Translate this page into:
Extensive tumoral calcinosis of cervical spine in systemic sclerosis – A rare entity

*Corresponding author: Aruna R. Patil, Department of Radiology, Apollo Hospitals, Bengaluru, Karnataka, India. dr.arunarpatil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chithra A, Patil AR, Karjigi U, Kumbhar KR. Extensive tumoral calcinosis of cervical spine in systemic sclerosis – A rare entity. Indian J Musculoskelet Radiol. 2024;6:128-31. doi: 10.25259/IJMSR_27_2024
Abstract
Tumoral calcinosis (TC) is a distinct pathology with etiologies ranging from primary hereditary forms to secondary underlying conditions, most common being chronic renal failure. Systemic sclerosis (SSc) is often affected by calcinosis, however limited to the subcutaneous tissue. Paraspinal soft tissue is a rare location for tumor like calcific masses in SSc. This case report describes the imaging features of TC in a female patient with SSc.
Keywords
Tumoral calcinosis
Systemic sclerosis
Paraspinal soft-tissue masses
INTRODUCTION
Tumoral calcinosis (TC) refers to tumor-like periarticular calcific masses that occur predominantly in the region of hip, shoulder, and elbow.[1] An autosomal dominant inheritance has been described where it affects an otherwise healthy individual or those with hyperphosphatemia, typically in their first or second decade of life with no sex predilection.[2] Secondary etiologies of TC include patients on hemodialysis, sarcoidosis, collagen vascular disease (particularly scleroderma or dermatomyositis), pseudoxanthoma elasticum, and massive osteolysis.[1] Calcinosis in systemic sclerosis (SSc) is usually limited to subcutaneous regions and not in tumoral form.[3] We present a case of a 60-year-old female with a known history of SSc developing TC in a rare location – cervical spine and paraspinal region.
CASE REPORT
A 60-year-old female patient, a diagnosed case of SSc on treatment for 2 years and follow-up, presented to the rheumatology outpatient department with generalized weakness, fingertip skin thickening, and on and off dry cough with breathlessness. The patient also complained of neck swelling and pain radiating to the right upper limb and back of head. At the time of presentation, the patient was on T. nifedipine, T. hydroxychloroquine, and disease-modifying anti-rheumatic drugs.
Clinical examination revealed reduced entry in bilateral lungs with basal crepitations. A hard painful mass was palpated along the right lateral aspect of neck with no restriction of active range of movements or focal neurological deficits. Plasma levels of phosphorus (3.8 mg/dL) and calcium (9.2 mg/dL) were normal. Serum anti-nuclear antibodies were positive, with positivity for antibody to Scl70 (2+ on Immunofluorescence). The patient had elevated N-terminal pro-B-type natriuretic peptide (1177 pg/mL) with echocardiography showing reduced right ventricular function and severe pulmonary arterial hypertension.
Radiographs of the chest and cervical spine were obtained followed by computed tomography (CT) of chest, cervical spine, and magnetic resonance imaging (MRI) of cervical spine for further workup.
Chest radiograph showed evidence of cardiomegaly with ill-defined radiodensities and reticular opacities in bilateral lung fields [Figure 1a]. High-resolution computed tomography of chest revealed bilateral ground glass opacities, with interstitial thickening and fibrosis predominantly in the periphery [Figure 1b]. Thickening of bronchovascular bundles, with tractional bronchiectasis and sub-pleural cysts were noted [Figure 1c]. Main pulmonary artery was dilated (30 mm) along with dilated esophagus [Figure 1d]. There was no evidence of honey combing/pleural effusion on imaging. The changes were suggestive of non-specific interstitial pneumonia type of interstitial lung disease.
