Translate this page into:
From impact to imaging: X-ray and computed tomography in assessing pelvic trauma and role of magnetic resonance imaging

*Corresponding author: Ami Jani, Department of Radiology, Sheffield Teaching Hospitals National Health Service Trust, Northern General Hospital, Sheffield, United Kingdom. janiami16@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jani A, Spalkit S, Chari R. From impact to imaging: X-ray and computed tomography in assessing pelvic trauma and role of magnetic resonance imaging. Indian J Musculoskelet Radiol. 2025;7:41-53. doi: 10.25259/IJMSR_70_2024
Abstract
Trauma is a leading cause of mortality and morbidity among young adults. Pelvic fractures seen in road traffic accidents are often associated with other bony and soft tissue injuries of the pelvis. Various classifications of pelvic injuries decide the management. Isolated fractures of the acetabulum, femur, and sacrum can occur and their management depends on the severity of injuries. The pelvis hosts important soft tissue organs such as the urinary bladder, urethra, vessels, bowel, and reproductive organs which are at risk of injury along with pelvic trauma. The knowledge of common soft tissue injury patterns and their management is crucial for the referral of the patient to a higher center. Low-energy trauma like falls or minor accidents can cause isolated bony fractures.
Keywords
Acetabular fractures
Bladder injuries
Pelvic fractures
Sacral fractures
Vascular injuries
INTRODUCTION
In this article, we will discuss the epidemiology of pelvic trauma, the brief anatomy of the pelvic ring, the imaging approach, the mechanism and classification of pelvic fractures, isolated acetabular fractures, sacral and femur fractures. As the pelvis hosts several organs, associated soft tissue injuries with pelvic fractures are described briefly. A radiologist should be able to pick up soft tissue injuries even on an unenhanced scan.
EPIDEMIOLOGY
Pelvic fractures account for 2–8% of skeletal injuries.[1] Motor vehicle accidents commonly seen in young adults can result in high-energy impact trauma and present with multiple bone injuries as well as soft tissue injuries. Avulsion fractures of the pelvis and hip are common in the pediatric age group. In the elderly, femur fracture after a fall is common. Muscular injuries of the pelvis and hip joints are common in contact sports. Pelvic trauma, especially high-energy motor vehicular accidents, should be managed in specialized centers that have the support of urologists, vascular interventionists, and surgeons.[2]
ANATOMY OF THE PELVIC RING
The pelvic ring comprises of sacrum and two innominate bones formed by the fusion of ilium, ischium, and pubis. In adults, the bones are fused but in young children, the triradiate cartilage is visible. The two pelvic bones articulate anteriorly with each other at pubic symphysis. Posteriorly, both pelvic bones articulate with the sacrum through sacroiliac joints (SIJs). The pelvic ligaments provide stability to the osseous joints. Anteriorly, pubic ligaments bind the pubic symphysis. The SIJs are supported by sacroiliac and posterior pelvic ligaments. The anterior sacroiliac ligament provides stability against the external rotation. The interosseous and posterior sacroiliac ligaments provide stability against the internal rotation. The iliolumbar ligament reinforces the posterior ligaments. The posterior pelvic ligaments include sacrospinous and sacrotuberous ligaments which provide stability against the vertical shearing (VS) forces.[3] Isolated injuries of these ligaments without bony fractures can result in SIJ diastasis and can be mechanically unstable. Figure 1 shows 3D reconstruction of the pelvis with diagrammatic representation of various pelvic ligaments stabilizing the pelvis.
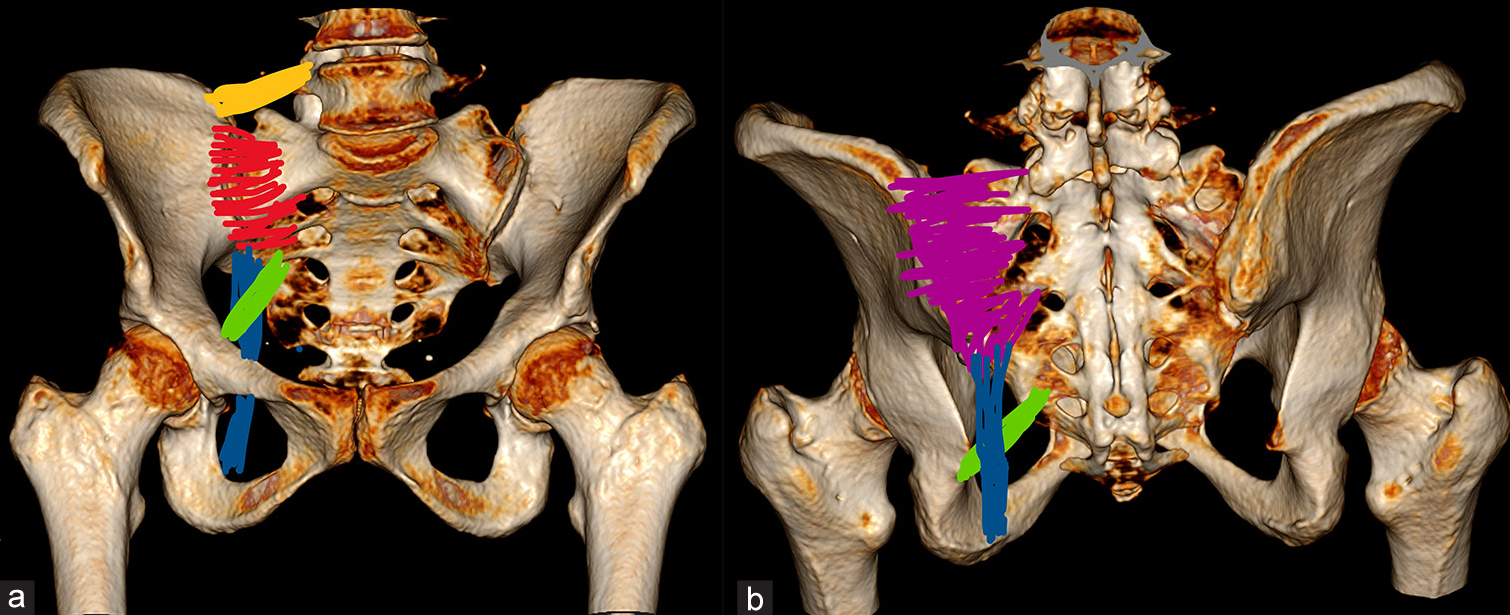
- (a and b) Represent 3D image of pelvic bones with anterior sacroiliac ligaments (red), posterior sacroiliac ligaments (pink), iliolumbar ligaments (yellow), sacrotuberous ligament (blue), and sacrospinous ligaments (green).
