Translate this page into:
Association between the Critical Shoulder Angle and Non-traumatic Rotator Cuff Tears

*Corresponding author: Dr. Sanjay Desai, Consultant Radiologist, Department of Radiology, Deenanath Mangeshkar Hospital, Pune, Maharashtra, India. drsanjaydesai@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jadhav A, Desai S, Reddy V, Kuruvilla R, Mahadeokar P. Association between the Critical Shoulder Angle and Non- traumatic Rotator Cuff Tears. Indian J Musculoskelet Radiol 2019;1(2):88-91.
Abstract
Background:
Moor et al. developed a critical shoulder angle (CSA) as a radiological parameter for the development of rotator cuff injury and degenerative changes of the glenohumeral joint. The objective of this study is to evaluate the association between CSA and the development of non-traumatic rotator cuff tears (RCTs) to further validate this study.
Materials and Methods:
The study was performed as an observational study dividing subjects into control and study groups, differing in the presence of non-traumatic RCT. The study group comprised 50 subjects with 40 subjects in the control group. All acceptable radiographs were evaluated, to measure the CSA in accordance with Moor et al.
Results:
The mean CSA of control subjects was 31.79° (± 1.89°), while that of study subjects were 37.85° (± 2.25°). The relative variability in the control group was about 6% and that in the study group was also 6%, indicating internal homogeneity of the study groups. Chi-square test applied to the distribution gave a P = 0.00001, representing an excellent association between the study groups and the CSA.
Conclusion:
There is a significant association between larger CSA and RCTs (P = 0.00001). Individual (quantitative) anatomical parameters may imply altered biomechanics, which are likely to induce RCTs, independent of trauma and degenerative glenohumeral joint disease.
Keywords
Critical shoulder angle
Rotator cuff
Non-traumatic
Instability
INTRODUCTION
The incidence of rotator cuff tears (RCTs) ranges from 7% to 40%, progressively increasing as age advances. RCTs are essentially traumatic and/or degenerative. The diagnosis of RCTs is primarily clinical, based on a detailed history and physical examination, which allows interpretation of the integrity of different muscles of the rotator cuff. A shoulder radiograph gives us details about the osseous anatomy of the shoulder. Since the rotator cuff is not directly visualized on a radiograph, important indirect signs, mainly regarding the acromial morphology pointing toward a possible rotator cuff lesion can be noted. Examples include the acromial morphology, acromial cysts, sclerosis, and spurs. The acromiohumeral distance (reduced in full- thickness supraspinatus tears) and the lateral acromial projection, the latter being the point of contention in our study. Measuring the lateral acromial projection by the critical shoulder angle (CSA) was proposed by Moor et al.[1] With this analysis, we aim to determine if any association exists between an increased CSA and the development of non-traumatic RCTs. Since trauma is an independent factor in the causation of RCTs, we are excluding traumatic tears in this study to further refine the supposed association.
Rationale
A radiograph of the shoulder is the most common radiological investigation conducted in orthopedic outpatient departments. Despite giving the aforementioned indirect signs, a radiograph cannot characterize a RCT, which requires ultrasonography (USG) and/or magnetic resonance imaging (MRI). We aim to provide CSA determined on an anteroposterior (AP) shoulder radiograph, as an additional predictor, in the supplement to the clinical examination, for diagnosing RCTs, which can be further characterized in detail by MRI and USG.
MATERIALS AND METHODS
This was a retrospective observational study, with subjects presenting with pain and/or restricted motion of their shoulder/s (symptomatic shoulders) presenting to the orthopedic department. We divided the subjects into case and control groups on the basis of presence and absence of “non-traumatic RCTs,” respectively, as per their USG (in three patients) and/or MRI shoulder scans. There were 50 study subjects and 40 control subjects. All subjects were invited to participate in the study and received information about the objectives and methods.
Inclusion criteria for the case and control groups were symptomatic shoulders with no history of trauma and radiologically confirmed RCTs.
Patients with asymptomatic shoulder, history of trauma, glenohumeral osteoarthritis, and infections were excluded from the study.
