Translate this page into:
Central groin pain: A pictorial review

*Corresponding author: Abhishek Milind Patil, InnoVision Imaging, Mumbai, Maharashtra, India. abhishekpatil190@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil AM, Lawande MA, Ahuja A, Daftary A. Central groin pain: A pictorial review. Indian J Musculoskelet Radiol. doi: 10.25259/IJMSR_42_2024
Abstract
Pubic symphysis pathologies are one of the common causes of groin pain. This pictorial review illustrates the common pathologies involving pubis symphysis along with a step-by-step approach to diagnose them.
Keywords
Pubic symphysis
Central groin pain
athletic pubalgia
osteitis pubis
pubic diastasis
INTRODUCTION
The articular cartilage, pubic bones, and myotendinous attachments of adductor group of muscles and anterior abdominal wall muscles stabilize the pubic symphysis. The pubic bone is divided into three parts, namely, body, superior, and inferior pubic rami. The medial margins of pubic body are covered by hyaline cartilage and fibrocartilaginous disc is located in between [Figure 1].[1]
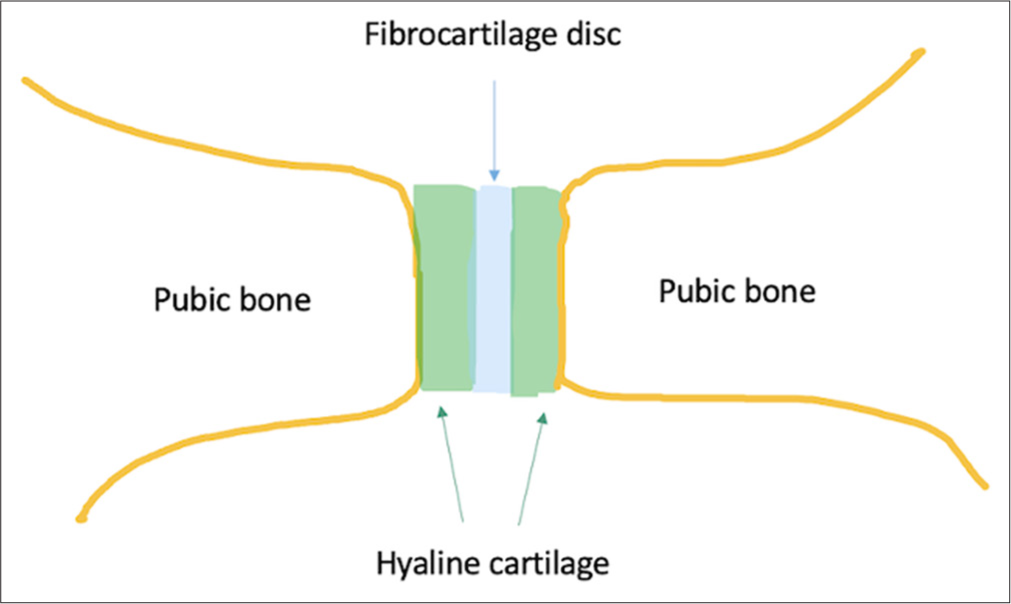
- Schematic presentation of the pubic symphysis joint.
Pubic symphysis is reinforced by [Figure 2].
Ligaments: Superior, inferior, anterior, and posterior ligaments
Myotendinous structures: Adductor group, rectus abdominis, and anterior abdominal wall muscles.[2]
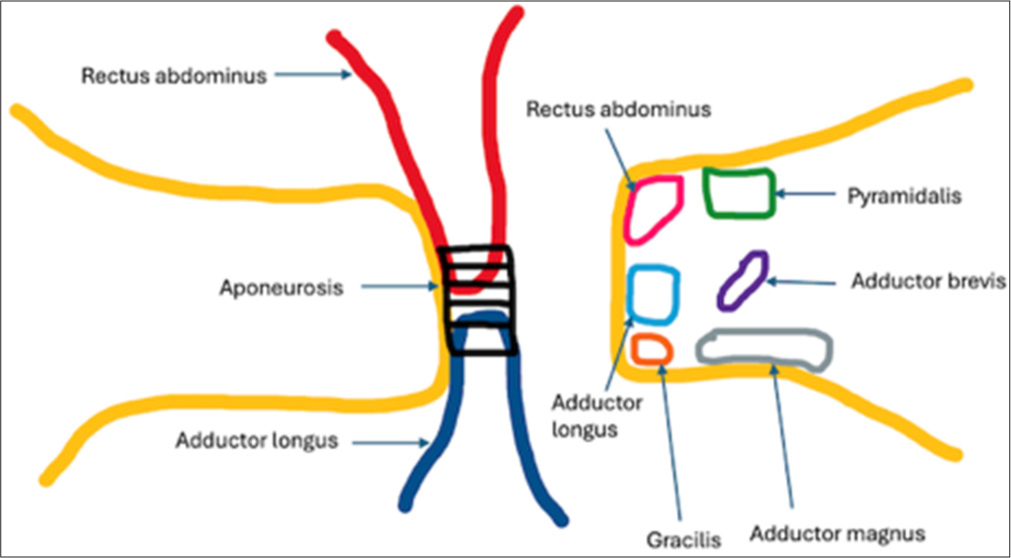
- Schematic diagram of pubic symphysis muscle attachments.
The inferior pubic ligament is the most crucial ligament with respect to the stability. The inferior pubic ligament merges with adductor aponeurosis and gracilis muscle.
Superiorly, the pubic symphysis is reinforced by anterior and anterior lateral abdominal wall muscles. The inferior rectus and rectus sheath provide support superiorly and anteriorly. The rectus muscle attachment is divided into the medial and lateral heads. The lateral head arises from the pubic crest and merges with adductor longus tendon. The medial head blends with anterior ligament. Laterally, the pubic symphysis anterior aponeurosis ligamentous complex blends with inguinal canal ligaments. The anterior wall of the inguinal canal is formed by external oblique aponeurosis and blends with the aponeurotic sheath. The posterior wall of the inguinal canal is formed by fascia transversalis, internal oblique, and transversus abdominus muscles and they merge with the anterolateral rectus sheath.
The pubic symphysis is inferiorly enforced by adductor group of muscles which include adductor longus, brevis, magnus, gracilis, and pectineus; adductor longus being the most important dynamic stabilizer. The adductor longus tendinous attachment blends with the periosteum, crosses midline, and blends with each other. The adductor aponeurotic fascia merges with the anterior rectus sheath [Figures 3 and 4].
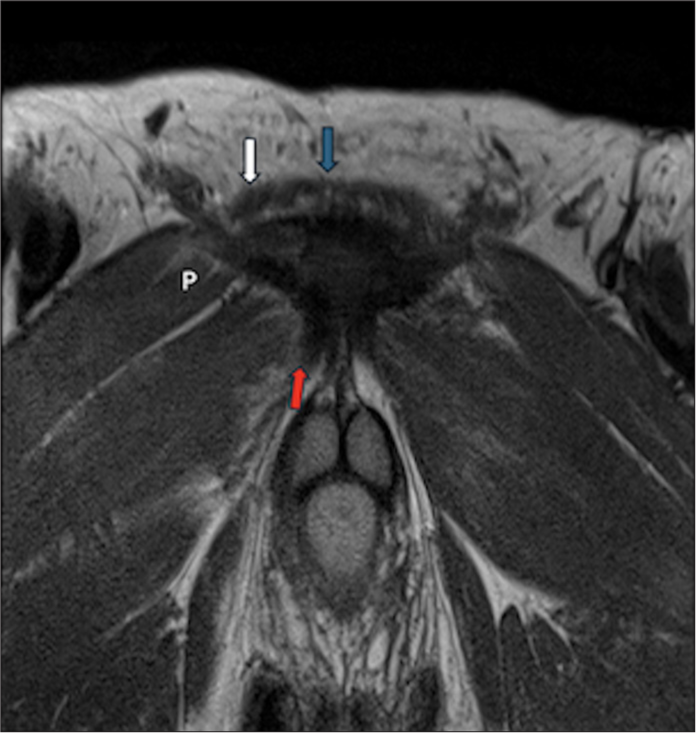
- Proton density (PD) oblique coronal image demonstrates rectus abdominus tendinous attachment superiorly (blue arrow medial head and white arrow-lateral head). The adductor longus tendinous attachment is seen inferiorly (red solid arrow). The pectineus muscle is marked by P.