APPROACH TO IMAGING IN PELVIC TRAUMA
The imaging choice must be tailored according to the presentation of the patient. As shown in the flowchart [Figure 2], if the patient presents with polytrauma or motor vehicular accidents, computed tomography (CT) whole body (head neck thorax abdomen-pelvis) is the imaging of choice in adults more than 16 years.[2] For pediatric population (<16 years), CT abdomen pelvis is the first choice for investigation when multi-organ injury is suspected. In the rest of the cases, an X-ray is the first choice of imaging. For adults presenting with minor injuries or localized trauma of the pelvis and hips, a pelvic anteroposterior (AP) radiograph is the first choice of imaging. CT can be done for surgical planning of acetabular fractures. In patients with implants, CT can be performed in addition to an X-ray to rule out periprosthetic fracture.[4] In elderly patients when X-ray is frequently false negative, magnetic resonance imaging (MRI) is the investigation of choice. In suspected muscle injuries in athletes, MRI is the preferred modality. Ultrasonography although a less frequently performed investigation for pelvic trauma can be effective when MRI is not easily available.
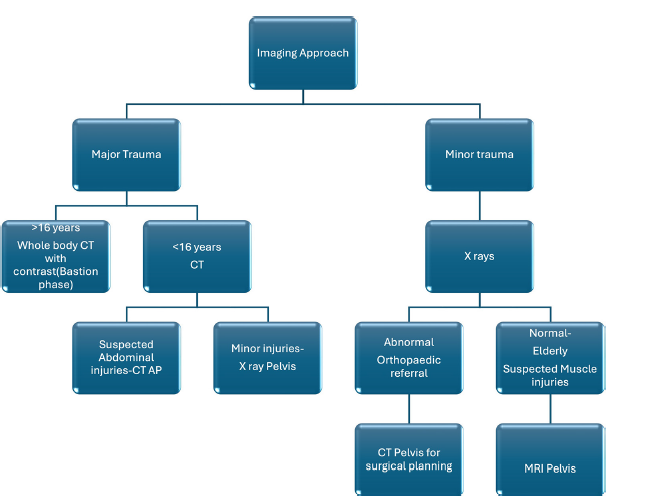
- Depicts the flow chart for the imaging approach to a patient with pelvic trauma which is based on the type of injury and age of the patient. CT AP: Computed tomography abdomen-pelvis
MECHANISM AND CLASSIFICATION OF PELVIC INJURIES
The pelvic ring fracture should be differentiated from isolated acetabular fracture or pelvic avulsion fractures. There are various classifications of pelvic ring injuries. Pennal classifies pelvic injuries based on the vector force into anterior-posterior compression (APC), lateral compression (LC), and VS.[5] Tile proposed a classification based on pelvic ring stability. Type A is stable because the posterior pelvic ring is not disrupted. Type B involves incomplete posterior ring disruption which has rotational instability but is vertically stable. Type C involved complete posterior and anterior ring disruption resulting in rotational and vertical instability.[6] The widely used by orthopedics and radiologists is the Young and Burgess classification.[7] This classification combines the mechanism of injury with fractures and associated injuries along with their management. Figure 3 explains the mechanism of impact and associated fractures. Table 1 compares various classification systems.
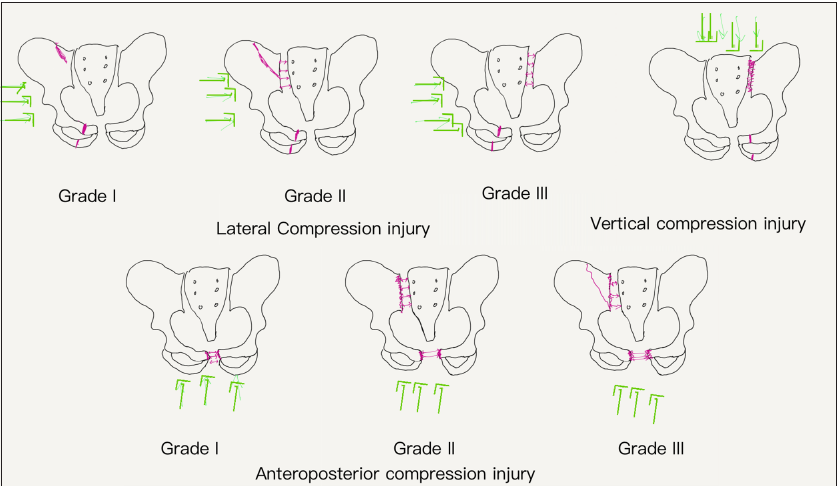
- Line diagram of classification of pelvic injuries which is based on the type of impact (green arrows) and resultant fractures (pink lines). The double-headed pink arrows represent diastasis. LC: Lateral compression, AP Grad: Anteroposterior compression grade
| Grade | WSES | Young and Burges | Pennal | Tile | Mechanical stability | Hemodynamic stability | CT | Management |
|---|---|---|---|---|---|---|---|---|
| Mild | Grade I | APC-I, LC-I | AP, LC | Type A | Stable | Stable | Yes | Conservative |
| Moderate | Grade II | APC-II/II, LC-II/III | AP, LC | Type B | Unstable-rotationally | Stable | Yes | Internal fixation, AE if active bleed. |
| Grade III | VS | VS | Type C | Unstable- vertically | Stable | Yes | Internal fixation, temporary external fixators, AE if active bleed. | |
| Severe | Grade IV | Any | Any | Any | Any | Unstable | No | Surgical packing |
CT: Computed tomography, AE: Angioembolization, LC: Lateral compression, VS: Vertical shearing, AP: Anteroposterior, APC: Anterior-posterior compression
Lateral compression
Grade I – Stable - involves the anterior ring with unilateral or bilateral pubic rami fracture and is treated conservatively.[4] Figure 4 shows an un-displaced pubic ramus fracture with undisplaced iliac wing fracture which was managed conservatively.
