Translate this page into:
Periosteal desmoid tumor: A benign-appearing lesion manifesting as smooth metaphyseal scalloping of the femur on plain radiography

*Corresponding author: Sonal Saran, Department of Diagnostic and Interventional Radiology, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India. sonalsaranmalik@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Handa S, Prajapati T, Phulware RH, Saran S. Periosteal desmoid tumor: A benign-appearing lesion manifesting as smooth metaphyseal scalloping of the femur on plain radiography. Indian J Musculoskelet Radiol. doi: 10.25259/IJMSR_40_2024
Abstract
“Desmoid tumors,” also known as “aggressive fibromatosis,” are rare mesenchymal neoplasms characterized by a fibrotic texture. Despite their non-metastatic nature, these tumors can lead to significant morbidity and mortality due to their tendency to recur locally and involve nearby organs. When these tumors affect bone, they are referred to as desmoplastic fibromas. This case report involves a 26-year-old male who presented with pain and tenderness in the right popliteal fossa. Diagnostic imaging and histopathology confirmed the presence of a periosteal desmoid tumor. Desmoid tumors have an incidence of 2–4 cases per million annually, with a slight female predominance, and typically arise in the third and fourth decades of life. Younger patients tend to experience more aggressive forms of the disease with higher recurrence rates. Histologically, these tumors consist of uniform spindle cells and fibroblasts within a dense collagenous stroma and exhibit distinct immunohistochemical profiles. Imaging, including ultrasound, computed tomography, and particularly magnetic resonance imaging (MRI), plays a critical role in the evaluation of these tumors, with MRI being the preferred modality. Management strategies include observation for stable tumors and intervention for symptomatic cases, with a growing preference for conservative treatment approaches.
Keywords
Aggressive fibromatosis
Desmoid tumors
Magnetic resonance imaging
Mesenchymal neoplasms
INTRODUCTION
“Desmoid tumors,” also known as “deep or aggressive fibromatosis,” are rare mesenchymal neoplasms characterized by a fibrotic, band-like texture. These tumors are locally aggressive but do not metastasize. Despite their lack of metastatic potential, they can lead to significant morbidity and mortality due to their high recurrence rate and ability to involve adjacent organs. When these tumors arise in bone, they are termed desmoplastic fibromas.[1] This report presents the case of a 26-year-old male who reported pain and tenderness in the right popliteal fossa. Imaging studies and histopathological analysis confirmed the diagnosis of a periosteal desmoid tumor, also known as fibromatosis.
CASE REPORT
A previously asymptomatic 26-year-old man presented to the orthopedic outpatient clinic with a complaint of pain and tenderness localized to the right popliteal fossa, specifically on the lateral aspect. The patient reported no history of trauma, recent physical exertion, or any activity that might have led to the onset of pain. Upon clinical examination, tenderness was noted over the lateral aspect of the right popliteal fossa. The skin over the area appeared normal, with no signs of redness and swelling. Conventional radiograph of the knee showed smooth scalloping above the lateral femoral condyle suggesting an extraosseous/periosteal lesion [Figure 1]. To further investigate the cause of the pain, magnetic resonance imaging (MRI) was performed [Figure 2], which showed an avidly enhancing T2 iso to hypointense, proton density fat suppressed hyperintense lesion in the right popliteal fossa, deep to the lateral head of gastrocnemius, abutting and scalloping the lateral femoral condyle, and having intra-capsular extension. The lesion showed broad base over periosteum. No cartilage defect or cortical erosion was seen. The popliteal neurovascular bundle was away from the lesion. Imaging differentials, in this case, were periosteal desmoid tumor/desmoplastic fibroma, cortical desmoid, periosteal fasciitis, cortical irregularity syndrome, giant cell tumor of tendon sheath, and a rare possibility of periosteal osteosarcoma. Consequently, an ultrasound-guided biopsy was performed to obtain tissue samples from the affected area. The histopathological examination of the biopsy samples [Figure 3] revealed fascicles of bland spindle cells arranged in a collagenous stroma and tumor cells positivity for smooth muscle actin (SMA) and beta-catenin. Both imaging and histopathological findings were consistent with the diagnosis of a desmoid tumor/fibromatosis. The patient refused for surgery and is currently on conservative management and 6 monthly follow-up.