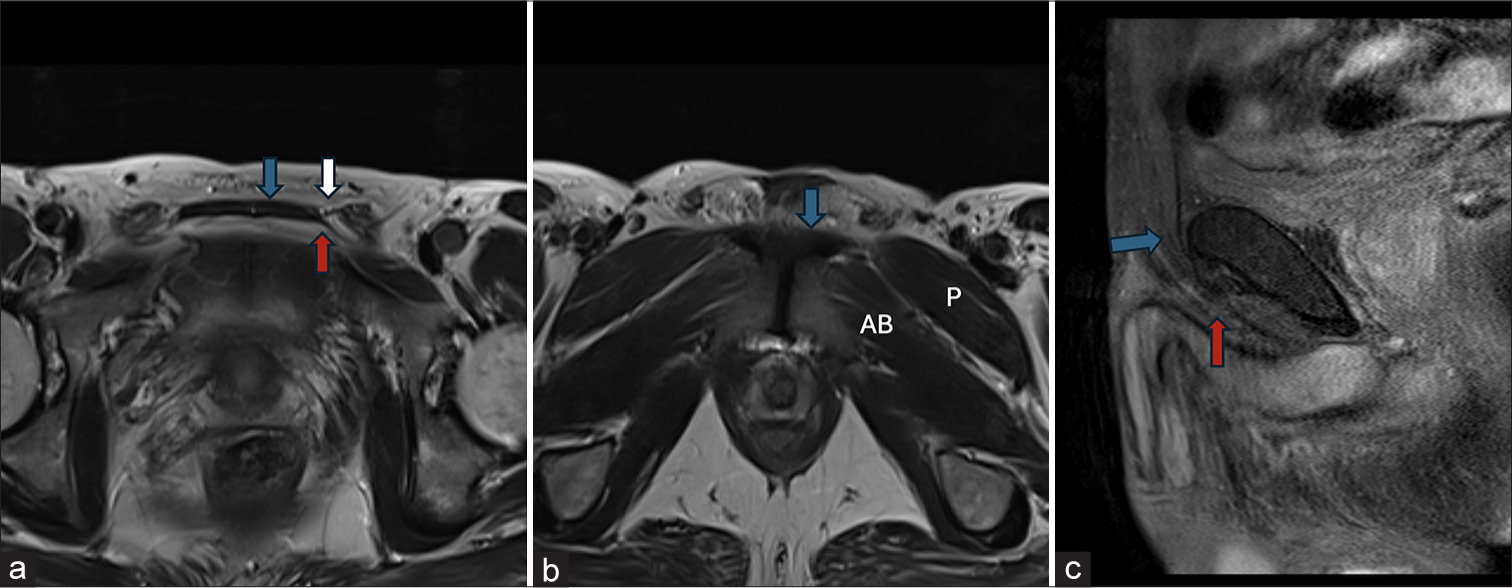
- Proton density (PD) axial image through superior aspect of pubic symphysis (a) demonstrates inferior rectus muscle (blue arrow), anterior wall of inguinal canal made of external oblique aponeurosis (white arrow) and posterior wall of inguinal canal blending with anterior rectus sheath (red arrow) PD axial image through inferior pubic symphysis, (b) demonstrate adductor longus tendinous attachment (blue arrow), pectineus muscle (P) and adductor brevis (AB) Proton density fat saturation (PD FS) oblique sagittal image through pubic symphysis, (c) demonstrates anterior rectus sheath (blue arrow) blending with adductor aponeurotic fascia (red arrow).
A systematic radiological assessment of these structures offers insights into the altered biomechanics and stability of the joint.[2]
The pubic symphysis pathologies are grouped into the following [Figure 5]:
Traumatic: Pelvic bones fracture, myotendinous avulsion, pubic diastasis, athletic pubalgia, pubic stress fractures, and osteitis pubis
Infectious
Inflammatory: Secondary to spondyloarthropathy
Neoplastic.
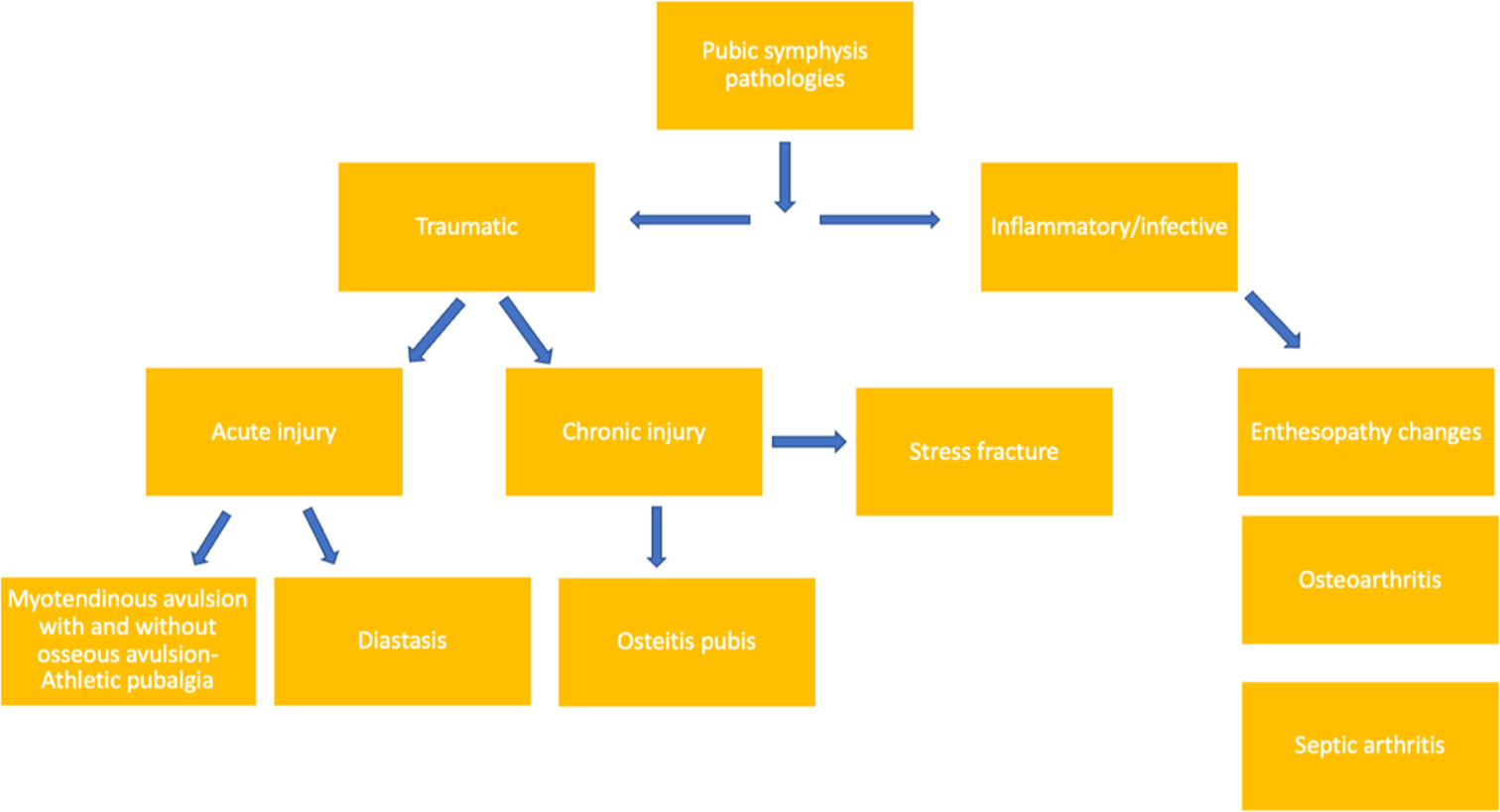
- The pubic symphysis pathologies are grouped as mentioned.
