Translate this page into:
Bilateral developmental coxa vara

*Corresponding author: Riya Samanta, Department of Radiology, Mahajan Imaging and Labs, Safdurjung Hospital, Sports Injury Centre, New Delhi, India. samanta.ria1011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Samanta R, Batta NS, Batra V. Bilateral developmental coxa vara. Indian J Musculoskelet Radiol. 2025;7:130-3. doi: 10.25259/IJMSR_74_2024
Abstract
Coxa vara in children is either a consequence of a congenital malformation or a developmental anomaly and is defined as a decrease in the femoral neck-shaft angle below a normal of 120°. The chief clinical features are limb shortening/deformity, limping, and delay or difficulty in walking. In cases of bilateral involvement, a distinctive waddle and exaggerated lumbar lordosis is noted. Prompt and early management leads to good results, whereas untreated cases often advance to crippling disabilities. This case report describes a 6-year-old boy presenting with walking difficulty, having the characteristic clinicoradiological features of bilateral developmental coxa vara.
Keywords
Congenital coxa vara
Developmental coxa vara
Infantile coxa vara
Inverted Y-shaped ossification defect
Triangular metaphyseal fragment
INTRODUCTION
Coxa vara in children is either a consequence of a congenital malformation or a developmental anomaly of the proximal femur. In the literature, it has been described under the headings “congenital coxa vara,” “infantile coxa vara,” “developmental coxa vara,” and “cervical coxa vara.” It is characterized by a decrease in the femoral neck-shaft angle below a normal of 120°.[1] The chief clinical features are limb shortening/deformity, limping, and delay or difficulty in walking. In cases of bilateral involvement, a distinctive waddle and exaggerated lumbar lordosis is noted. Pain is not a common symptom unless weight-bearing or walking have led to secondary changes.[1] Both genders are equally affected. Bilateral involvement is seen in about 30% of the cases.[2]
The etiopathology involved is an osteochondral dysplasia of the neck of femur and is characterized by distinctive imaging features.[3] A triangular fragment develops in the femoral neck which has been proposed by many investigators to have developed as a result of an additional ossification center (ununited)[4]/osteochondritis/vascular insufficiency or an insufficiency fracture.[5] Normally, the femoral neck is essentially thought to be a continuation of the femoral shaft which grows superomedially forming an angle with the long axis of the shaft which is wider in infancy and becomes narrower with continuing growth until, in the adult, it is about 120°. The medial process of the femoral neck extends along the undersurface of the femoral head/capital epiphysis and plays a significant role in supporting the head from below. In congenital/developmental coxa vara, the space which is normally occupied by this medial process is instead occupied by a triangular fragment of bone/an additional ununited ossification center. Subsequently, the femoral head is no longer supported by the medial process; it sinks downwards under the pressure of the bodyweight and eventually coxa vara deformity ensues [Figure 1].[4] The biomechanics of the hip region are so profoundly altered that serious disability ensues in the childhood or early adolescence unless recognized early and given prompt treatment. Imaging plays a key role in early detection of the pathology. Imaging evaluation includes radiographs (X-rays) and computed tomography (CT). Plain radiographs can clearly demonstrate all the characteristic imaging findings; however, CT scans are essential for better characterization and delineation of the deformity and for surgical planning. Till date, many authors have used the terms “congenital coxa vara” and “developmental coxa vara” interchangeably; however, few researchers have found that ideally the term “congenital coxa vara” should be used in cases where there are associated congenital anomalies such as hip dislocation, cleidocranial dysostosis, and abnormal femoral development as in proximal focal femoral deficiency.[1] Magnetic resonance imaging has limited role in the detection of these pathologies; however, it may be helpful in providing information and characterization of associated abnormalities such as acetabular dysplasia.