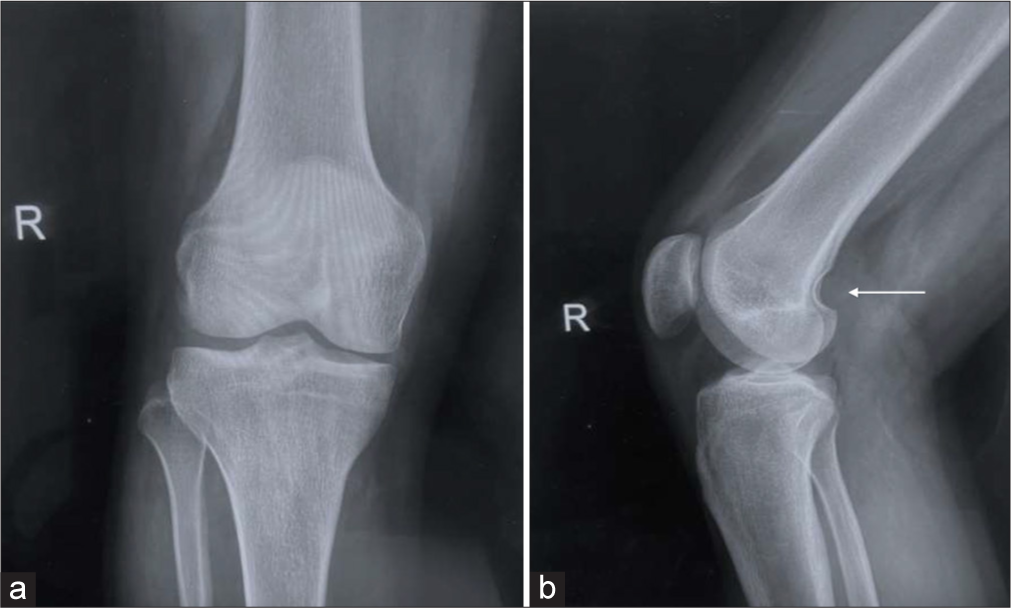
- Conventional radiograph of the knee in (a) anteroposterior view and (b) lateral view showing smooth scalloping above the lateral femoral condyle (arrow).
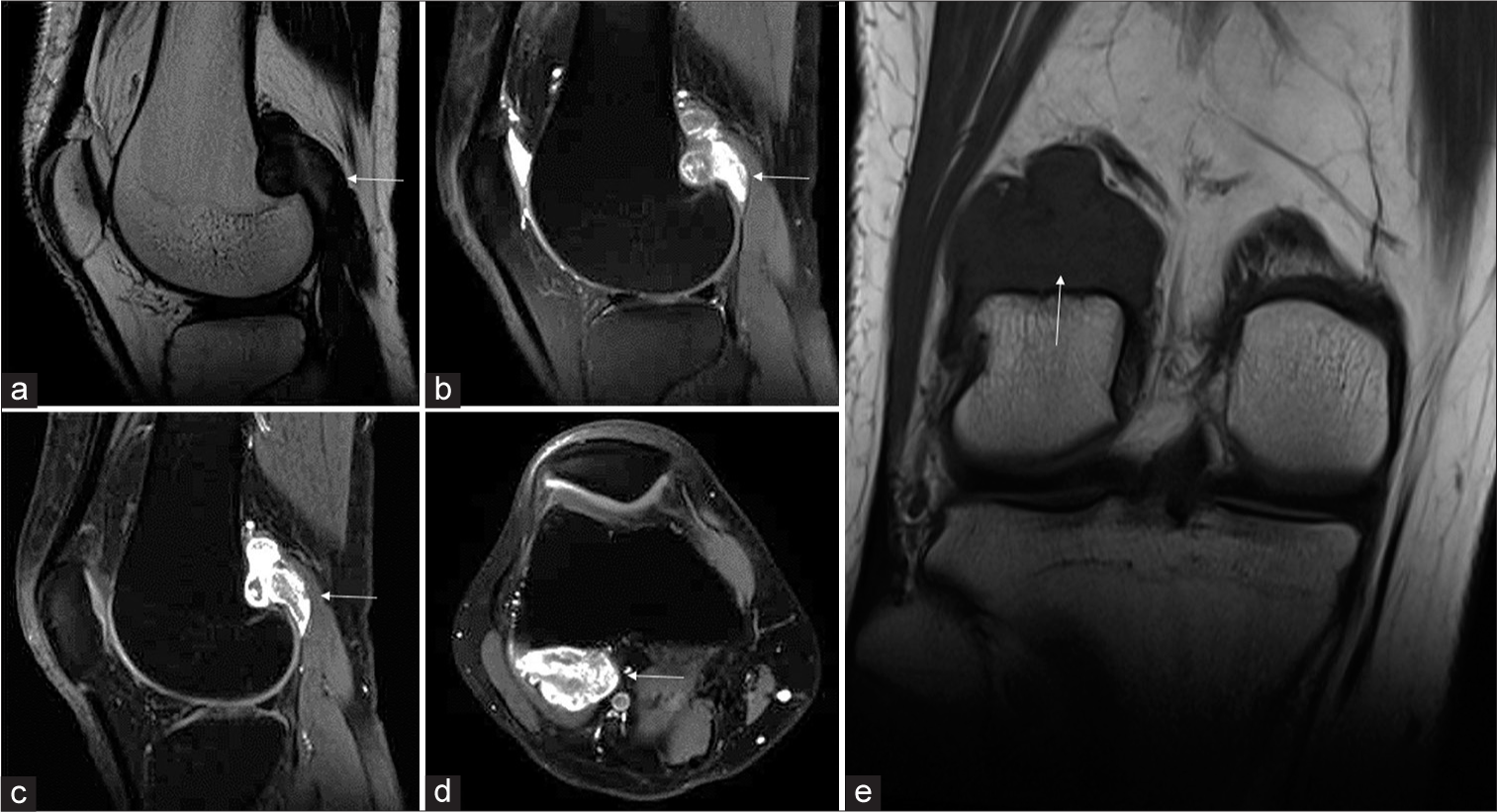
- (a) Sagittal T2-weighted and (b) Proton density fat suppressed (PDFS) images of the right knee show a T2 iso to hypointense, PDFS hyperintense lesion (white arrow in a and b) in the popliteal fossa, deep to the lateral head of the gastrocnemius. (c) Post-contrast T1 fat-saturated sagittal and (d) axial images show avid enhancement of the lesion (white arrow in c and d). Underlying smooth scalloping above the lateral femoral condyle is noted. (e) Coronal T1-weighted sequence shows that the lesion is hypointense (white arrow).