Grade II – rotational instability – The anterior ring fractures are associated with ipsilateral SIJ diastasis, requiring surgical fixation.[4] Figure 5 shows comminuted acetabular fracture and ipsilateral SIJ diastasis treated with internal fixation.
Grade III – multidirectional instability (windswept pelvis) – the anterior ring fractures are associated with contralateral SIJ diastasis requiring surgical fixation and temporary external fixators.[4]
- (a) Non-contrast computed tomography (NCCT) pelvis coronal and (b,c) axials show undisplaced superior and inferior pubic rami fractures (black arrow) and undisplaced iliac wing fracture (white arrow). (d) Axial NCCT images show undisplaced subarticular fracture (black block arrow) without any diastasis. (e) Soft tissue window show extraperitoneal hematoma (black star) surrounding the bladder. (f) A 3D reconstruction image shows undisplaced iliac wing fracture (white arrow). No diastasis is seen suggesting stable type I injury.
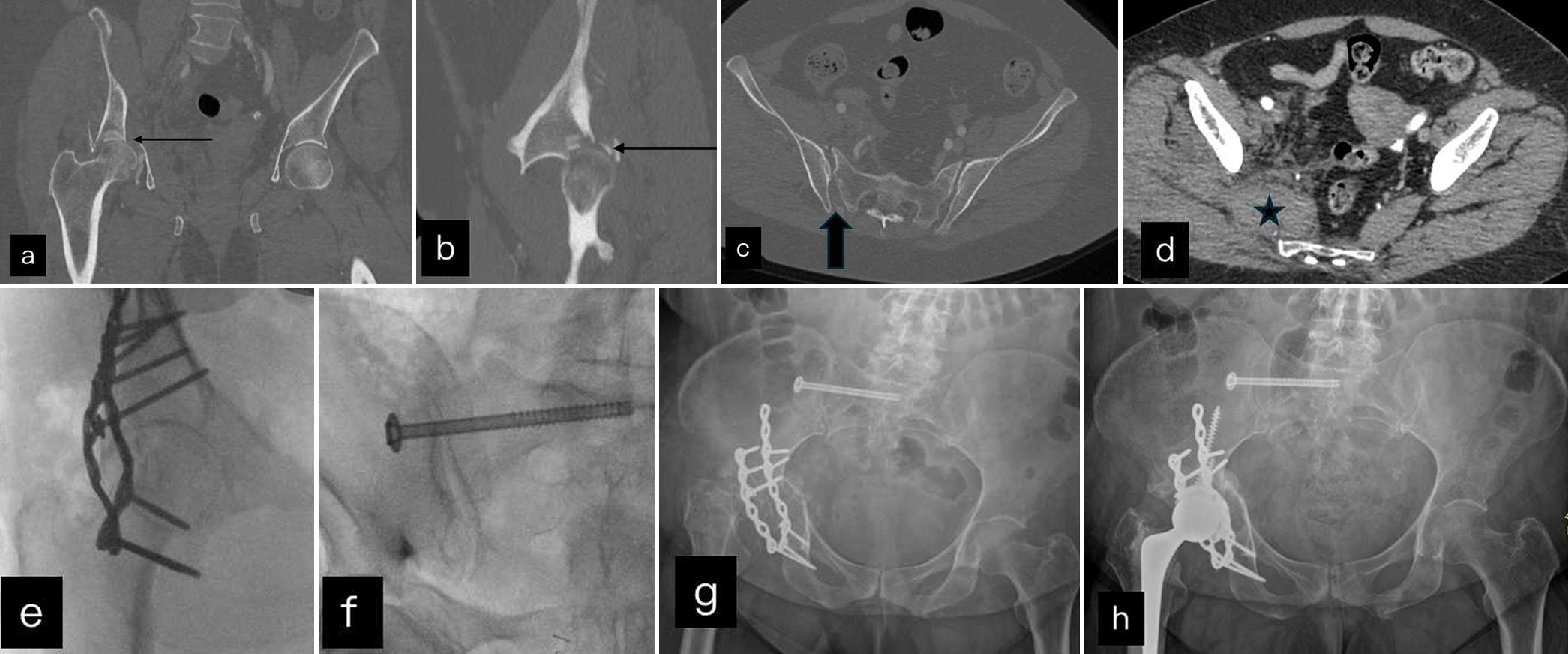
- (a and b) Coronal and sagittal reformats of NCCT show comminuted displaced acetabular fracture (black arrow) with posterior femoral displacement. (c) Shows diastasis of right sacro-iliac joint (black block arrow) and chip fracture of ilium. (d) Axial soft tissue window shows right pyriformis hematoma (black star). (e and f) Intra operative fluoroscopy images where unstable acetabular and posterior ring fracture were fixed internally. (g) Post operative X rays shows lysis of femoral head. (h) Post operative radiographs shows subsequent arthroplasty done with right femoral head prosthesis.
Anterior-posterior compression
The force vector is in an AP direction and resulting fractures result in open book configuration.
