Translate this page into:
Acro-osteolysis in Hajdu Cheney syndrome: A case report with review of literature

*Corresponding author: Humsheer Singh Sethi, Department of Radiodiagnosis, Kalinga Institute Of Medical Sciences, Odisha, India. humsheer@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sethi HS, Sen KK, Mohanty SS, Panda S, Agrawal A, Sharawat A. Acro-osteolysis in Hajdu Cheney syndrome: A case report with review of literature. Indian J Musculoskelet Radiol 2021;3(1):39-44.
Abstract
Objectives:
We present a case report and review the literature on Hajdu Cheney syndrome (HCS), an extremely rare connective tissue disorder with <100 cases reported in the last 72 years. We have emphasized on the patterns of acro-osteolysis (acrosteolysis) in the literature review to conclude if the syndrome follows any particular pattern like in our case.
Material and Methods:
All major databases were searched for all cases of HCS. One hundred and eighty-eight hand radiographs were analyzed and detailed analysis of all digits was carried out with emphasis on the pattern of acrosteolysis.
Results:
Acrosteolysis may not be a mandatory association in HCS as 18.8% did not have acrosteolysis at all. The first finger to be involved in 90/96 (93.7%) of the cases was the index finger, followed by the middle finger and then the thumb. The 4th digit (ring finger) was involved in only 11/96 (11.4%) of the cases, of which 9/11 (81.8%) were above the age of 25. Incidence of acrosteolysis of the 4th digit when in comparison to all other finger has a P < 0.05 and a P < 0.001 with the index finger. Newborn with HCS evaluated for acrosteolysis at birth was negative.
Conclusion:
There was statistical evidence to conclude that in a majority of the cases the 4th digit was involved the least. A rough timeline of the onset and progression of acrosteolysis was made. An attempt was made to shed light on the possible lesser-known manifestations of the syndrome such as retroflexed odontoid, Arnold Chiari I, middle phalanx osteolysis, and first carpometacarpal joint osteolysis. As very little is known about the disease and awareness about it is pertinent for early management and to differentiate it from other less-lethal causes of acrosteolysis.
Keywords
Acrosteolysis
Hajdu Cheny syndrome
NOTCH gene
Idiopathic acrosteolysis
INTRODUCTION
Hajdu-Cheney syndrome(HCS) is an infrequently encountered connective tissue disorder with less than a 100 cases reported till date. Typical findings are “band like” acrosteolysis (resorption of the mid-portion of the phalanges) involving the distal phalanges of both hands which is distinct from the typical type of acrosteolysis wherein there is resorption of only the terminal tuft. In our reported case we found that there was sparing the distal phalanx of the fourth(ring) finger. This interesting finding was the main impetus for us to review all the reported hand radiographs in the literature of HCS and to conclude if this peculiar pattern of acrosteolysis can be attributed as a pattern of digital involvement in the syndrome. Other features are absent or hypoplastic frontal sinuses, early loss of teeth, short stature ,characteristic facies and osteoporosis. Deformities involving skull, mandible, spine other bones are also encountered.
CASE PRESENTATION
A 35-year-old female presented to the medicine outpatient for non-specific complaints. She appeared short for age with obvious skeletal abnormalities and was referred for an X-ray. She gave a history of painless and progressive shortening of her fingers and toes. Interestingly she gave a history of menarche at 19 and attained menopause at the age of 26. She was a teacher by profession and showed no signs of mental retardation. Her BMI classified her as underweight. She had a distinctive facial appearance with low set ears, receding chin, beaking of the nose (sharp nose), microsomia (narrow mouth opening), thin and pursed lips with a long philtrum, and straight hair with bushy eyebrows. However, no hypertelorism was noted.