After the informed consent was obtained, the epidemiological analysis sheet was completed for each subject. Following this, true AP shoulder radiographs of the subjects were evaluated. Accepted radiographs were those with <20° of internal or external rotation (those radiographs where upper and lower glenoid margins were clearly discernible), in accordance with the study of Moor et al.[1] The radiographs were evaluated by drawing a line connecting the upper (point X) and lower (point Y) glenoid margins. Another line was drawn from point Y to the lateral-most acromial projection (point Z). Angle XYZ was the CSA [Figure 1].

- Critical shoulder angle.
Observations
The mean age of the control group was 55.67 years, while that of the study group was 59.26 years. The study group had a predominance of males (58%). About 62% of subjects in the study group had right-sided symptomatic shoulders. Table 1 depicts the age, sex, and side distribution of the study and control groups.
| Parameter | Control group (n=40) | Study group (n=50) |
|---|---|---|
| Mean age | 55.67 years (45–79) | 59.26 years (45–74) |
| Sex Females Males |
20 (50) 20 (50) |
21 (42) 29 (58) |
| Side Right Left |
21 (52.5) 19 (47.5) |
31 (62) 19 (38) |
The mean CSA of control subjects was 31.79° (±1.89°), while that of study subjects were 37.85° (±2.25°). Table 2 shows the minimum and maximum CSA values in the study and control groups as well as their mean, median and mode, with standard deviation. Mean CSA values of study and control groups are represented in [Figure 2].
| Subjects | Min. CSA |
Mean | Median | Mode | Max. CSA |
SD |
|---|---|---|---|---|---|---|
| Control | 28.8 | 31.79 | 31.55 | 31.5 | 39.4 | 3.61 |
| Study | 33.8 | 37.85 | 37.95 | 38.5 | 49 | 5.06 |
SD: Standard deviation, CSA: Critical shoulder angle
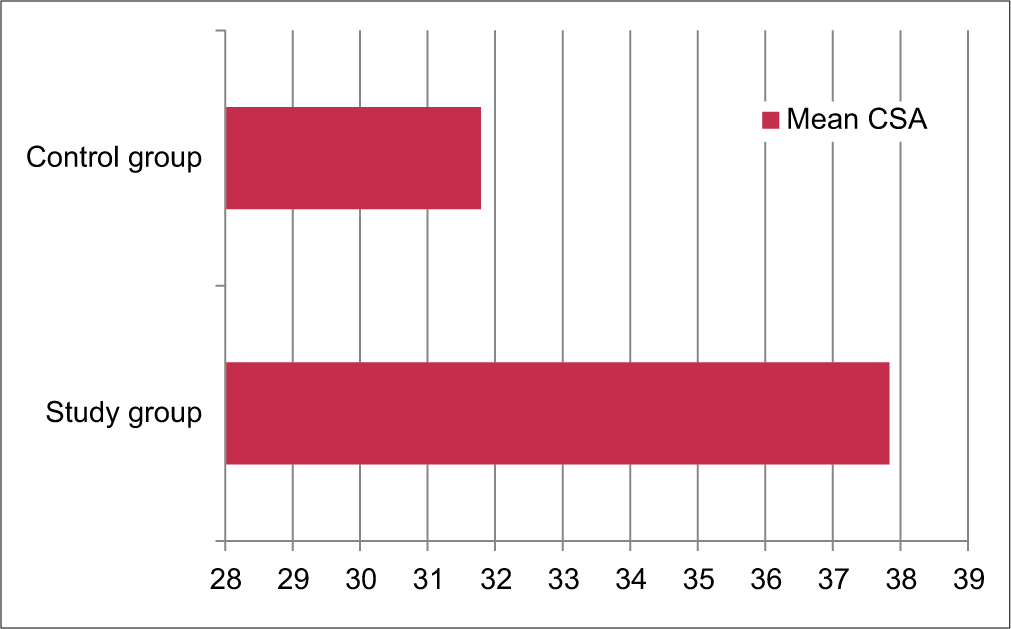
- Mean critical shoulder angle of study and control groups, depicted by a bar diagram.