Grade I – Stable – The pubic symphysis diastasis is <2.5 cm, and it may be associated with vertical pubic rami fractures. The treatment is conservative.[4]
Grade II – Rotational instability – Pubic diastasis is more than 2.5 cm with vertical pubic rami fractures and anterior SIJ diastasis which requires surgical fixation.[4]
Grade III – Multidirectional instability – pubic diastasis more than 2.5 cm with vertical pubic rami fracture and anterior as well as posterior SIJ diastasis. The treatment requires surgical internal fixation.[4]
Vertical shearing
The force vector is craniocaudal resulting from a fall from height – multidirectional instability (Malgaigne) – there are vertical fractures of the iliac wing, sacrum, and SIJ diastasis resulting in posterior arch disruption along with anterior ring vertical fractures, which requires surgical fixation. There is avulsion fracture of transverse process of the fifth lumbar vertebra on the ipsilateral side which represents rupture of the iliolumbar ligament and posterior ring disruption.[8] Figure 6 represents bilateral pubic and vertical sacral fractures with SIJ diastasis. The fracture extends into transverse process of the fifth lumbar vertebra, suggesting posterior ring disruption which requires internal fixation as well as a temporary external fixator.
- (a and b) Non-contrast computed tomography coronal and axial images show displaced superior and inferior pubic fracture (black arrows). (c and d) Axial and coronal through the sacrum show zone I sacral fracture with significant diastasis (black block arrow) and avulsed fracture of transverse process (white block arrow). (e) Axials soft tissue window show pelvic hematoma (black star). This is a type III injury. (f) and (g ) Axial post operative CT and radiographs show internal fixation screws (white arrow) and temporary external fixator (black arrow head). (h) Axial CT shows temporary external fixator (black arrow head).
Combined mechanisms
In high-energy trauma, there is usually a combination of the above-mentioned forces. The most common type of combined mechanism is LC and VS injury.[9] There is usually multidirectional instability, and the treatment is surgical internal fixation.[4]
WORLD SOCIETY OF EMERGENCY RADIOLOGY (WSES CLASSIFICATION)
The WSES classification takes into account the anatomy of injury and hemodynamic instability. The patient is considered hemodynamically unstable if the systolic blood pressure (BP) is <90 mmHg and heart rate is >120 beats/minute with evidence of vasoconstriction, altered level of consciousness, and/or shortness of breath.[10] The WSES classified pelvic injuries into
Mild – Grade I – Anatomically and hemodynamically stable
Moderate – Grade II and III -– Hemodynamically stable and mechanically unstable
Severe –- Grade IV – Hemodynamically unstable irrespective of mechanical stability.
SACRAL FRACTURES
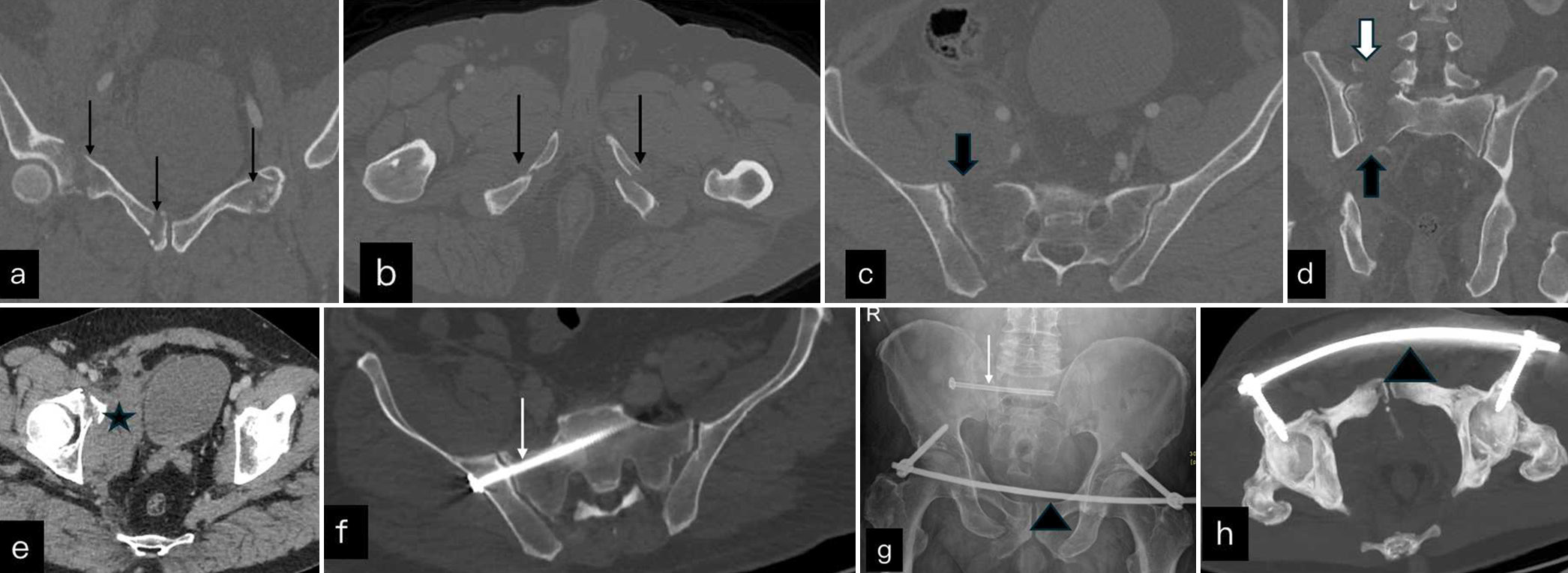
Isolated fractures are rare and are usually associated with other injuries of the pelvis.[4] The sacrum is divided into three zones as seen in Figure 7. Based on the location in relation to the zone, Denis et al. classified the sacral fractures into three zones as seen on AP radiographs.[11]
- Sacrum radiograph divided by four imaginary lines into three zones. The zone lateral to the red lines on each side represents zone 1. The area between green and red lines on each side represents zone 2 which contains sacral foramina and area between two green lines represents zone 3 which contains central canal.