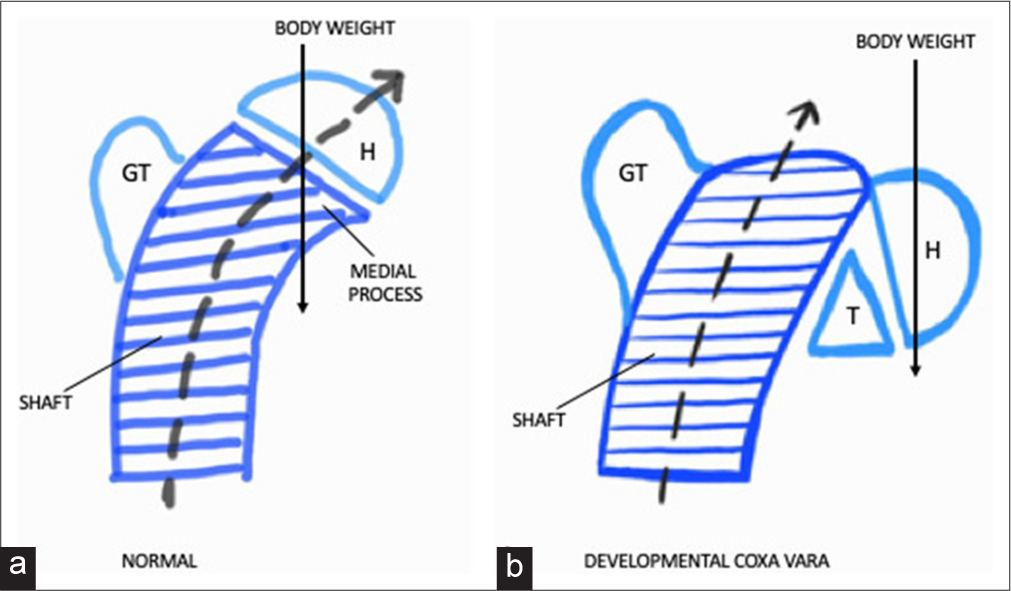
- Diagram showing (a) normal femoral development and (b) developmental coxa vara. Normally, the femoral neck is a continuation of the femoral shaft which grows superomedially (black dashed arrow). The medial process of the femoral neck extends along the undersurface of the femoral head/capital epiphysis (H) and plays a significant role in supporting the head from below. In congenital/developmental coxa vara, the space which is normally occupied by the medial process is instead occupied by a triangular fragment of bone (T)/an additional ununited ossification center. The femoral shaft shows upward growth only (instead of the normal superomedial growth) (black dashed arrow). Subsequently, the femoral head is no longer supported by the medial process; it sinks downwards under the pressure of the bodyweight (long black arrow) and eventually coxa vara deformity ensues. GT: Greater trochanter.
CASE REPORT
A 6-year-old boy presented with a painless waddling gait which was insidious in onset and was noticed by the parents as the child began walking. There was no significant history of trauma or swelling. The family history was negative.
The deformity had continued to increase with the child’s growth, and he was eventually brought to the hospital for analysis. Clinical examination revealed moderate lordosis. Trendelenburg’s sign was positive bilaterally. Abduction and internal rotation were limited on both sides. The greater trochanters (GTs) were noted to be superiorly positioned – above the Nelaton’s line on both sides.
Radiographic examination (X-ray) revealed markedly reduced bilateral femoral neck-shaft angle, that is, coxa vara deformity with poorly developed femoral neck. The neck-shaft angle measured 66.6° on the right side and 77° on the left side. The orientation of the growth plate was nearly vertical. Considerable juxta-metaphyseal-epiphyseal irregularity was present with a triangular bone fragment located inferiorly in the area of the growth plate. The GTs were markedly elevated [Figure 2]. CT was done for better evaluation of the status of acetabulum and femoral head, deformity configuration, assessment of bone stock, and physeal widening, thereby enabling proper surgical planning [Figure 3]. CT images revealed severe bilateral developmental coxa vara, with widened, irregular and nearly vertically oriented growth plates, and inverted Y-shaped ossification defects/triangular metaphyseal fragments at the inferior aspect of the region of femoral neck bilaterally. The femoral neck appeared short and deformed bilaterally. Both acetabuli showed normal development with no sign of dysplasia. The femoral shafts were displaced posterosupero-laterally. The femoral heads appeared osteopenic and showed irregularity and sclerosis at their lateral aspects. A diagnosis of bilateral developmental coxa vara was made and the child was referred to the orthopedic team for further management. A plan for bilateral corrective valgus derotation osteotomy was made with the aim of restoring the growth plate at a more horizontal position, thereby eliminating the abnormal shearing forces of weight-bearing that affect normal growth.