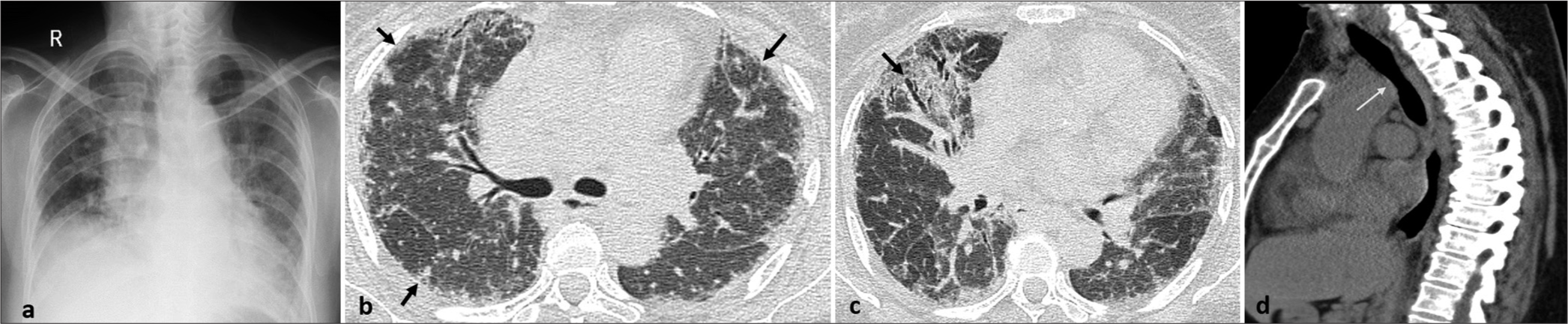
- (a) Chest radiograph frontal view shows cardiomegaly with ill-defined densities and reticular opacities in bilateral lung fields. (b and c) high-resolution computed tomography chest axial image shows subpleural interstitial thickening and fibrosis with tractional bronchiectasis (arrows). (d) Computed tomography chest sagittal image in soft-tissue window shows dilated esophagus (arrow).
The anteroposterior and lateral radiographs of the cervical spine showed a large paravertebral radiopaque lesion in close relation with the posterior elements of spine with sclerosis of C4-6 vertebral bodies and facets [Figure 2a and b]. A subsequently performed CT and MRI cervical spine revealed a large extra-articular calcified lobulated right paravertebral soft-tissue lesion adjacent to the facet joints extending from C1 to C3 vertebrae measuring 2.7 × 3 × 4.5 cm (transverse × anteroposterior × craniocaudal) [Figure 3a and b]. The lesion was predominantly hypointense on both T1-w and T2-w images [Figure 3c and d]. No evidence of fat or fluid signal was noted within the lesion. There was no significant adjacent bony destruction. There were also extensive bilateral fluffy soft-tissue calcifications (hyperdense on CT and hypointense on T1-w and T2-w sequences) predominantly around facet joints and lamina from C2/C3 level to C5/C6 level [Figure 4a and b]. There was sclerosis of the adjacent facet joints with irregularity of the articular margins [Figure 4c and d]. The calcification was also noted to extend into the spinal canal with severe neural foraminal narrowing on the right at C3/C4 and C4/C5 levels. The cord signal intensity was normal.