Zone 1: Lateral to the neural foramina.
Zone 2: Involves the neural foramina.
Zone 3: Fracture is medial to the neural foramen involving sacral canal. There is high risk of neural injuries in this zone with resultant bowel and genitourinary dysfunction. The fracture involving central vertebral body can be further classified into four types on lateral radiograph as type 1: There is kyphotic angulation at the
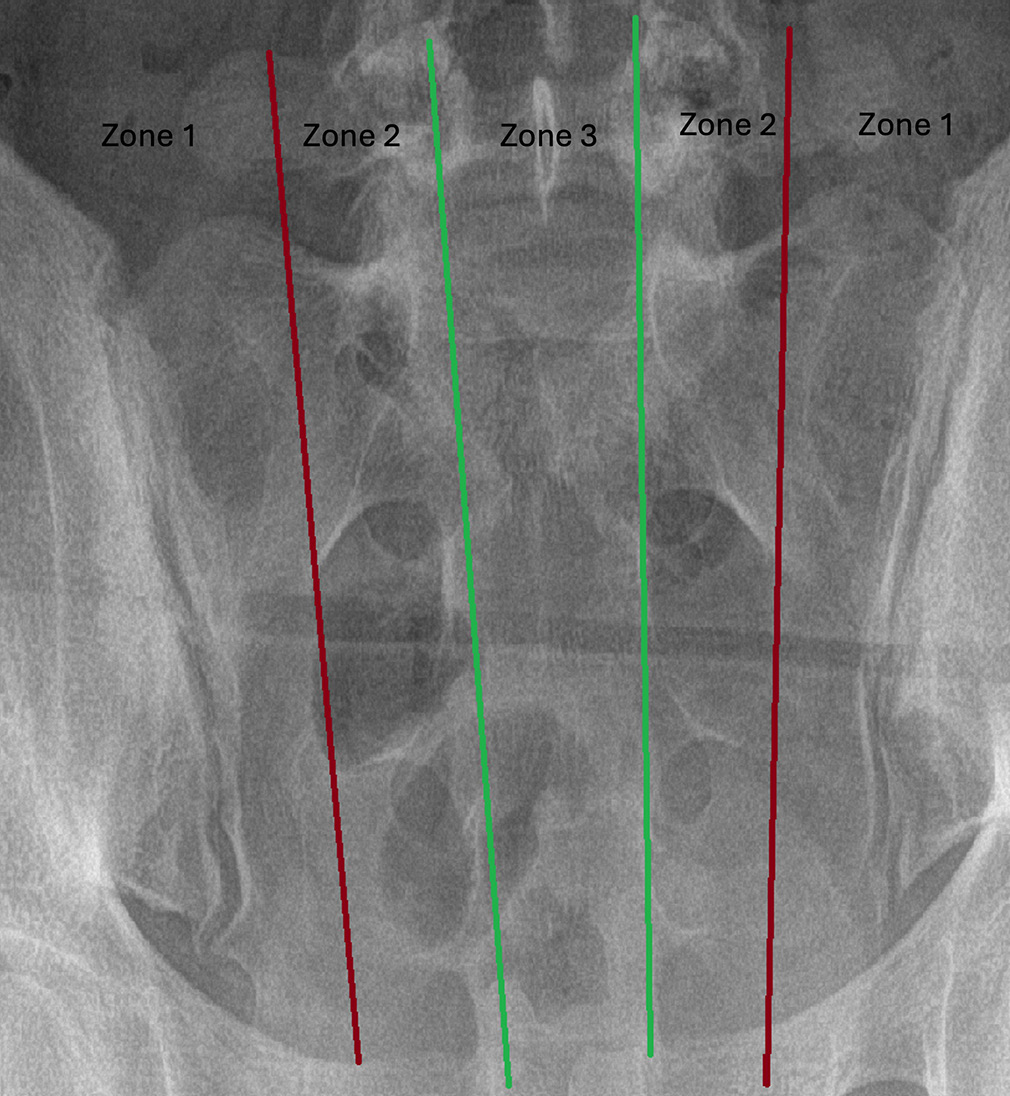
As shown in Figure 8, there is vertical zone 2 fracture with diastasis requiring internal fixation. The fractures involving zone-2 and 3 can have neurological deficits if nerve roots are involved.
- (a and b) Coronal imagest of CT shows a zone 2 sacral fracture (black block arrow) through left sacral ala with mild diastasis associated with undisplaced superior pubic fracture (white arrow) in (b). (c) Post operative radiograph and (d) non contrast computed tomomography pelvis shows intramedullary nails across the SI joint and complete healing of the fracture.