The traumatic injuries can be acute such as fractures or myotendinous avulsions or pubic diastasis or they can be sequelae to persistent microtrauma leading to stress edema or fracture and osteitis pubis.
Inflammatory and infective involvement of pubic symphysis demonstrates marrow edema with or without erosions and synovitis. Magnetic resonance imaging (MRI) is definitely helpful in differentiating between infective and inflammatory etiologies. MRI provides earlier radiological evidence of infection than radiographs or computed tomography (CT) scans.
DISCUSSION
Trauma
Injuries occurring at the level of the pubic symphysis can be either acute or chronic injuries. Acute injuries may manifest as osseous or soft-tissue injuries or both.
Osseous injuries can be part of traumatic pelvic rim fractures or stress or insufficiency fractures.
Violent trauma such as road traffic accidents leads to an open book fracture, there is pubic diastasis associated with sacroiliac joint widening, sacral ala, and posterior ilium fractures. In a bucket handle fracture, there is ipsilateral superior and inferior pubic rami fracture and contralateral sacroiliac joint disruption. In a case of “windswept fracture,” there is a unilateral open book pattern of injury.
Elderly patients are more susceptible for insufficiency fractures, which occur as a result of normal stress on underlying weaker or abnormal bone. Factors such as osteoporosis, osteomalacia, previous radiation therapy, long-term exposure to oral corticosteroid therapy, renal failure, or altered mechanics following hip arthroplasty contribute to this vulnerability.[3]
Myotendinous injuries are commonly observed in young athletes, often associated with osseous avulsions. These athletes may present with lower abdominal pain or groin pain attributed to prolonged stress on the rectus abdominis-adductor aponeurosis, leading to tear, periosteal stripping, or osseous avulsion.
Pubic diastasis is frequently observed in postpartum cases.
Case 1: Athletic pubalgia
Periosteal stripping refers to the separation or lifting of the periosteum, which is the dense fibrous membrane covering the surface of bones. The adductor aponeurosis is a thin, fibrous structure that connects the tendons of the adductor muscles to the bone. Periosteal stripping can occur due to trauma or repetitive stress. This process can lead to inflammation and pain.
Athletes, particularly those involved in sports that require sudden changes in direction, kicking, or twisting movements, such as soccer, hockey, football, and rugby are highly prone for pubic symphysis injuries.[4]
The adductor longus helps in adduction and stabilization of the pelvis during movements such as walking and running. The rectus abdominis muscle is located vertically in the anterior abdominal wall and is involved in flexing the trunk and stabilizing the pelvis.
Adductor and rectus femoris muscle or tendinous tears can disrupt the balance of forces around the pelvis, leading to altered biomechanics and instability across the anterior pelvis. The weakening of the common aponeurosis, a sheet of connective tissue where multiple muscles converge, can further compromise stability.
A torn unopposed tendon can weaken the aponeurosis, and repeated stress can lead to degeneration and eventually a tear through the aponeurosis. This tear can extend into the adductor tendons, further compromising stability. The destabilization can then affect neighboring muscles such as the pectineus and adductor brevis, ultimately resulting in an unstable pubic symphysis.
This sequence of events highlights the interconnectedness of muscles and connective tissues around the pelvis and underscores the importance of maintaining proper biomechanics and addressing injuries promptly to prevent further complications.
In young athletes due to sudden strain, there is periosteal stripping of rectus abdominis-adductor longus aponeurosis which leads to chronic lower abdominal pain. In the past, it was referred to as sportsman’s hernia which is a misnomer as there is no hernia.[5]
Diagnosis is often confirmed through imaging studies, such as MRI which can reveal changes in the periosteum, soft tissues, and bone. Ultrasound can be useful to evaluate the adductor origins.
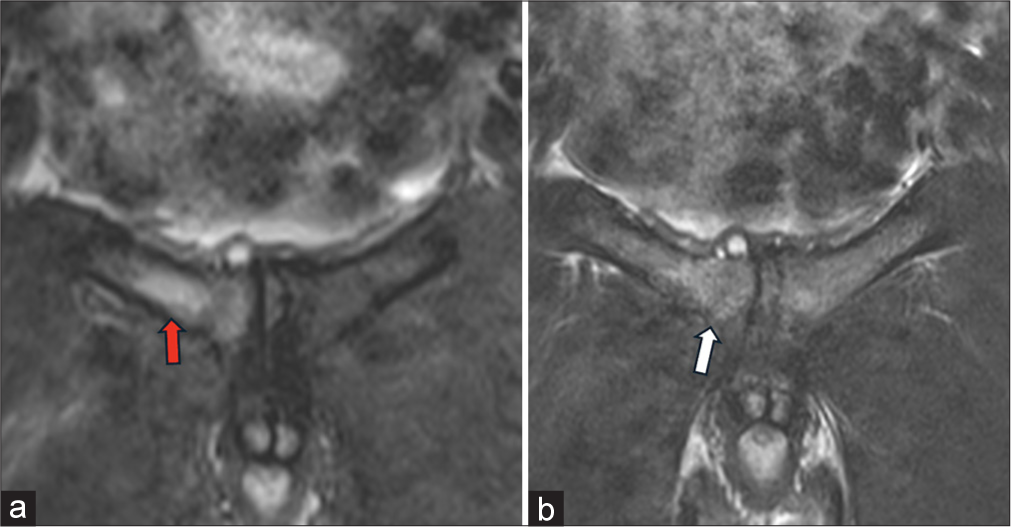
MRI images are acquired parallel and perpendicular to the pubic symphysis, a fluid cleft may be seen under the surface of the aponeurosis with adjoining marrow edema. Sometimes, there can be associated osseous avulsion which can be retracted or non-displaced [Figure 6].