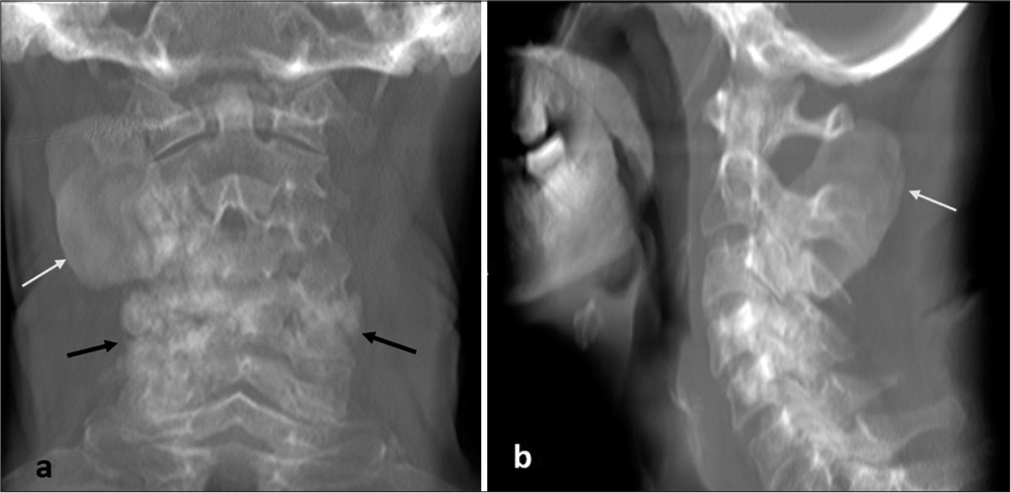
- (a and b) Radiographs of cervical spine, anteroposterior and lateral views. It shows a well-defined paravertebral radiopaque lesion (white arrows) in close relation with the posterior elements of spine and facetal sclerosis (black arrow).
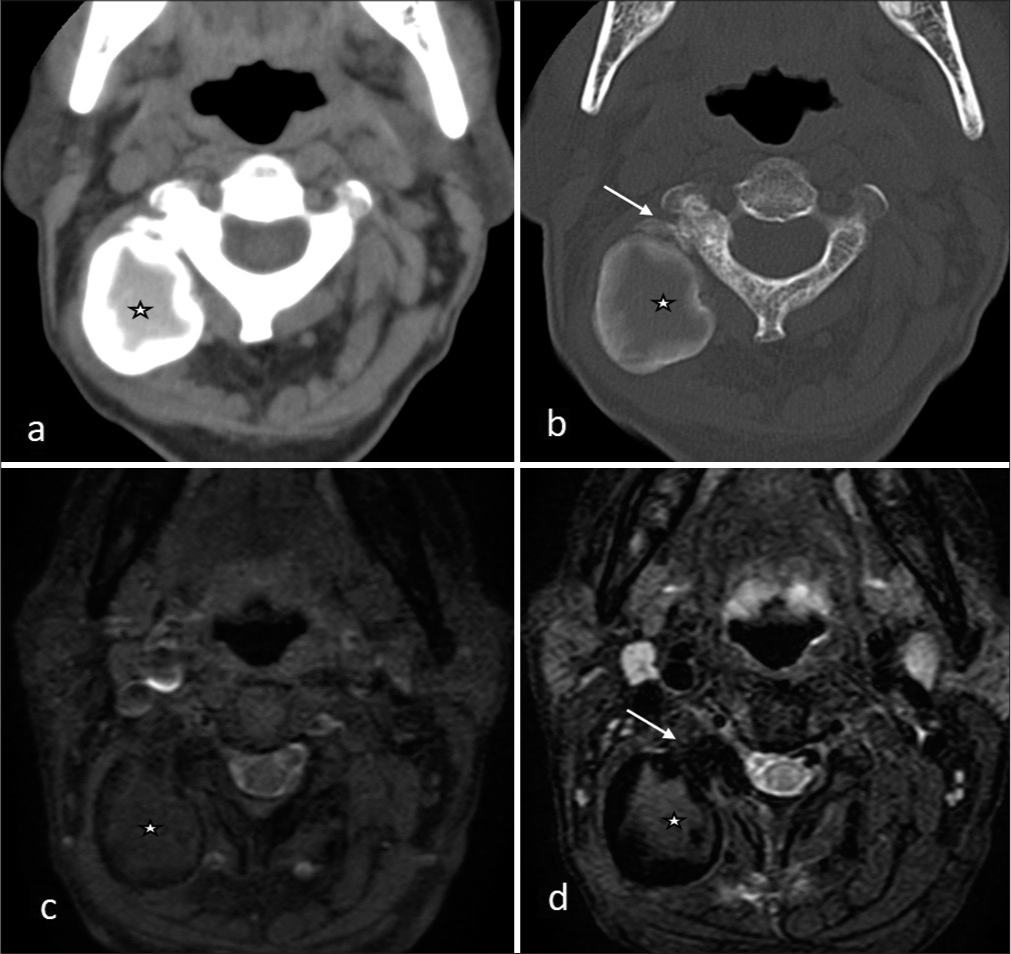
- (a and b) Computed tomography cervical spine axial images, soft tissue and bone window. (c and d) Magnetic resonance imaging cervical spine axial images, T1-weighted fat-saturated. T2-weighted fat-saturated. Show large extra-articular heterogeneously calcified right paravertebral soft-tissue lesion (*) adjacent to the facet joint which shows sclerosis (arrows).