ACETABULAR FRACTURES
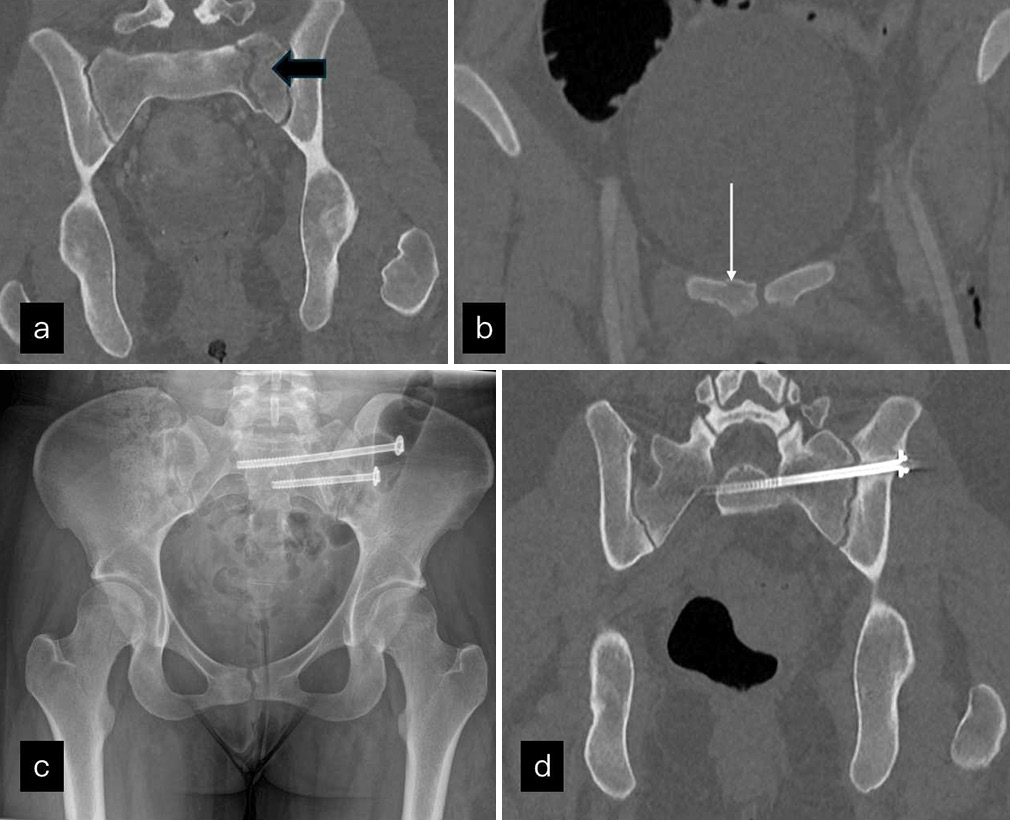
Isolated acetabular fractures can be seen in pelvic trauma. X-ray can identify the fracture by the disruption of normal lines as seen in Figure 9. CT is required for surgical planning and classification. The acetabular fractures are classified into 5 types as shown in Figure 10.[12] Figures 11 and 12 show isolated acetabular T-shaped fractures and stable fractures involving anterior wall pubic symphysis, respectively. As shown previously in Figure 5, unstable acetabular fracture associated with SIJ diastasis requires internal fixation.
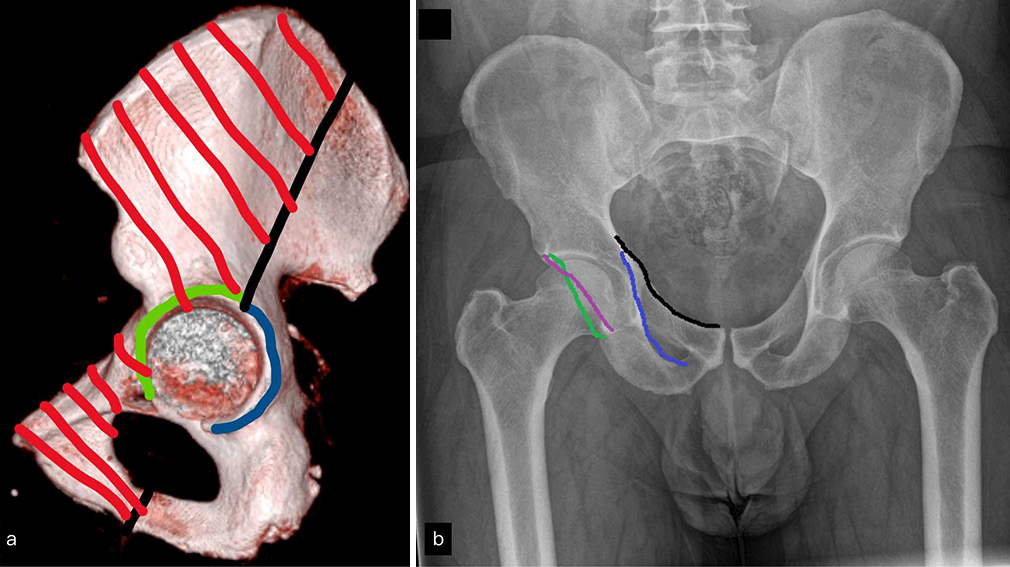
- (a) 3D reconstructed image of hemipelvis where green line represents anterior wall, blue line posterior wall, shaded red area anterior column, and unshaded area posterior column. (b) A pelvis anteroposterior radiograph with black line representing iliopectineal line, purple line representing ilioischial line, green line representing anterior acetabular wall, and blue line representing posterior acetabular wall. Any discontinuity in the above-mentioned lines on radiograph is sign of acetabular fracture.