On oral examination she had a high arched palate, both right and left maxillary second molars were partially erupted. The lower third of the face appeared to be short and the maxilla appeared to be hypoplastic. After a thorough investigation, there was no evidence of spinal, renal, or cardiac pathology. No similar familial history was present, patient’s younger sister was not suffering from any similar illness. Antenatal history was not significant, no developmental delays were present at birth. The fingers [Figure 1] and toes of both hands and feet respectively appeared to be short and stubby. Symptoms were not present at birth and manifested approximately 5 years after birth. There were no signs of local inflammation. Existing endocrinological and metabolic workup revealed that there was a low serum calcium (6.0 mg/dl), normal PTH, and an increased serum alkaline phosphatase (110 U/L). At the end of the clinical evaluation, there were two major conditions in the differentials, Hajdu Cheney syndrome and Adult-Onset Progeria. However, the hyaluronic acid estimation in urine was within normal limits (although this is not a confirmatory test) and there was no cardiac abnormality but the history of the premature menopause and the clinical “beaking” was hinting in the direction of Adult-Onset Progeria.

- Clinical photograph of hands showing short fingers and distal pseudo-clubbing.
We hoped a skeletal survey could help us in narrowing down to the diagnosis, it included posteroanterior (PA) projections of hands [Figure 2], wrist and feet [Figure 3] ,skull lateral [Figure 4], Chest PA view, Dorsal lumbar spine-AP & Lateral, Pelvis including both femoral long bones, and subsequently an MRI brain (Figure 5) was also done. The chest radiograph showed no lateral clavicular osteolysis to favor the diagnosis of Adult-onset Progeria. The radiograph of the pelvis was essentially normal save for the osteopenia. The patients clinical, radiological features and history led us to investigate in the direction of Hajdu Cheny Syndrome, which was confirmed by PCR amplification (DNA Labs. in) and sequencing showed a mutation in exon 34 of the NOTCH2 gene: mutation Q2233X C > T which was sufficient for the confirmatory diagnosis of the disease.

- Radiograph of the right hand (a) shows transverse band like acro-osteolysis involving distal phalanx of the second, third, and fifth finger (red arrows). There was near complete osteolysis of distal phalanx of the thumb. Fourth digit was completely spared. Radiograph of left hand(b) shows transverse band like acroosteolysis involving distal phalanx of the thumb, second, third and fifth finger (red arrows). Fourth digit was completely spared. The soft tissues around the tips of terminal phalanges of both hands appear normal. No periarticular or any soft tissue calcification is seen in both hands.

- Frontal radiograph of right foot (3A) shows osteolysis involving distal phalanx of second, third and fourth toe and middle phalanx of fifth toe (red arrows). Frontal radiograph of left (3B) foot shows osteolysis involving the distal phalanges of all distal phalanges (red arrows).

- Lateral radiograph of the skull showed aplasia of frontal sinus (dotted red arrow) and multiple wormian bones (red arrow) in the lambdoid suture with multiple unerupted teeth.

- T1 Sagittal MRI image shows tonsillar herniation (red arrow) with a retroflexed odontoid process (dotted red arrow).
DISCUSSION
Hajdu Cheney syndrome(HCS) also known as type VI idiopathic osteolysis and acorosteolysis dominant type is an extremely rare connective tissue disorder with <100 cases reported in the past 72 years. With the prevalence being less than one in one million (<1/1,000,000)[1] it is thought to occur due to a defective bone and collagen formation mechanism in affected individuals.[2,3] It has an autosomal dominant inheritance[3] but sporadic cases have also been reported.[4]
Common imaging findings [Table 1] documented to be associated with the syndrome were assessed. The presence of acrosteolysis with any three other features, such as Wormian bones, open skull sutures, platybasia, micrognathia, mid-facial flattening, premature loss of teeth, coarse hair, and short stature, was enough for a diagnosis prior to the era of genetic testing.[5]
| Finding | Percen |
|---|---|
| Craniofacial | |
| Wormian bones | 59.3 |
| Hypoplastic frontal sinus Sella abnormalities |
32.2 29.1 |
| Basilar invagination Platybasia |
28.1 15.6 |
| Skeletal | |
| Acro-osteolysis Osteoporosis Scoliosis Dislocation of Radial head |
81.2 53.1 14.5 10.4 |
| Other Abnormalities | |
| Short stature | 57.2 |
| Dental abnormalities | 25 |
| Hearing impairment Polycystic kidneys Patent Ductus Arteriosis High arched palate |
22.9 15.6 12.5 11.4 |
Acro-osteolysis can be radiologically classified into three major groups. In the first group, there occurs resorption only of the terminal tufts. This pattern is seen in diseases like scleroderma, psoriatic arthropathy, neuropathic disease, Raynaud’s disease, sarcoidosis, hyperparathyroidism, porphyria, pachydermoperiostosis, and progeria. These are all differential of HCS and can be differentiated based on the laboratory and imaging findings [Table 2].
