis on MRI and correlation with polyethylene surface damage of total knee arthroplasty. Am J Roentgenol. 2017;209:W231-7.
- [CrossRef] [PubMed] [Google Scholar]
- MRI characteristics of adverse local tissue reactions associated with intraoperative tissue damage and poor revision surgery outcomes: A systematic review. J Am Acad Orthop Surg. 2021;29:e1025-33.
- [CrossRef] [Google Scholar]
- MRI Predicts ALVAL and tissue damage in metal-on-metal hip arthroplasty. Clin Orthop. 2014;472:471-81.
- [CrossRef] [PubMed] [Google Scholar]
- MRI Findings in painful metal-on-metal hip arthroplasty. Am J Roentgenol. 2012;199:884-93.
- [CrossRef] [PubMed] [Google Scholar]
- Ischiofemoral impingement syndrome: An entity with hip pain and abnormalities of the quadratus femoris muscle. Am J Roentgenol. 2009;193:186-90.
- [CrossRef] [PubMed] [Google Scholar]
- Extra-articular hip impingement: A narrative review of the literature. J Can Chiropr Assoc. 2016;60:47-56.
- [Google Scholar]