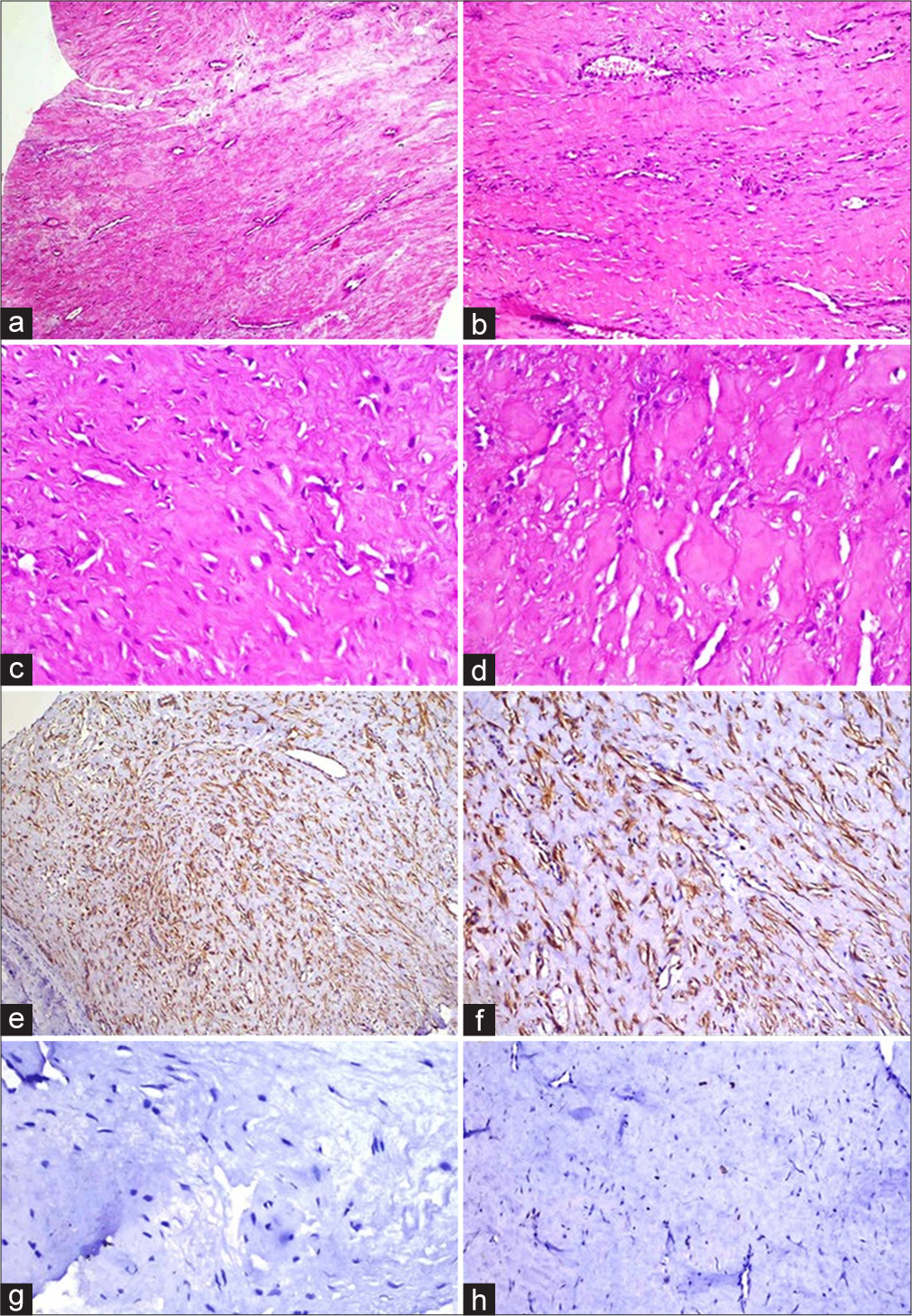
- (a) Hematoxylin and eosin-stained section shows fascicles of bland spindle cells arranged in a collagenous stroma (×100). (b) Hyalinized areas of desmoid tumor with staghorn vasculature (×200). (c and d) Prominent stromal hyalinization along with compressed and thin-walled vessels (×400). (e) Tumor cells immunopositive for smooth muscle actin (SMA; ×100). (f) Tumor cells displaying beta-catenin expression (β catenin; ×200). (g) Tumor cells negative for S-100 (S100; ×400). (h) Tumor cells displaying <1% of ki-67 activity (Ki67; ×200).