| Condition | Clinical and Laboratory parameters | Imaging features |
|---|---|---|
| Hajdu-Cheney | • Short stature | • Type of acro-osteolysis- Band such as (Resorption of |
| syndrome | • Shortened lower third of the face | the mid-portion of the phalanges) |
| • Conductive hearing loss | • Wormian bones | |
| • Dental abnormalities | • Hypoplastic frontal sinus | |
| • Pseudoclubbing” | • Sella abnormalities | |
| • Polycystic kidneys | • Basilar invagination | |
| • Alkaline phosphatase may be increased | • Platybasia | |
| • Generalized osteoporosis | ||
| • Scoliosis | ||
| • Dislocation of Radial head | ||
| Psoriatic arthritis | • Negative for rheumatoid factor | • Type of acro-osteolysis- Resorption of phalangeal tuft |
| • Strong association with nail involvement | and periarticular resorption, both | |
| • Uveitis, Conjunctivitis | • Dactylitis: which can present as a “sausage digit” | |
| • Inflammatory bowel disease | • Arthritis mutilans: osteolysis and articular collapse | |
| can cause “telescoping fingers” | ||
| • Enthesitis and marginal bone erosions; “pencil-in- | ||
| cup” deformities are common | ||
| • Periostitis and Sacroilitis | ||
| Hyperparathyroidism | • Primary, secondary, or tertiary (less common) | • Type of acro-osteolysis- Resorption of phalangeal tuft |
| • Increased PTH levels | and periarticular resorption, both | |
| • Can occur in the context of conditions | • Resorption subperiosteal bone, subchondral, | |
| Scleroderma | such as multiple endocrine neoplasias • Autoimmune connective tissue disorder |
subligamentous, intracortical •Type of acro-osteolysis- Resorption of phalangeal tuft |
| characterized by multisystem fibrosis and | and periarticular resorption, both | |
| soft tissue calcification | • Musculoskeletal- subcutaneous and periarticular | |
| • Elevated ESR | calcification | |
| • Pulmonary- ILD changes | ||
| • Gastrointestinal dilatation of distal esophagus, be | ||
| Progeria | • Rapid aging | associated with CREST syndrome • Type of acro-osteolysis- Resorption of phalangeal tuft |
| • Skin changes | • Erosion of superior aspects of ribs | |
| • Osteolysis of distal clavicle | ||
| • Wormian bones | ||
| • Osteoporosis | ||
| • Periarticular soft tissue calcification | ||
| Neuropathic | • Uncontrolled diabetes, leprosy | • Type of acro-osteolysis- Resorption of phalangeal tuft |
| of long duration | • Severe bone destruction | |
| • Feet involved early on | • Malalignments | |
| • Penciling of phalanges “Licked candy appearance” | ||
| • Bone mineral density is maintained | ||
| • Vascular calcification | ||
| Rothmund- | • Poikiloderma typical rash seen in infants | • Type of acro-osteolysis Band like (Resorption of the |
| Thompson’s | • Sparce facial hair | mid-portion of the phalanges) |
| syndrome | • Absent thumb | • Absent radius |
| • Short stature | • Hypoplastic and early fusion of long bones | |
| • RECQL4 mutation | • May be associated with a higher risk for | |
| • Cataracts | osteosarcomas | |
| Pyknodysostosis | • Autosomal recessive | • Type of acro-osteolysis- Band like (Resorption of the |
| • Short stature | mid-portion of the phalanges) | |
| • Multiple bone fractures | • Osteosclerosis with narrowed medullary cavities is | |
| • Osteosclerosis | the main generalized imaging finding | |
| • Nasal Beaking | • Obtuse mandibular angle | |
| • Wormian bones | ||
| • Delayed closure of sutures | ||
| • Hypoplastic clavicle | ||
| Other rarer causes of | • Polyvinyl chloride (PVC) exposure | |
| Band like acro-osteolysis | • Mechanical such as string instrument players |
In Hajdu Cheney syndrome, Rothmund’s syndrome, and chronic polyvinyl chloride exposure there is resorption of the mid-portion of the phalanges. However, the typical characteristic pattern of the “band like” acrosteolysis involving the distal phalanges of both hands with sparing the distal phalanx of the 4th digit has been of interest in our study which has not been reported earlier. We have no plausible hypothesis for this peculiar pattern of digital involvement; however, it seems unlikely that it is coincidental.