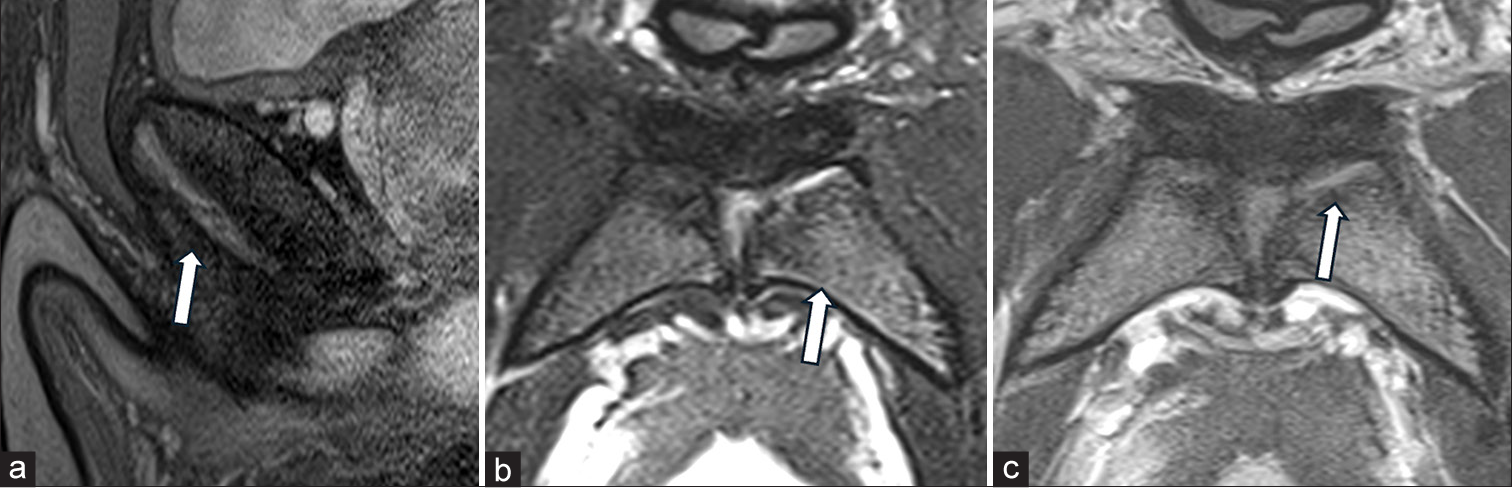
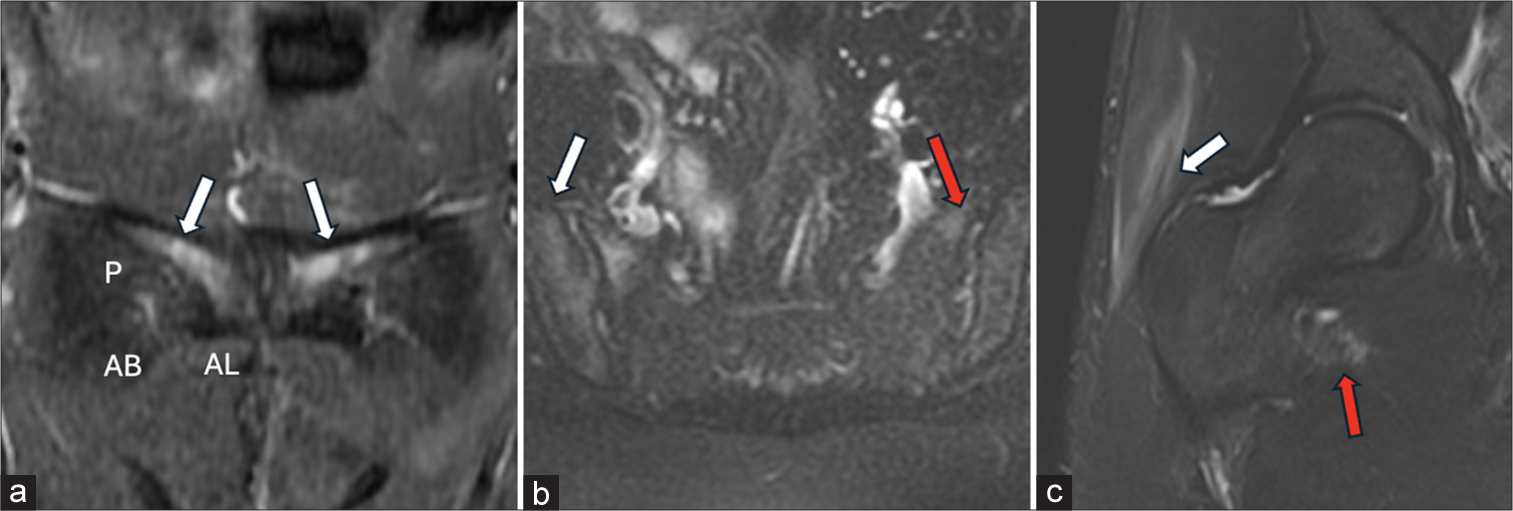
- (a) Sagittal fat sat T2, (b) oblique axial fat sat T2 and (c) oblique axial PD images show periosteal stripping of the left adductor aponeurosis (white arrow in a and c) at the anterior pubic symphysis attachment with underlying left pubic marrow edema (white arrow in b).
Case 2: Osseous avulsion
The adductor longus contributes to the adduction of the hip joint and adductor longus tendinous attachment with aponeurosis provides anterior stability. Osseous avulsion yields a fragment of bone detached from its normal attachment due to the force generated by the muscle’s contraction. Diagnosis is typically confirmed through imaging studies, such as X-rays or MRI, which can reveal the avulsed bone fragment and assess the extent of the soft-tissue injury [Figure 7].[5]
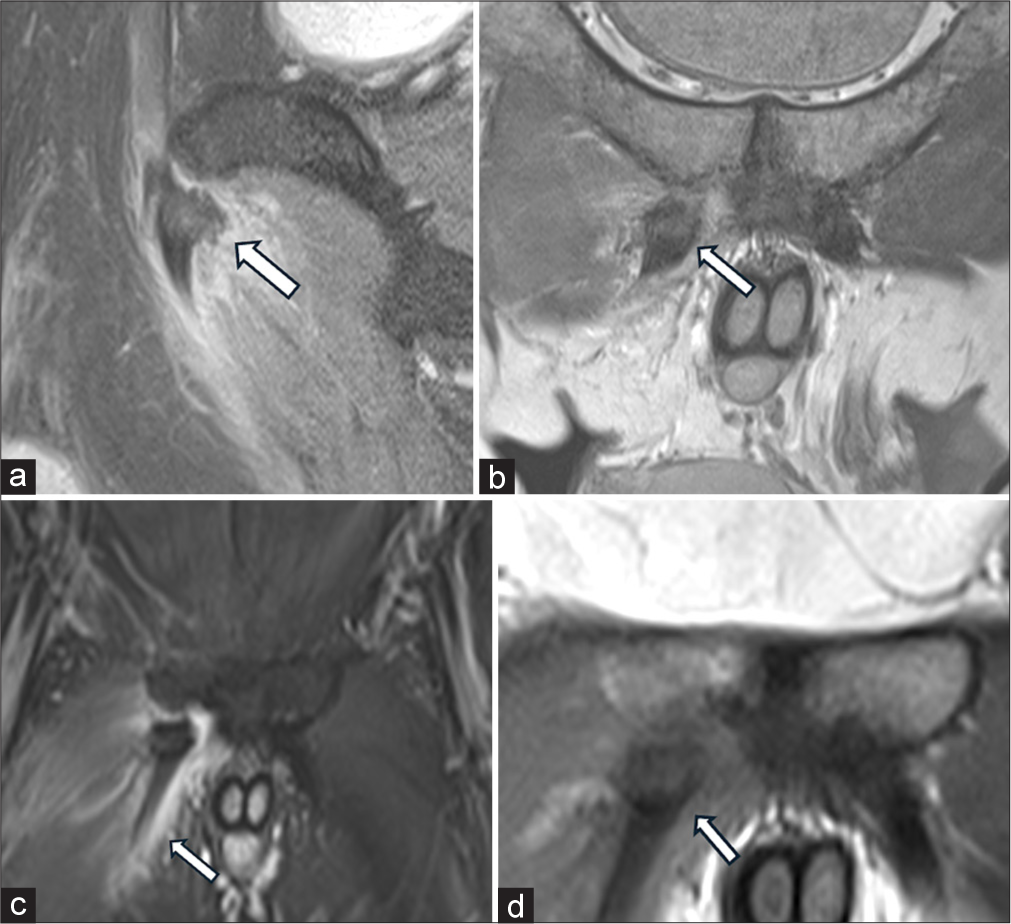
- MR images (a) oblique sagittal fat sat. (b and d) coronal PD and (c) coronal T2 fat sat MR images through pubic symphysis demonstrate a discrete osseous avulsion (white arrow in a, b and d) originating from the undersurface of the right adductor longus attachment. This avulsion is accompanied with retraction and marked intramuscular edema (white arrow in c).