We divided the subjects into two groups, as we noted there was a predominance of CSA values more than 34° in the study subjects, while CSA values of ≤34° were predominant in the control subjects. Subjects with CSA ≤34° were put into Group 1, while those with CSA values more than 34° were put in Group 2, as shown in Table 3, and represented in [Figure 3]. Hence, the CSA chosen was 34°.
| Crossed table | Group 1 (with CSA≤34°) |
Group 2 (with CSA>34°) |
Total |
|---|---|---|---|
| Control group | 36 | 4 | 40 |
| Study group | 2 | 48 | 50 |
| Total | 38 | 52 | 90 |
CSA: Critical shoulder angle
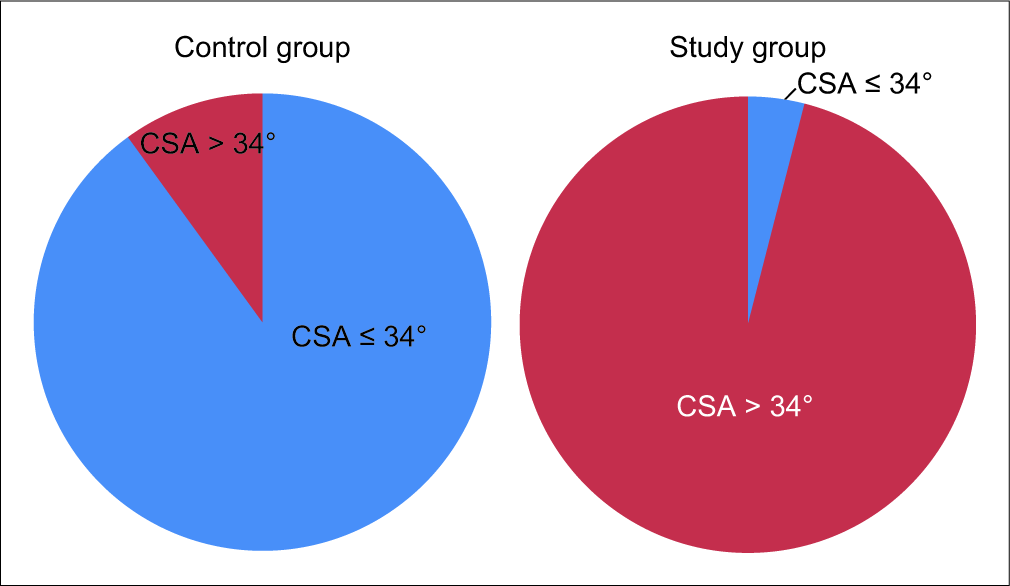
- Group-wise distribution of control and study subjects on either side of 34°, depicted by pie diagrams.
We also observed that most of the RCTs were those involving the supraspinatus tendon alone (62%), followed by the combined affliction of supraspinatus and subscapularis tendons (18%). Infraspinatus was more commonly affected along with the supraspinatus tendon (14%), rather than being involved alone (2% – in just one study subject). The distribution of different RCTs is depicted in [Figure 4].