All specific findings with most secondary findings were seen in our patient. Diagnosis is made on clinical grounds, radiological evaluation, and genetic counseling. NOTCH-2 gene mutation is analyzed by isolating genomic DNA from peripheral leukocytes and exon 34 amplified by polymerase chain reaction. Treatment is symptomatic, bisphosphonates prevent resorption of bone and are prescribed.
The NOTCH gene apart from being diagnostic in the syndrome has been of interest as the signaling correlates with a higher likelihood to develop osteoporosis.[6]
which could help reverse this physiological phenomenon. Furthermore, the link between loss of NOTCH gene and osteoarthritis in model studies has recently garnered interest.[7]
REVIEW OF LITERATURE
The databases Medline, Pubmed, Embase, Biological Abstract, Science Citation Index, and Scielo were searched for relevant articles in all languages from January 1948 to November 2020. Using the keywords “Hajdu-Cheney Syndrome”, “Acro-Osteolysis”, NOTCH2 gene, “Acrosteolysis dominant type”, and “Type IV acrosteolysis”.
Repeat publications were excluded. All case reports of HCS were included in the study. Following the retrospective study of the available data, further analysis of the skeletal details in HCS was undertaken. Manual search of the references quoted in these articles was also carried out.
95 cases were studied retrospectively and with the present study, the prevalence to 96 globally. A total of 188 hand radiographs were analyzed to look for any particular pattern, especially for acro-osteolysis.
Study of the digits
Acrosteolysis in some form was noted in 78 of the 96 cases with the left hand being more commonly affected in 54/96 (56.2%). The first finger to be involved in 90/96 (93.7%) of the cases, was the index finger, followed by the middle finger and then the thumb [Figure 6]. The ring finger was involved in only 11/96 (11.4%) of the cases, of which 9/11 (81.8%) were above the age of 25. In familial cases, the first fingers to be involved were index and the little finger simultaneously.