Case 3: Pubic diastasis
Pubic diastasis is attributed to elevated ovarian and placental hormones, resulting in physiological pelvic ligament relaxation and fibrocartilaginous disc changes that alter the biomechanics at the level of the pubic symphysis. In some cases, this progression may lead to chronic stress, eventually leading to osteitis pubis. A pubic symphysis widening >10 mm is considered pathological and clinically presents with symptoms such as suprapubic pain. Pubic diastasis may also be seen in trauma due to rupture of the supporting ligaments [Figure 8].[6]
- (a) T2 coronal, (b) oblique axial STIR and (c) oblique axial T2w MR images demonstrate post partum widening of the pubic symphysis (white arrow in a and c). There is moderate marrow edema and soft tissue edema (white arrow in b), consistent with pubic diastasis.
Case 4: Insufficiency fractures
These fractures result from repetitive stress on weakened bone.
Etiology
These fractures often occur due to repetitive stress on the pubic symphysis, particularly in individuals with osteoporosis or osteomalacia. Pregnancy-related changes and medical conditions that affect bone density can also be contributing factors.
Trivial trauma can result in insufficiency fractures if the underlying bone is weak. These fractures are commonly seen in cases of Vitamin D3 deficiencies. Other less common etiologies include chronic renal failure, long-term exposure to oral corticosteroids, or patients of radiotherapy. Rarely in a case of total hip arthroplasty with poor rehabilitation, there are altered biomechanics which leads to chronic stress over pubic symphysis and predisposes it to stress reactions or insufficiency fractures.[3]
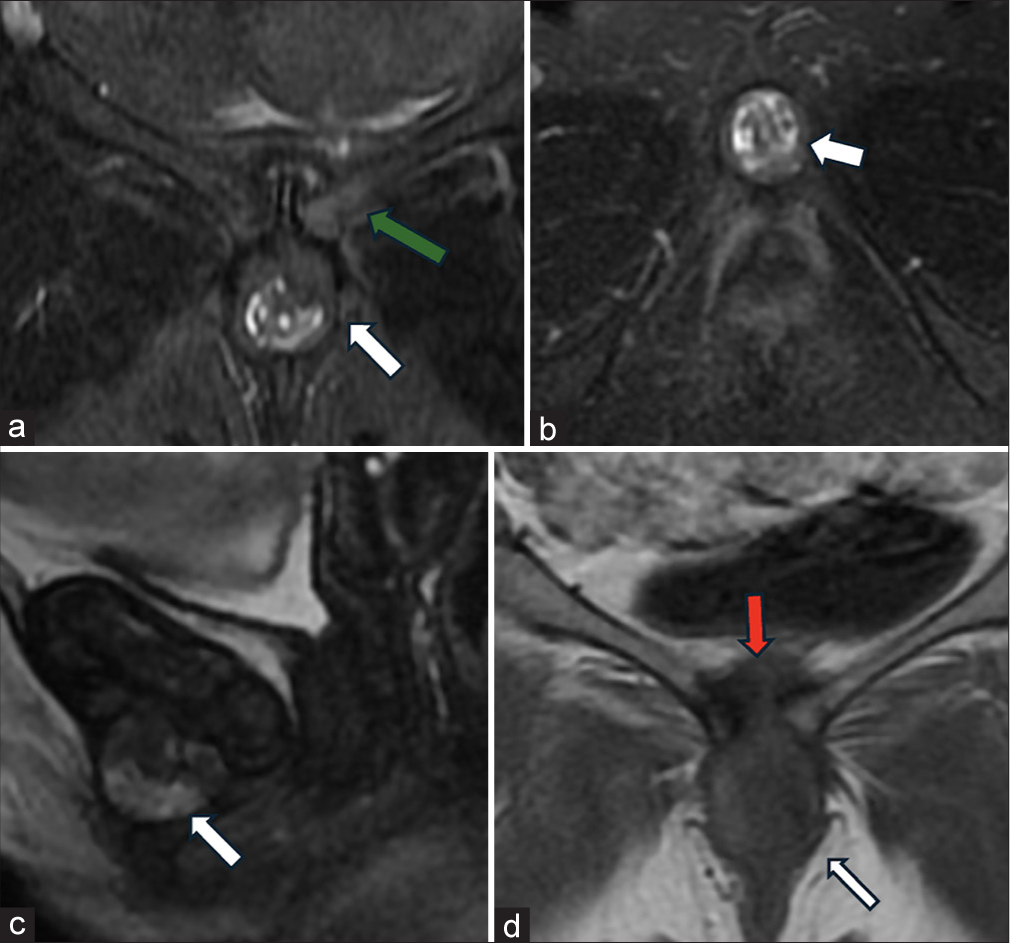
Radiographic imaging, such as X-rays or MRI, may reveal fractures and MRI also reveals marrow edema [Figure 9].

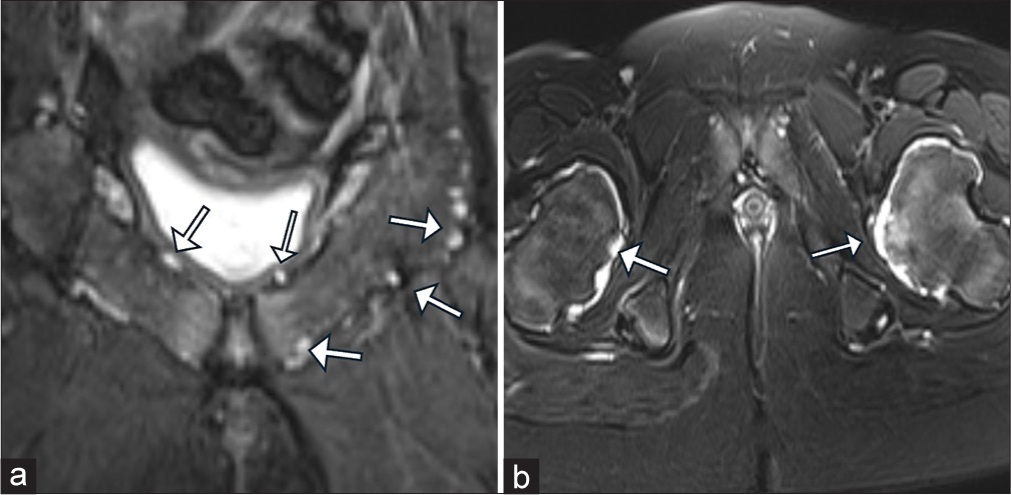
- (a,b) Red arrow only shows fracture line of left superior pubic ramus and white arrow only shows right pubic marrow edema. Oblique coronal T2 (c) Fat saturation and (d) T1 images demonstrate incomplete insufficiency fractures with marrow edema (white arrows in c and d) involving the bilateral sacral ala. Notably, there is no associated fluid collection.
Case 5: Pubic symphysis stress fracture
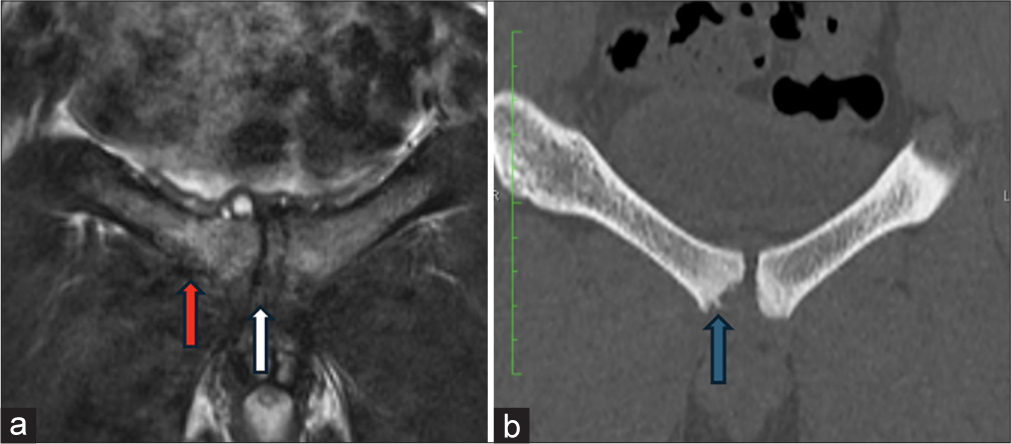
Perisymphyseal pubic bone stress fractures often occur due to activities that place repeated strain on the pelvis, such as running, jumping, or certain athletic activities. Diagnosis is often confirmed through imaging studies, such as X-rays or MRI. X-rays may initially appear normal or show subtle changes, while MRI can reveal the presence of early stress edema as well as frank fractures [Figure 10].[7]
- (a) Oblique coronal T2 fat saturation and (b) proton density images through pubic symphysis demonstrates an evolving right perisymphyseal pubic bone stress fracture (white arrow in b) with marrow edema (red arrow in a).