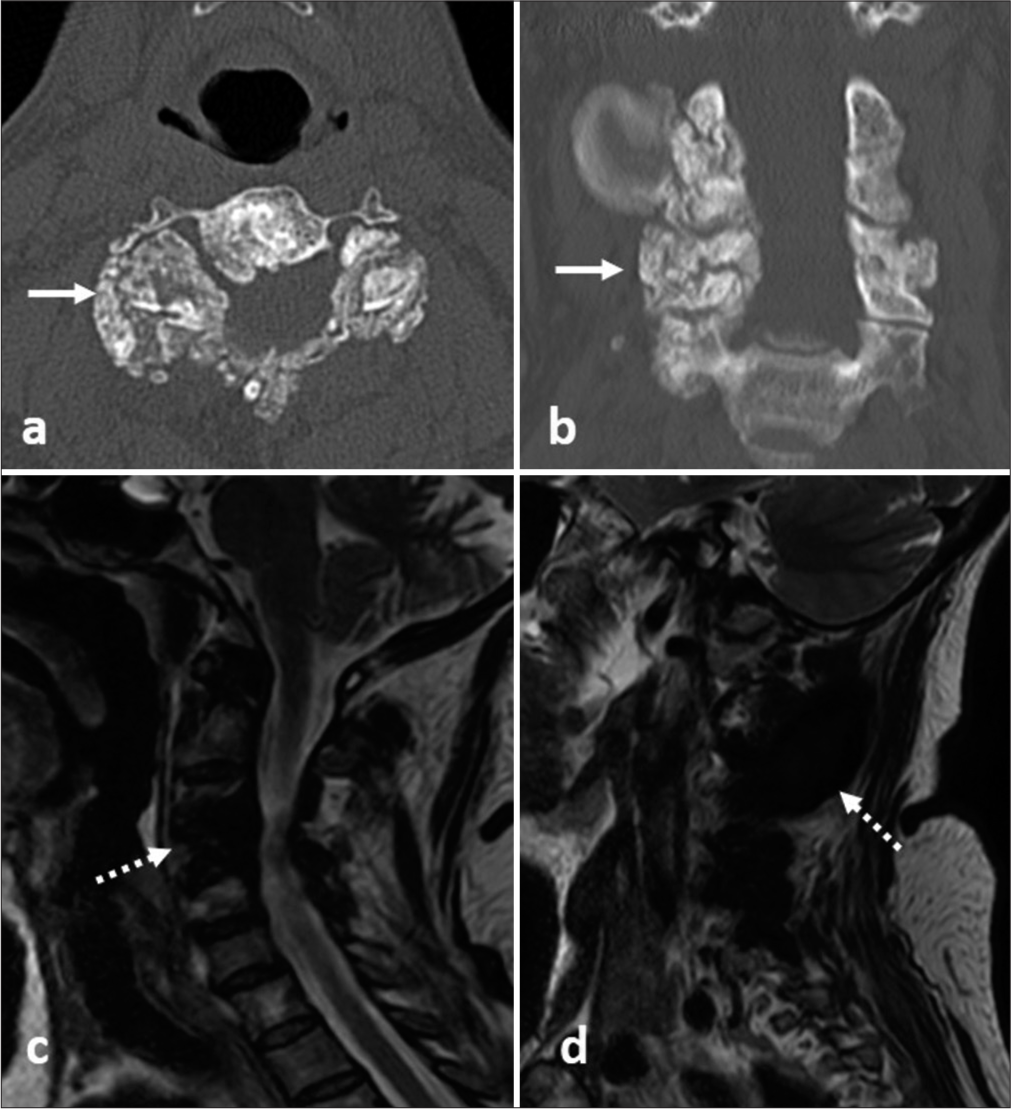
- (a and b) Computed tomography cervical spine axial and coronal images. (c and d) Magnetic resonance imaging (MRI) cervical spine T2 turbo-spin-echo sagittal images. Parasagittal section. Show extensive bilateral fluffy soft-tissue calcifications (arrows) predominantly around facet joints and lamina from C2/C3 level to C5/C6 level. Hypointense areas in corresponding MR images (dotted arrow).