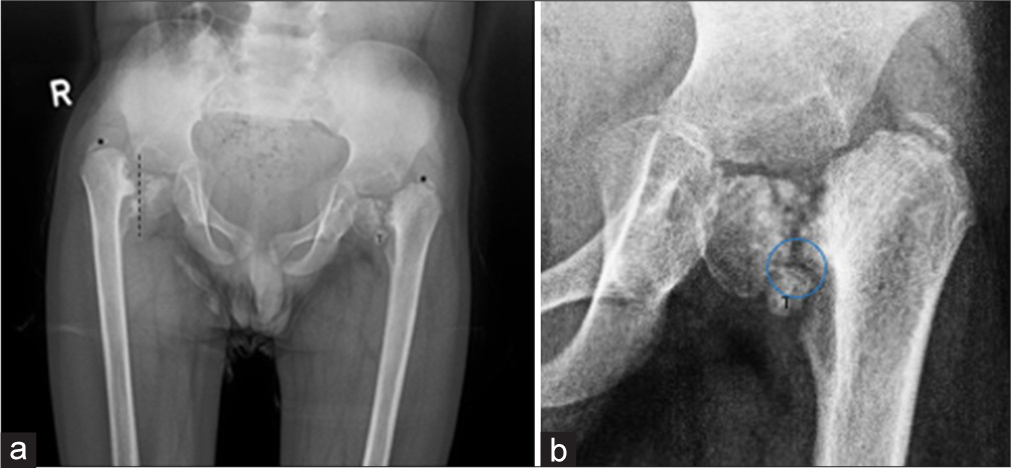
- (a) Plain radiograph of pelvis with both hip joints in a 6-year-old boy with waddling gait showing markedly reduced bilateral femoral neck-shaft angle, that is, bilateral coxa vara deformity with poorly developed femoral neck. The orientation of the growth plate was nearly vertical (dotted line). Considerable juxta-metaphyseal-epiphyseal irregularity was present with a triangular bone fragment (T) located inferiorly in the area of the growth plate. The greater trochanters were markedly elevated (asterisk). (b) Magnified radiographic image showing inverted Y-shaped ossification defect (blue ring) at the inferior aspect of the region of femoral neck seen due to ununited triangular bone fragment (T).
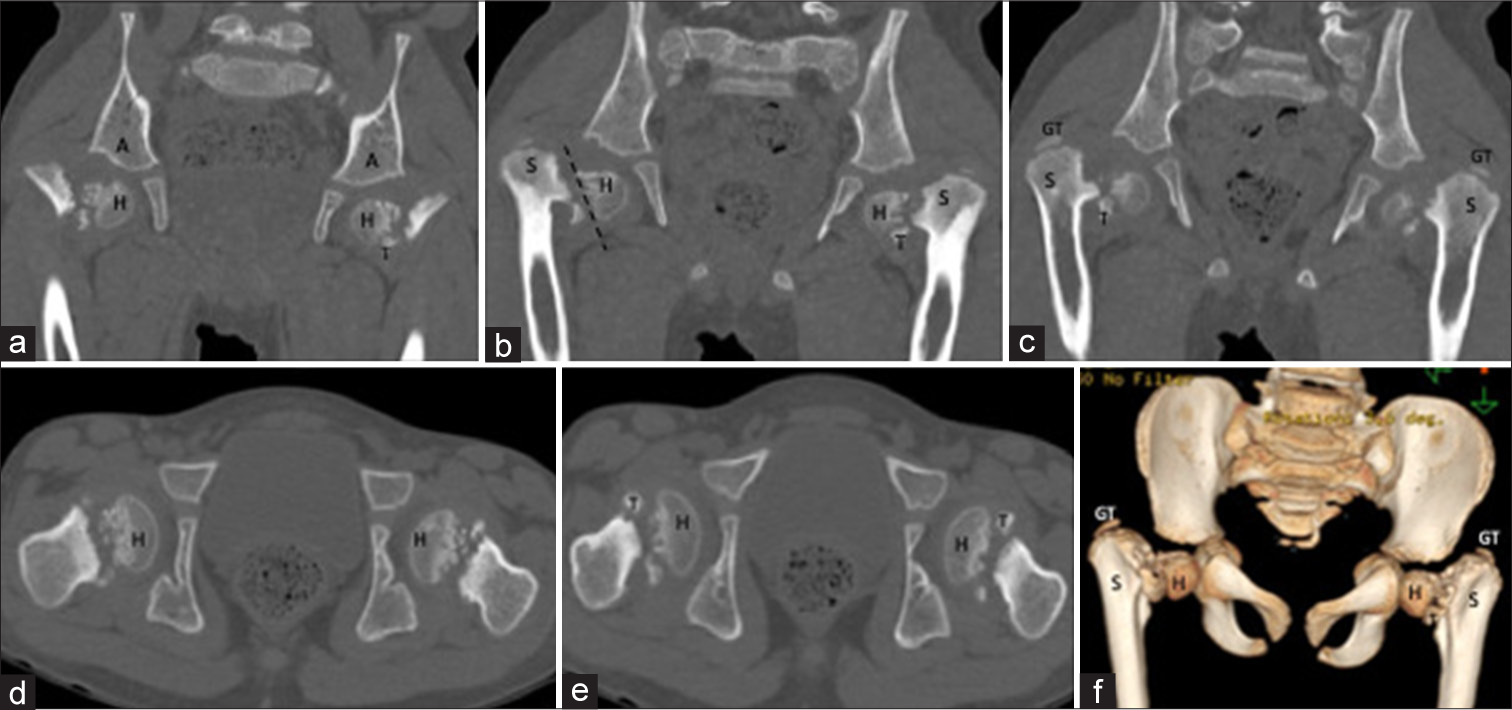
- (a-f) Computed tomography images of the patient. (a-c) Serial coronal sections from anterior to posterior, (d and e), serial axial images from superior to inferior, and (f) volume rendered image showing severe bilateral developmental coxa vara. Widening, irregularity and near vertical orientation of the growth plates (dotted line in b) were noted. Inverted Y-shaped ossification defects/triangular metaphyseal fragments (T) were seen at the inferior aspect of the region of femoral neck bilaterally. The femoral neck appeared short and deformed bilaterally. Both acetabuli (A) showed normal development with no sign of dysplasia. The femoral shafts (S) were displaced postero-supero-laterally. The femoral heads (H) appeared osteopenic and showed irregularity and sclerosis at their lateral aspects. The greater trochanters were markedly elevated. GT: Greater trochanter
DISCUSSION
The definition of developmental coxa vara includes a decreased femoral neck-shaft angle secondary to osteochondral dysplasia of the femoral neck. The femoral neck fails to develop normally and is replaced by a triangular bone fragment (ununited ossification center) as a result of which the femoral head cannot withstand the mechanical shearing forces of the body weight.[5-7] The femoral shaft, instead of showing the normal superomedial growth, continues growing in upward direction only, while the unsupported femoral head keeps sinking downwards under the pressure of the body weight [Figure 1].[4] Consequently, the femoral neck-shaft angle continues decreasing with the child’s ambulation and weight-bearing and eventually a limp or waddle ensues. Bilateral involvement is seen in about 30% of the cases.