Case 6: Pubic symphysis degenerative cyst
Pubic symphysis osteoarthrosis or degenerative changes lead to fluid accumulation which, in turn, leads to capsular/ synovial cyst formation. There is cartilaginous wear and tear with joint fluid extending into the cartilaginous cyst which extends into the space of Retzius. These cysts can be suprapubic, retropubic, or sub/infrapubic. Subpubic cyst may extend posteroinferiorly at the level of vagina leading to dyspareunia or lower urinary tract symptoms or acute urinary retention. Retropubic or suprapubic cyst can have a mass effect on the urinary bladder with stress incontinence [Figure 11].[8]
- (a) Oblique coronal, (b) axial fat saturation T2, (c) sagittal and (d) coronal T1 images demonstrate a capsulated infrapubic lesion with mixed signal intensity (white arrow in a-d), accompanied by mild widening of the pubic symphysis (red arrow in d), mild parasymphyseal marrow edema (green arrow in a), and degenerative changes. Additionally, there is evidence of reactive synovial thickening. These observations are consistent with a diagnosis of a degenerative infrapubic cartilaginous cyst.
Case 7: Osteitis pubis
Osteitis pubis is a condition characterized by inflammation of the pubic symphysis, which can lead to pain and discomfort in the pelvic region, particularly during activities that involve movement of the pelvis or stress on the joint.[9] Osteitis pubis is often associated with repetitive stress, overuse, or microtrauma to the pubic symphysis.[10] It can occur in athletes, particularly those involved in sports that require frequent changes in direction, such as soccer, hockey, or running.[11] Diagnosis is typically confirmed through imaging studies, such as X-rays, MRI, or CT scans. These imaging modalities can reveal irregularities and marrow edema along the pubic symphysis [Figure 12].[5]
- (a) Oblique coronal fat saturation T2 image demonstrates pubic symphysis chondral loss (white arrow in a) with parasymphyseal bone marrow edema (red arrow in a) involving the adjacent superior pubic ramus and (b) CT scan demonstrates subcortical irregularity (blue arrow in b).
Osteolysis
Osteolysis is the process of bony resorption and breakdown. Osteolysis is multicausal with inflammatory and mechanical stress being the most common factors contributing to it. It can be associated with superadded infections and pathological fractures. This leads to structural instability. It can be associated with large collection or heterotopic ossification which, in turn, can lead to mass effect on the bladder or pelvic viscera [Figure 13].
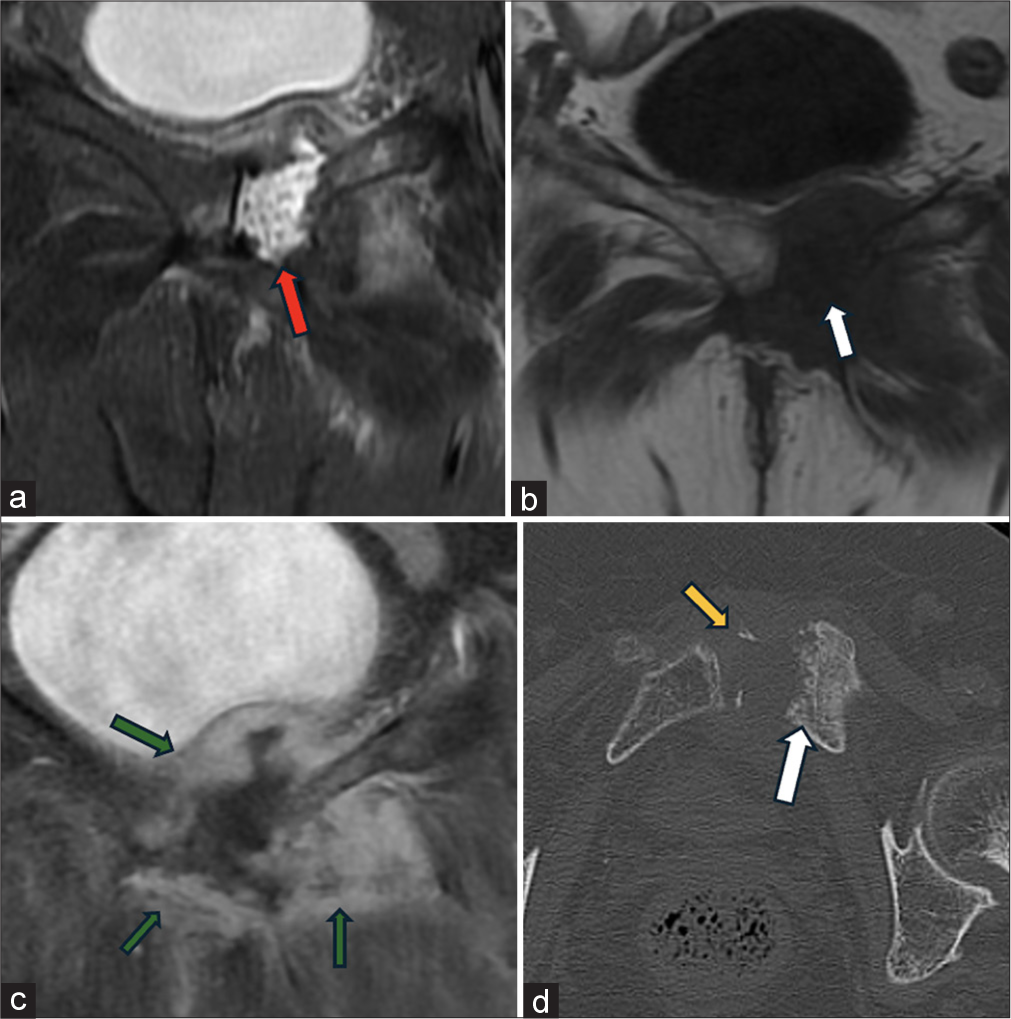
- (a) Oblique coronal fat saturation T2 and (b) T1 images demonstrate left perisymphyseal pubic bone resorption (white arrow b) with associated widening of the pubic symphysis filled with hyperintense fluid pocket (red arrow in a). (c) Post contrast image demonstrates centrally placed peripherally thick enhancing area of osteolysis (green arrows in c). (d) Axial CT image demonstrates parasymphyseal erosions (white arrow in d) and few peripherally placed heterotopic ossifications (yellow arrow in d)
Case 8: Infection
Septic arthritis is a serious medical condition characterized by the infection of a joint. Septic arthritis of pubic symphysis demonstrates joint space widening, joint fluid, parasymphyseal marrow, and soft-tissue edema with or without fluid collection. Enlarged inguinal lymph nodes may be associated with it. Post-contrast imaging shows peripheral post-contrast enhancement which helps in delineating the pathology. Joint fluid aspiration or associated soft-tissue biopsy can be performed under ultrasound or CT guidance. This not only helps us in narrowing down to a particular organism but also establishes antibiotic sensitivity.
Common risk factors for septic arthritis include
Recent joint trauma or surgery: Any break in the skin or disruption of the joint can provide an entry point for bacteria.