In view of previous history, the clinical and imaging findings were attributed to soft-tissue TC secondary to SSc involving the cervical spine and paraspinal location. Surgical excision of the paravertebral soft-tissue mass was suggested but deferred in view of patient’s impaired cardiac parameters. The patient was managed symptomatically with analgesics and non-calcium-based phosphate binders which allowed an improvement of her clinical symptoms. The patient remains on regular follow-up.
DISCUSSION
TC is characterized by the presence of periarticular lobulated soft-tissue masses which are usually non-tender and contains insoluble chalky calcific material. When large, these can be tender on palpation and may ulcerate the overlying skin exuding chalky, milky fluid.[2] The lesions are usually along the extensor surfaces, commonly affecting the elbows, hips, shoulders, knees, and small joints of the feet.[4]
Smack et al.[5] classified TC into three types: (1) Primary normo-calcemic normo-phosphatemic TC, affecting majority of the patients in their 2nd decade of life. (2) Primary normo-calcemic hyper-phosphatemic TC, affecting patients in their 1st and 2nd decades of life. (3) Secondary TC due to underlying predisposing conditions, including SSc. Chronic renal failure (CRF) is the most common etiology of secondary TC, with hyperphosphatemia and secondary hyperparathyroidism developing in CRF being responsible for TC.[5] SSc is a chronic connective tissue disorder characterized by progressive vasculopathy, autoimmune inflammation, and, eventually tissue and organ fibrosis.[1] Although calcinosis has been well recognized in SSc, with an estimated prevalence of 18–49%, the calcific areas are often small and in the subcutaneous tissue.[6] The occurrence of large calcified masses in SSc is rarely reported (about 3% of patients), with peri-articular soft-tissue calcinosis around the spine being a rare event in SSc.[6,7] Among the spinal forms, cervical region is the most frequently involved, and pain being the most common symptom.[5,8,9] Advanced cases can present with symptoms related to nerve root or cord compression. Calcinosis in SSc occurs without any overt abnormalities of calcium or phosphate metabolism and is thought to be due to dystrophic calcification secondary to mechanical stress, insufficient blood flow, tissue hypoxia, and chronic inflammation.[5]
Radiographs will demonstrate a radiodense lobulated well-defined soft-tissue mass.[7,10] CT may depict radiolucent septations within the lesion giving a cobblestone or chicken wire appearance. Occasionally, the presence of fluid-fluid levels indicates the milk of calcium consistency know as sedimentation sign.[2] On radiographs or CT scan, the calcium level appears hyperdense at the bottom of the lesion; on MRI, sedimented calcium appears hypointense and fluid level above it appears hyperintense on T2. CT or MRI is also useful for pre-operative planning and to assess associated bone or joint changes.[7,9,10] Often absence of erosion of adjacent bones and joints, along normal serum phosphate levels support the diagnosis of secondary TC in appropriate settings.[4]