[2] Diagnosis is usually made on radiographs which reveal reduced femoral neck-shaft angle, nearly vertical orientation of the growth plate, juxtametaphyseal-epiphyseal irregularity, and a distinctive triangular bone fragment (inverted Y-shaped ossification defect) located inferiorly in the area of the growth plate.[1] The GTs and femoral shaft become markedly elevated in advanced disease. CT is needed for deformity configuration, assessment of bone stock, and physeal widening and for proper surgical planning. Management depends on the severity of the disease. Mildly symptomatic cases with slight varus deformity and minimal osseous defects may be managed by observation alone and close follow-up. The surgical treatment of choice in severely dysplastic hips is corrective valgus derotation osteotomy/subtrochanteric osteotomy at an early age (6–8 years) with the aim of correction of varus deformity and restoring the growth plate at a more horizontal position, thereby eliminating the abnormal shearing forces of weight-bearing that affect normal growth.[1,8] If improved alignment of weight-bearing is achieved, the femoral neck subsequently ossifies with improvement of symptoms, gait and limb length which can be assessed with follow-up radiographs and clinical examinations.
CONCLUSION
Developmental coxa vara is an unusual cause of childhood limp resulting from femoral neck development. The biomechanics of the hip region are so profoundly altered that serious disability ensues in the childhood or early adolescence unless recognized early and managed appropriately. Imaging plays a key role in early detection of the pathology and for surgical planning. Prompt and early management leads to good results, whereas untreated cases often advance to crippling disabilities.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Congenital coxa vara, osteochondrodysplasia of the femoral neck. Radiology. 1954;63:59-63.
- [CrossRef] [PubMed] [Google Scholar]
- A case of infantile coxa vara: With notes on the ætiology. Lancet. 1935;225:1498-500.
- [CrossRef] [Google Scholar]
- Congenital coxa vara: Computed tomographic analysis of femoral retroversion and the triangular metaphyseal fragment. J Pediatr Orthop. 2000;20:551-6.
- [CrossRef] [PubMed] [Google Scholar]
- Shear strength of the human femoral capital epiphyseal plate. J Bone Joint Surg Am. 1976;58:94-103.
- [CrossRef] [PubMed] [Google Scholar]
- Slipped capital femoral epiphysis: Factors affecting shear forces on the epiphyseal plate. J Pediatr Orthop. 1984;4:745-8.
- [CrossRef] [PubMed] [Google Scholar]