DISCUSSION
“Desmoid tumors,” also known as “aggressive fibromatosis,” are uncommon mesenchymal neoplasms with a characteristic fibrotic consistency. These tumors are locally aggressive, leading to significant morbidity and mortality due to their tendency for local recurrence and involvement of adjacent organs, although they do not metastasize. The incidence rate of desmoid tumors is 2–4 cases per million annually, with a slight predominance in females and a peak occurrence in the third and fourth decades of life.[1] These tumors tend to be more aggressive in younger individuals, with recurrence rates reported as high as 87%. Clinically, desmoid tumors often present as firm masses, frequently located outside the abdomen.[2] Histologically, they are composed of uniform spindle cells and fibroblasts within a dense collagenous stroma, characterized by low mitotic activity and rare instances of necrosis. Immunohistochemically, desmoid tumors are positive for β-catenin, vimentin, and SMA but negative for markers such as desmin, S-100, CD34, and MDM2.[3] These tumors are associated with conditions such as “familial adenomatous polyposis” and “Gardner syndrome,” and other risk factors include trauma, surgical procedures, pregnancy, and oral contraceptive use. “Extra-abdominal desmoid tumors” often involve muscle and fascia and commonly occur in regions such as the shoulder, extremities, back, and neck. In addition, desmoids can manifest as intraosseous desmoplastic fibromas, particularly in the mandible, long bones, and pelvis.[4,5]
Imaging plays a critical role in evaluating desmoid tumors, with ultrasound, computed tomography, and MRI being essential modalities. MRI is particularly advantageous due to its superior soft-tissue contrast.[6,7] Characteristic MRI appearance of desmoid tumor is hypointensity on T2-weighted sequence which was present in our case. Key differentials in our case included periosteal desmoid tumor/desmoplastic fibroma, cortical desmoid, periosteal fasciitis, cortical irregularity syndrome, giant cell tumor of the tendon sheath, and the rare possibility of periosteal osteosarcoma. Cortical desmoids typically appear on the posteromedial aspect of the distal femur and lack a prominent soft-tissue component. Giant cell tumor of the tendon sheath shares a similar T2 hypointense appearance on MRI. Periosteal osteosarcoma, though a possible consideration, was less likely here due to the absence of ossification on radiography. To the best of our knowledge, there is no published literature that mentions periosteal desmoid tumor or fibromatosis at this site. The management of desmoid tumors typically involves a multidisciplinary approach. Stable, asymptomatic tumors may be monitored, while symptomatic tumors often require treatment, with surgical resection being a common option despite the high risk of recurrence. There is a growing trend toward conservative management, including the use of radiation therapy and systemic treatments.[8]
CONCLUSION
This case highlights the importance of recognizing the periosteal origin of desmoid tumors for accurate diagnosis and optimal patient care. Radiologists are pivotal in identifying these rare presentations, which can significantly impact diagnostic and management decisions. Although femoral metaphyseal scalloping appears benign on plain radiographs, further evaluation with MRI is essential to avoid overlooking the periosteal lesion. In addition, MRI provides a baseline for ongoing monitoring, whether the lesion is surgically excised or followed through imaging follow-up.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- A to Z of desmoid tumors. AJR Am J Roentgenol. 2011;197:W1008-14.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and imaging features of desmoplastic fibroma of bone for correct diagnosis and differentiation. Curr Med Imaging. 2022;18:1093-8.
- [CrossRef] [PubMed] [Google Scholar]
- Desmoplastic fibroma of the Mandible with unusual histopathological features. Indian J Pathol Microbiol. 2021;64:548-52.
- [CrossRef] [PubMed] [Google Scholar]
- Non-odontogenic tumors of the jaws In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025.
- [Google Scholar]
- Case report 847. Juxtacortical aggressive fibromatosis (desmoplastic fibroma) of the forearm. Skelet Radiol. 1994;23:560-3.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodality imaging assessment of desmoid tumors: The great mime in the era of multidisciplinary teams. J Pers Med. 2022;12:1153.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodality imaging features of desmoid tumors: A head-to-toe spectrum. Insights Imaging. 2020;11:103.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advances in desmoid tumor therapy. Cancers. 2020;12:2135.
- [CrossRef] [PubMed] [Google Scholar]