The other diagnoses to be considered in a secondary soft-tissue calcified masses include: (1) Benign heterotopic ossification[10] which can present following trauma, cerebrospinal disorder, or burn (myositis ossificans) or rarely, in hereditary forms (fibrodysplasia ossificans progressiva). Spine is rarely involved with hip, shoulder, and knee being the common sites, often within the muscles. Ossification following trauma can develop as early as 3 weeks after injury in the form of floccular calcifications, which progresses to develop well-defined peripheral cortex and inner trabeculations in 6–8 weeks time. Serum calcium and phosphate levels are often normal. (2) Calcified hematoma: Often presents with rim such as calcifications, localized, and less mineralized than TC. The adjacent bones and joints are often spared. Careful examination of the CT images may depict underlying fractures. A past history of trauma adds to the diagnosis. (3) Polymyositis or dermatomyositis: Shows sheet such as calcifications of the skin, subcutaneous tissue and fascial planes (commonly referred to as calcinosis universalis), and rarely form a well-defined mass. (4) Calcium pyrophosphate dihydrate crystal deposition disease: Typically presents as articular calcifications of knee, followed by the wrist, pubic symphysis, and the hip. On imaging, there are calcifications in the hyaline and fibrocartilages and also in the tendons where it appears linear and stratified. In the spine, it represents calcifications of the TR ligaments and intradiscal calcifications, rather than presenting as calcified mass. (5) Metastatic calcifications: Underlying metabolic abnormalities in the form of elevated serum calcium and phosphate levels are seen. Often seen in patients with CRF undergoing hemodialysis. Presents as finely speckled calcium deposition throughout the soft tissue.
Treatment of secondary TC relies on treating the underlying condition and medical management with phosphate binders, intravenous Pamidronate, etc. Phosphate binding chelating agents (oral aluminium hydroxide) has shown its effect in both normo- and hyper-phosphatemic cases.[4,5] Surgical excision of the lesion or decompression of the spine may be performed in larger lesions and in those patients having cord compression with neurological deficit. However, surgical excision is often under performed in secondary TC due to other medical comorbidities of the patients and high recurrence rate.[2,4,5]
CONCLUSION
Although rare, TC can occur during the course of SSc. Cervical spine and paraspinal region is an unusual site of involvement. Classical imaging findings, along with clinical and laboratory correlation, help in the diagnosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Extensive tumoral calcinosis in a patient with systemic sclerosis. Am J Orthop (Belle Mead NJ). 2010;39:E108-10.
- [Google Scholar]
- A rare case report of tumoral calcinosis syndrome in an adult with rheumatoid arthritis. Clin Cases Miner Bone Metab. 2015;12:62-4.
- [CrossRef] [PubMed] [Google Scholar]
- Review of tumoral calcinosis: A rare clinico-pathological entity. World J Clin Cases. 2014;2:409-14.
- [CrossRef] [PubMed] [Google Scholar]
- Proposal for a pathogenesis-based classification of tumoral calcinosis. Int J Dermatol. 1996;35:265-71.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudotumoral calcinosis in systemic sclerosis: Data from systematic literature review and case series from two referral centres. Semin Arthritis Rheum. 2020;50:1339-47.
- [CrossRef] [PubMed] [Google Scholar]
- Tumoral calcinosis of the spine in the course of systemic sclerosis: Report of a new case and review of the literature. Clin Exp Rheumatol. 2015;33:S175-8.
- [Google Scholar]
- Tumoral calcinosis involving the cervical spine. Surg Neurol Int. 2015;6:109.
- [CrossRef] [PubMed] [Google Scholar]
- Tumoral calcinosis in the cervical spine: A case report and review of the literature. J Med Case Rep. 2017;11:304.
- [CrossRef] [PubMed] [Google Scholar]