Pre-existing joint conditions: Conditions such as rheumatoid arthritis, osteoarthritis, or gout can increase the risk of developing septic arthritis.
Invasive procedures: Injections into joints or invasive medical procedures can introduce bacteria into the joint space.
Immunosuppression: Conditions or medications that weaken the immune system can make individuals more susceptible to infections such as diabetes mellitus, long-term exposure to steroids, patients on immunomodulators, patients with HIV-positive status, and post-organ transplant.
Key findings associated with septic arthritis
-
Joint effusion [Figure 14]
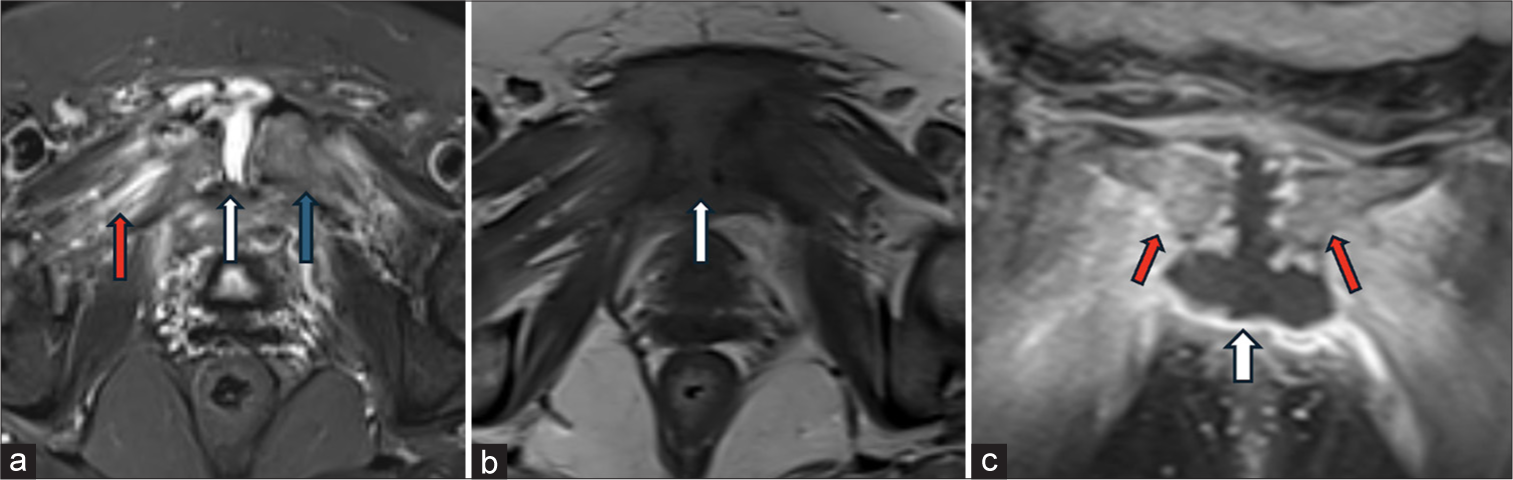 Figure 14:
Figure 14:- (a) Oblique axial T2 Fat saturation and (b) T1 images demonstrate fluid filled widening of pubic symphysis (white arrowsin a-c), mild adjoining marrow edema (blue arrow in a) and moderate adjacent soft tissue edema predominantly involving adductor group of muscles (red arrow in a). The (c) post contrast coronal T1 FS image demonstrates moderate to marked peripherally enhancing joint synovitis and effusion (white arrow c) with enhancing marrow edema (red arrows in c)
Subarticular erosions
Marrow edema
Locoregional lymphadenopathy.
It is crucial to note that septic arthritis requires prompt medical attention and treatment with antibiotics. Early diagnosis and intervention can help prevent long-term joint damage and systemic complications.
Case 10: Inflammatory etiologies
Musculoskeletal manifestations associated with inflammatory spondyloarthropathy or inflammatory arthritis, such as rheumatoid arthritis, may involve the pubic symphysis.
Enthesopathy refers to inflammation or pathological changes at the sites where tendons or ligaments attach to bones. In the context of inflammatory arthritis, enthesopathy changes at the pubic symphysis may involve the insertions of muscles and ligaments around this joint.
In the pubic symphysis, marrow edema may be seen with inflammatory processes associated with arthritis conforming active disease.
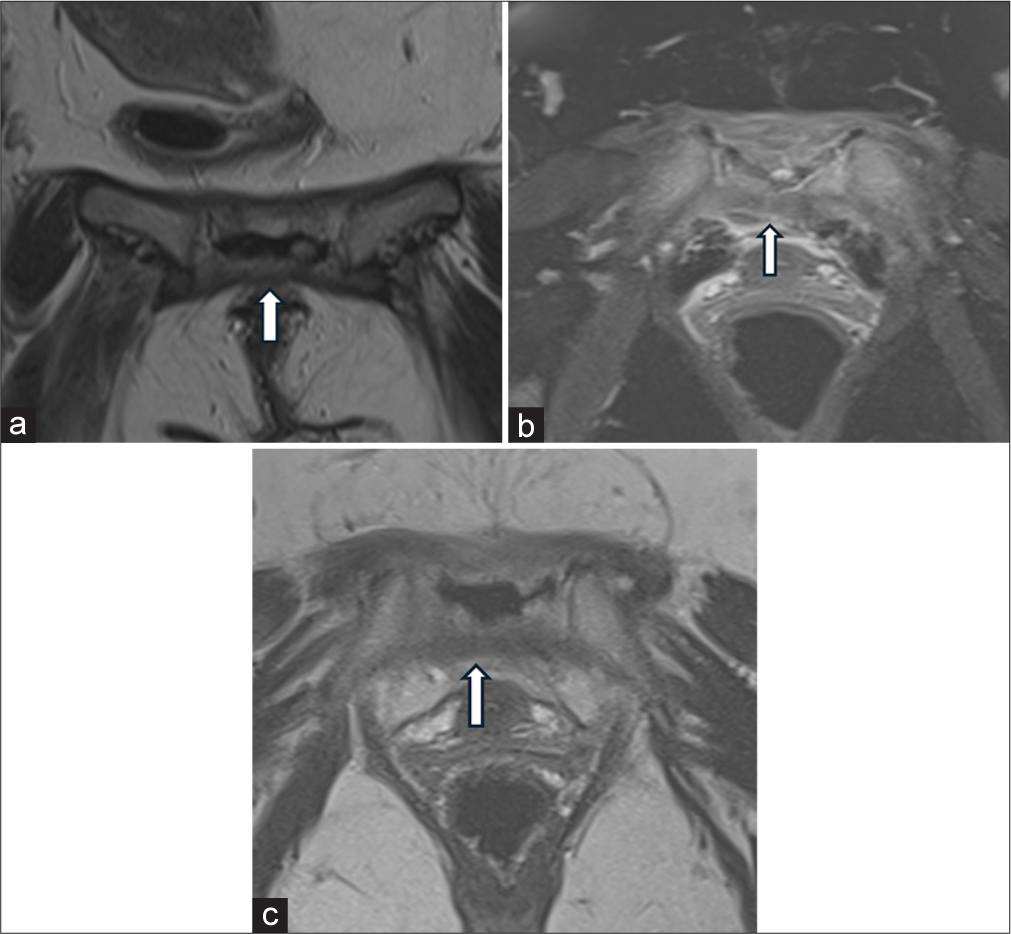
Imaging modalities, such as MRI, are useful to detect active inflammatory changes and aid in the diagnosis and management of inflammatory spondyloarthropathy or arthritis [Figure 15].[9]
- (a) Coronal T2 Fat saturation through pubic symphysis demonstrates pubic body and crest marrow edema (white arrow) at adductor longus (AL), brevis (AB) and pectineus (P) entheseal or attachment site to both sides of midline. (b) Coronal T2 image through sacroiliac joints demonstrates bilateral sacroiliac joint marrow edema right (white arrow) more than left (red arrow in b) and (c) Coronal T2 FS images through right hip joint demonstrates peritrochanteric edema (white arrow) and iliopsoas tendinosis at lesser trochanter attachment (red arrow), collectively suggest inflammatory arthropathy and enthesopathy.