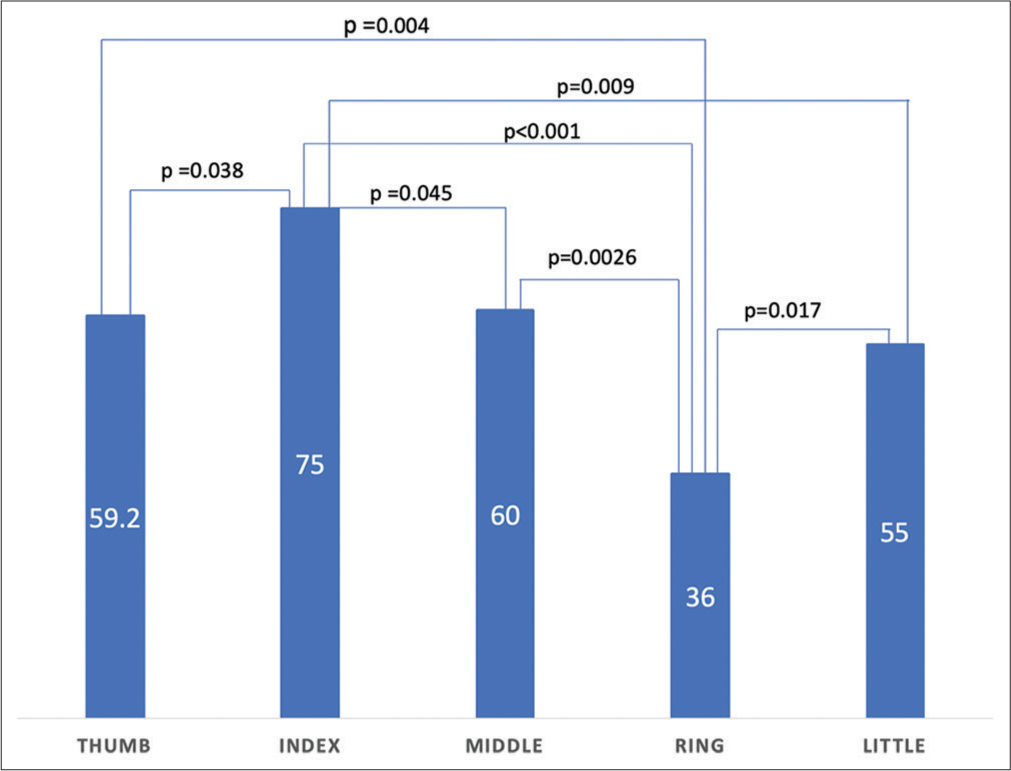
- The 4th digit when in comparison to all other fingers has a p<0.05 which is of statistical significance
The age of diagnosis of acrosteolysis was in between 1 and 4 years whereas in sporadic it was 6–12 years. Newborn with HCS (genetic diagnosis) evaluated for acrosteolysis at birth was negative. Acrosteolysis was seen in 5/8 (62.5%) of the toddlers (1–4 years) evaluated.
Ethical clearance
Institutional Ethical Committee, Ref. No.: KIIT/KIMS/ IEC/379/2020.
CONCLUSION
Following review of literature and analysis of the radiographs in them, it is evident that this rare condition was not systematically documented with no mention of the pattern of digital involvement.
Some of the salient findings in this review of HCS are the predilection for females 56%. Age distribution in both males and females was between 20 and 22 years. Acrosteolysis may not be a mandatory association in HCS as 18.8% did not have acrosteolysis. The incidence of involvement of the 4th digit was the least 11.4%.
Some associated findings with although reported incidence of <10% was retroflexed odontoid, Arnold Chiari I, middle phalanx osteolysis, and first carpometacarpal joint osteolysis they may have been underreported as they are not considered a part of the syndrome. The features basilar invagination and acro-osteolysis tend to become more prominent with advancing age.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Hajdu-Cheney syndrome: A review. Orphanet J Rare Dis. 2014;9:200.
- [CrossRef] [PubMed] [Google Scholar]
- Truncating mutations in the last exon of NOTCH2 cause a rare skeletal disorder with osteoporosis. Nat Genet. 2011;43:306-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mutations in NOTCH2 in families with Hajdu-Cheney syndrome. Hum Mutat. 2011;32:1114-7.
- [CrossRef] [PubMed] [Google Scholar]
- Mutations in NOTCH2 cause Hajdu-Cheney syndrome, a disorder of severe and progressive bone loss. Nat Genet. 2011;43:303-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrodentoosteodysplasia: A genetic “acroosteolysis” syndrome. Birth Defects Orig Artic Ser. 1974;10:145-52.
- [Google Scholar]
- Dimorphic effects of Notch signaling in bone homeostasis. Nat Med. 2008;14:299-305.
- [CrossRef] [PubMed] [Google Scholar]
- Mice harboring a Hajdu Cheney syndrome mutation are sensitized to osteoarthritis. Bone. 2018;114:198-205.
- [CrossRef] [PubMed] [Google Scholar]