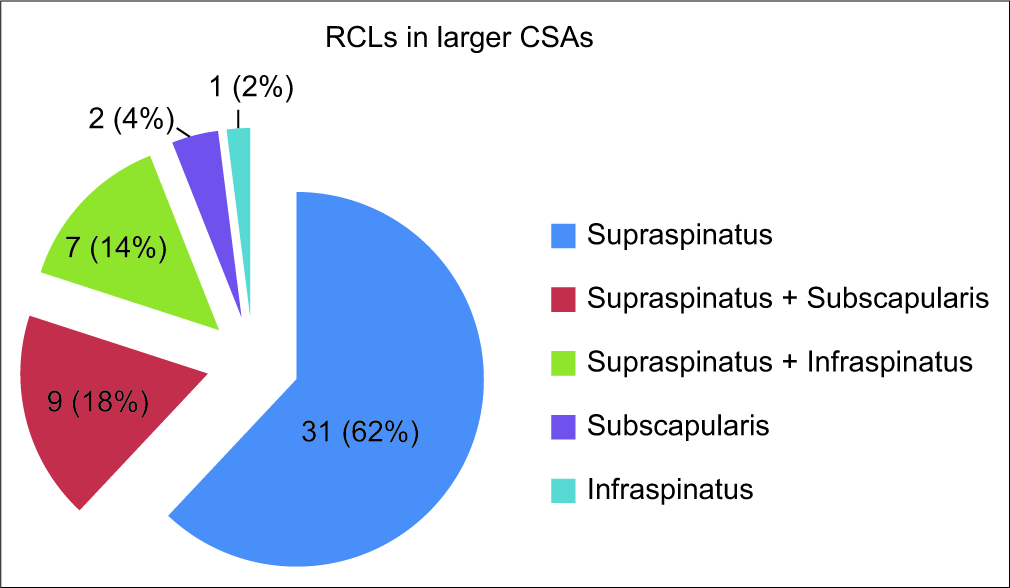
- Distribution of rotator cuff lesions depicted by the pie diagram.
The data tended to symmetry as the median and mean values for both study and control groups were relatively close. The relative variability in the control group was about 6% and that in the study group was also 6%, indicating internal homogeneity of the study groups.
Chi-square test applied to the distribution in Figure 2 gave P = 0.00001, representing an association between the study groups and the CSA.
DISCUSSION
CSA as a parameter was first introduced by Moor et al.[1]
Nyffeler et al.[2] introduced the acromion index, suggesting an association between a greater lateral projection of the acromion and a possible rotator cuff injury. Armstrong[3] would be the first to indicate impingement on supraspinatus tendon due to acromial morphology. Bigliani et al.[4] identified different acromial morphologies. Banas et al.[5] also reported an association between the increased lateral acromial inclination and subacromial pathology.
Gerber et al.,[6] in 2013, proposed that CSA quantifies the lateral acromial coverage independently of features seen in glenohumeral osteoarthritis, such as humeral head flattening or bony erosions of glenoid. He also performed a biomechanical analysis constructing a simulator and hypothesized that increased CSAs lead to an increase in joint shear to joint compression forces (instability ratio), which requires supraspinatus overloading, especially during initial stages of abduction.
Our study observations represent an association between increased CSAs and non-traumatic RCTs. These findings are in sync with those of Moor et al.,[1] Gerber et al.,[6] and Spiegl et al.[7]
Normal healthy shoulder is defined by a balanced mechanical overload. CSA essentially defined the acromial anatomic configuration, in that apart from reflecting the acromial coverage, it also indicates the glenoid inclination, combining these factors into a biomechanical parameter.[6] Hence, CSA points toward potentially altered biomechanics.
The drawback of our study included being limited by the accuracy of USG and/or MRI in diagnosing the RCTs, as all the study subjects did not undergo surgery and hence arthroscopic confirmation of the tears.
CONCLUSION
There is a significant direct association between larger CSA and non-traumatic RCTs.
Declaration of patient consent
Patient's consent not required as patients identity is not disclosed or compromised.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Joint J. 2013;95-B:935-41.
- [CrossRef] [PubMed] [Google Scholar]
- Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am. 2006;88:800-5.
- [CrossRef] [PubMed] [Google Scholar]
- Excision of the acromion in treatment of the supraspinatus syndrome; report of 95 excisions. J Bone Joint Surg Br. 1949;31B:436-42.
- [CrossRef] [Google Scholar]
- The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:216.
- [Google Scholar]
- Relationship between the lateral acromion angle and rotator cuff disease. J Shoulder Elbow Surg. 1995;4:454-61.
- [CrossRef] [Google Scholar]
- Supraspinatus tendon load during abduction is dependent on the size of the critical shoulder angle: A biomechanical analysis. J Orthop Res. 2014;32:952-7.
- [CrossRef] [PubMed] [Google Scholar]
- The critical shoulder angle is associated with rotator cuff tears and shoulder osteoarthritis and is better assessed with radiographs over MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24:2244-51.
- [CrossRef] [PubMed] [Google Scholar]