Neoplasms
Pubic symphysis neoplasms are rare, and the most common types are cartilaginous tumors or metastatic lesions. Cartilaginous tumors, such as chondrosarcoma, may arise in the pubic symphysis.[12]
Evaluation and diagnosis of pubic symphysis neoplasms often involve imaging studies such as X-rays, CT scans, and MRI, as well as biopsy for definitive diagnosis. Management and treatment strategies depend on the type of neoplasm, its location, and other individual factors.
Case 11
Hereditary multiple osteochondromas (HMO), also known as multiple hereditary exostoses, is a rare genetic disorder characterized by the development of multiple benign bony outgrowths called osteochondromas. These growths typically arise near the ends of long bones, such as the femurs and humerus, and can also affect the pelvic bones. HMOs are inherited in an autosomal dominant manner, meaning that an affected individual has a 50% chance of passing the condition on to each of their children. While the majority of osteochondromas associated with HMO are benign, they can cause various complications, such as pain, deformity, and restricted joint movement [Figure 16].
- (a) Oblique coronal and (b) axial T2 Fat saturation images through pubic symphysis and bilateral femoral neck demonstrates multiple diffuse osteochondromas (white arrows in a and b) scattered throughout the pelvic bones and femoral necks.
Case 12: Round cell neoplasm
Round cell neoplasm is an aggressive neoplasm seen in younger/pediatric age group. The lesion is characterized by expansile bone destruction demonstrating T2 hyperintensity, T1 hypointensity, and heterogenous post-contrast enhancement with associated soft-tissue components [Figure 17].
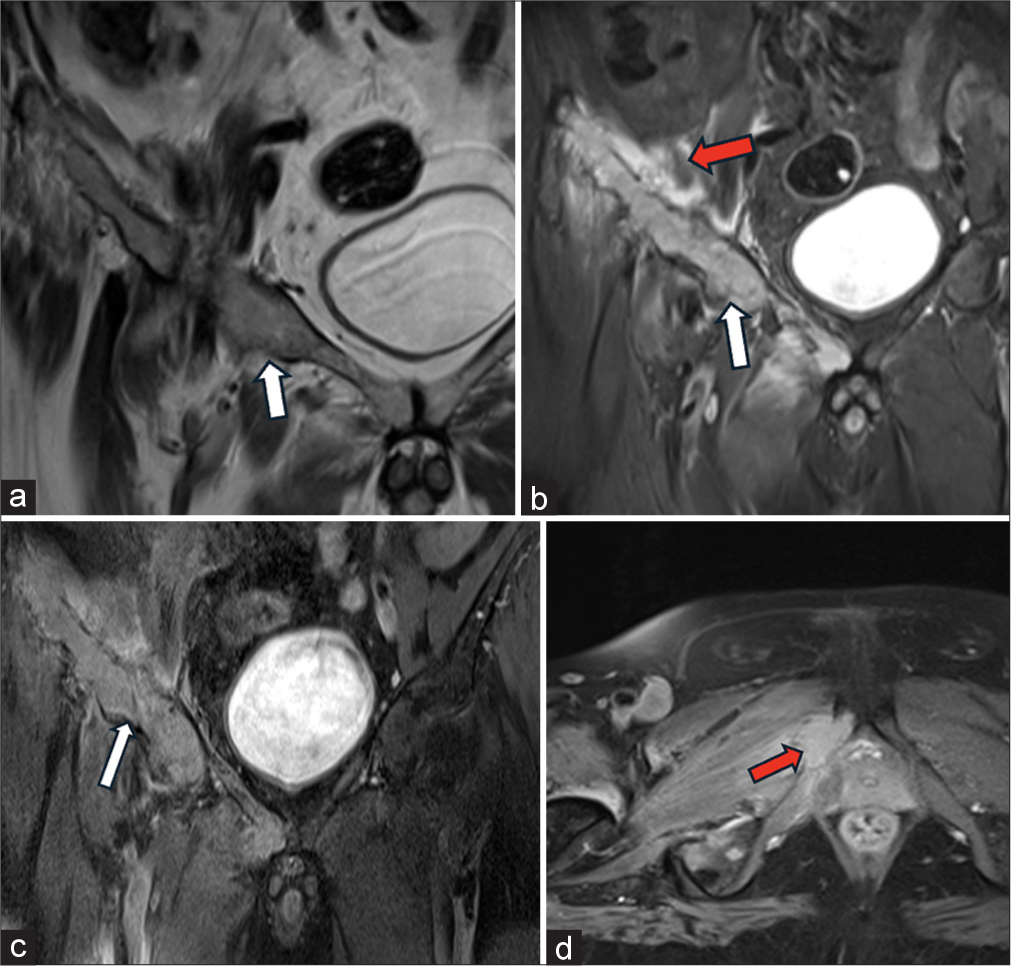
- (a) Oblique coronal T2 and (b) T2 FS images demonstrate expansile lesion (white arrow in a and b) involving iliac bone, anterior acetabulum, superior and inferior pubic rami with associated soft tissue edema (red arrow in b). Post contrast (c) coronal and (d) axial T1 Fat saturation demonstrates intensely enhancing lesion (white arrow in c) with enhancing soft tissue component (red arrow in d).
CONCLUSION
A thorough knowledge of the anatomy allows accurate interpretation of the imaging studies and clinical findings. An accurate diagnosis and appropriate management contribute to better patient outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Pictorial essay diseases of the pubis and pubic symphysis: MR imaging appearances. 1997 Available from: https://www.ajronline.org [Last accessed on 2024 Aug 24]
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of the pubic symphysis: Anatomy and pathologic conditions. Radiographics. 2023;43:e220058.
- [CrossRef] [PubMed] [Google Scholar]
- MRI and CT of insufficiency fractures of the pelvis and the proximal femur. Am J Roentgenol. 2008;191:995-1001.
- [CrossRef] [PubMed] [Google Scholar]
- Pubic apophysitis in elite Australian Rules football players: MRI findings and the utility of VIBE sequences in evaluating athletes with groin pain. Clin Radiol. 2020;75:293-301.
- [CrossRef] [PubMed] [Google Scholar]
- Patterns of bone and soft-tissue injury at the symphysis pubis in soccer players: Observations at MRI. AJR Am J Roentgenol. 2007;188:W291-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pubic symphysis diastasis: Imaging and clinical features. Eur J Radiol Extra. 2006;59:127-9.
- [CrossRef] [Google Scholar]
- MRI findings in athletic groin pain: Correlation of imaging with history and examination in symptomatic and asymptomatic athletes. Skeletal Radiol 2024
- [CrossRef] [PubMed] [Google Scholar]
- Imaging in retropubic cartilaginous cyst. Indian J Musculoskelet Radiol. 2022;4:103-6.
- [CrossRef] [Google Scholar]
- Pathology of pubic symphysis - What radiologist should know? In: ECR Poster Number: C-08782. Austria: European Society of Radiology; 2020.
- [Google Scholar]
- Radiological findings in symphyseal and adductor-related groin pain in athletes: A critical review of the literature. Br J Sports Med. 2013;47:611-9.
- [CrossRef] [PubMed] [Google Scholar]
- Athletic pubalgia. 2010. Available from: https://radsource.us/wp-content/uploads/2010/02/1a.jpg [Last accessed on 2024 Aug 24]
- [Google Scholar]
- Bone and soft tissue tumors of hip and pelvis. Eur J Radiol. 2012;81:3793-801.
- [CrossRef] [PubMed] [Google Scholar]