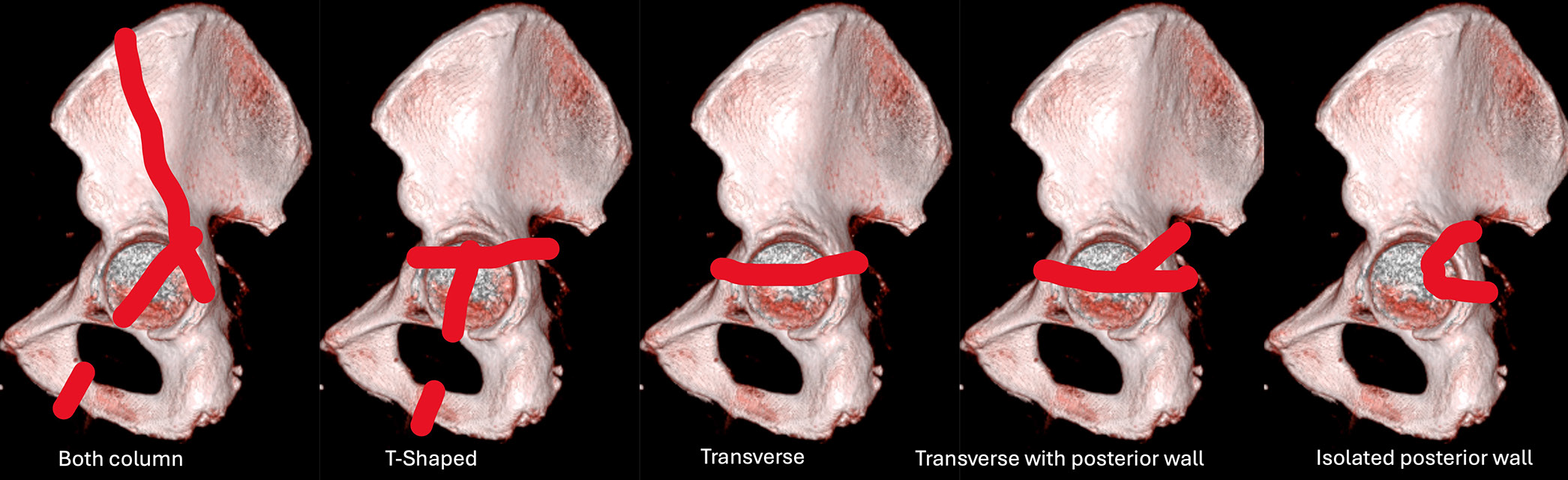
- Representation of the five types of acetabular fracture pattern on 3D hemipelvis.
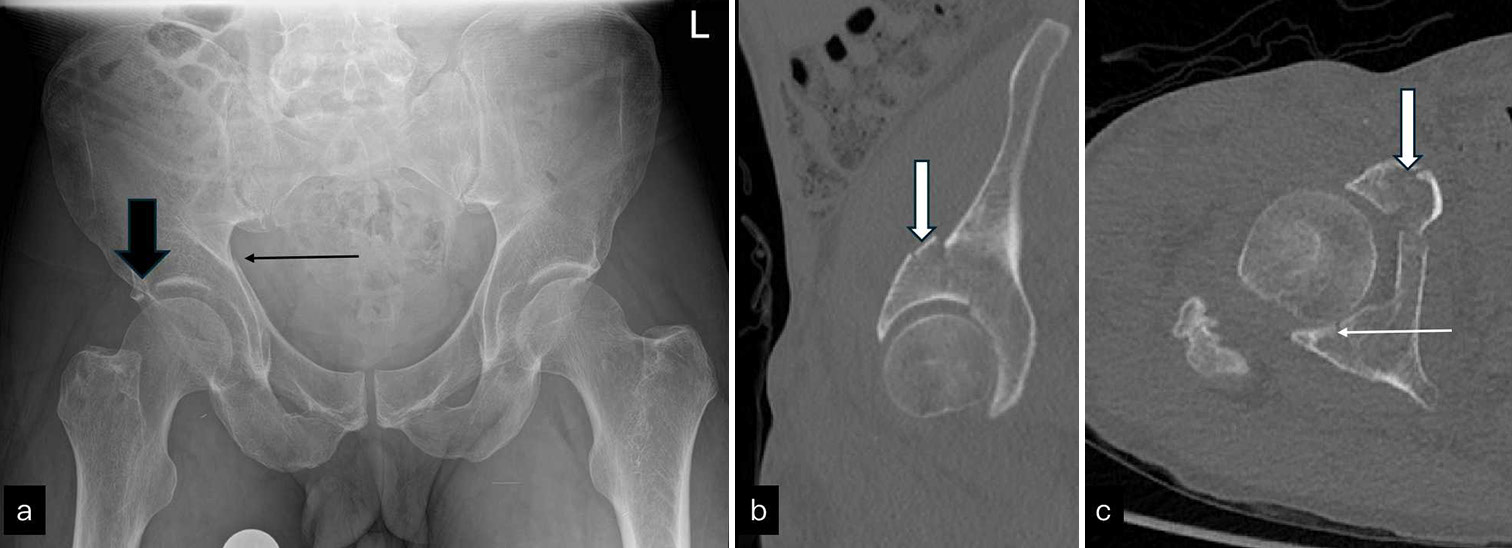
- (a) AP radiograph of pelvis shows break in iliopectineal (long black arrow) and roof of acetabulum (black block arrow). (b) Sagittal non-contrast computed tomography images show minimally displaced anterior column fracture (white block arrow in b and c). (c) shows undisplaced posterior wall fracture (white arrow). AP: Anterior posterior
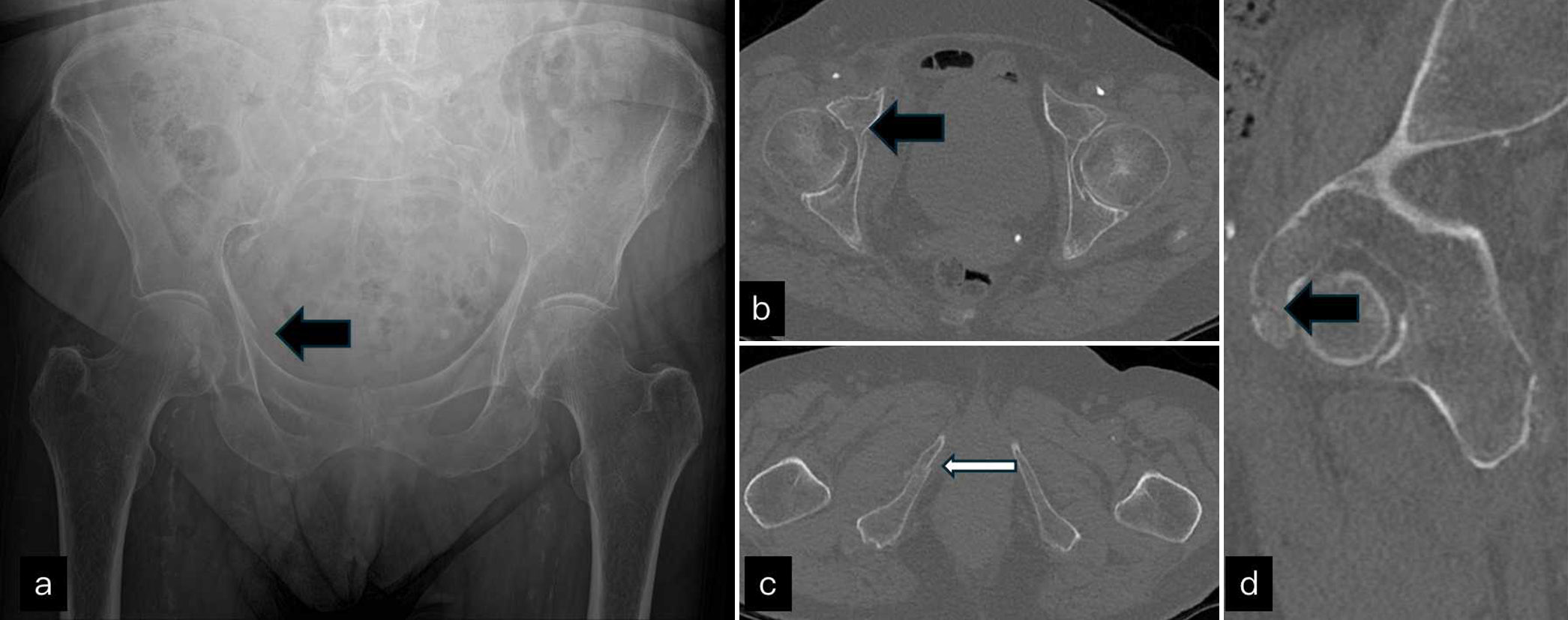
- (a) Anteroposterior pelvis radiograph shows a break in iliopectineal line (black block arrow) on right side. (b-d) non-contrast computed tomography axial images through hip joint and inferior pubic ramus and sagittal images show pubic fracture (black block arrow) which extends to involve anterior wall of acetabulum on sagittal image and undisplaced inferior pubic ramus fracture (white arrow). This can be treated conservatively.
Femur fracture
Based on the location of the fracture, the femur neck fractures are classified as subcapital, mid cervical, and intertrochanteric as seen in Figure 13.[13] X-ray is diagnostic. However, CT scan can be requested by the clinician if there is concern for femoral head involvement. Intertrochanteric fractures and mid-cervical fractures are treated by intramedullary nailing. Sub-capital femoral neck fractures, especially in the elderly, are subjected to arthroplasty. Figure 14 shows classical traumatic femur fracture treated by arthroplasty. Figure 15 shows atypical fracture in patient taking bisphosphonates. Although they are not true fractures, but can progress into complete fractures, they are treated with intramedullary nailing.[14]
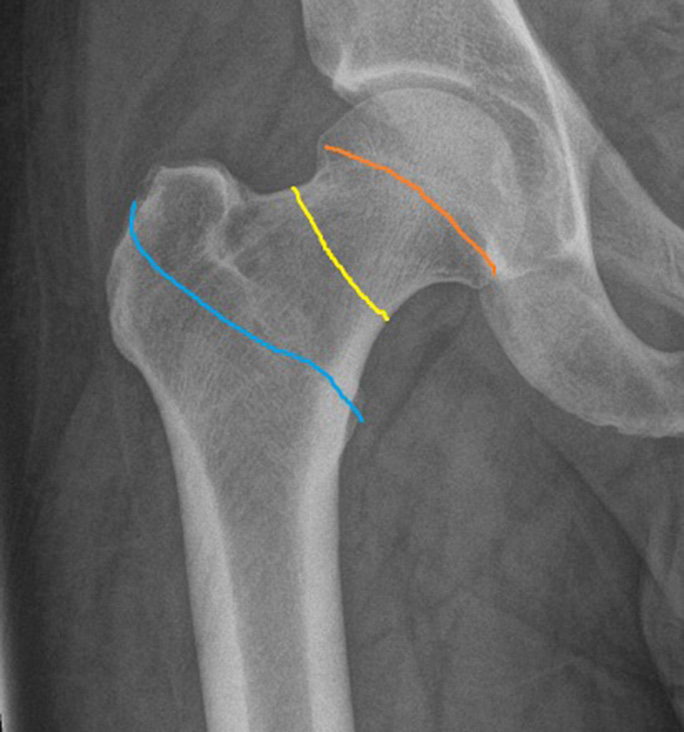
- Anteroposterior radiograph of right hip joint shows three types of femoral neck fracture. The orange line represents subcapital, yellow line represents mid cervical, and blue line represents intertrochanteric fracture.

- (a-d) Anteroposterior radiograph of pelvis (a) and non-contrast computed tomography coronal images (b) demonstrate minimally displaced subcapital fracture (white block arrow) which was treated with femoral head replacement (c and d).

- (a) AP radiograph shows focal cortical bulge in proximal lateral femoral cortex (white block arrow). (b) Zoomed in image shows horizontal lucency and periosteal reaction (white block arrow) in keeping with atypical femoral fracture. (c and d) T2FS axial and coronal MRI shows periosteal edema along lateral femoral cortex and marrow edema (white block arrow). (e) Intraoperative fluoroscopic images show prophylactic intramedullary nailing done for this fracture. AP: Anteroposterior
The femur fracture can be isolated or associated with pelvic injuries. When associated with ipsilateral fracture of the pelvis and/or acetabulum, the proximal femoral shaft fracture results in floating hip injury which requires surgical treatment.[15] In high-energy trauma and comminuted acetabular fractures, there is telescoping of femoral head as shown in Figure 5. Figure 16 shows femoral shaft injury with pelvic dissociation in a degloving injury of pelvis secondary to run over by tractor.
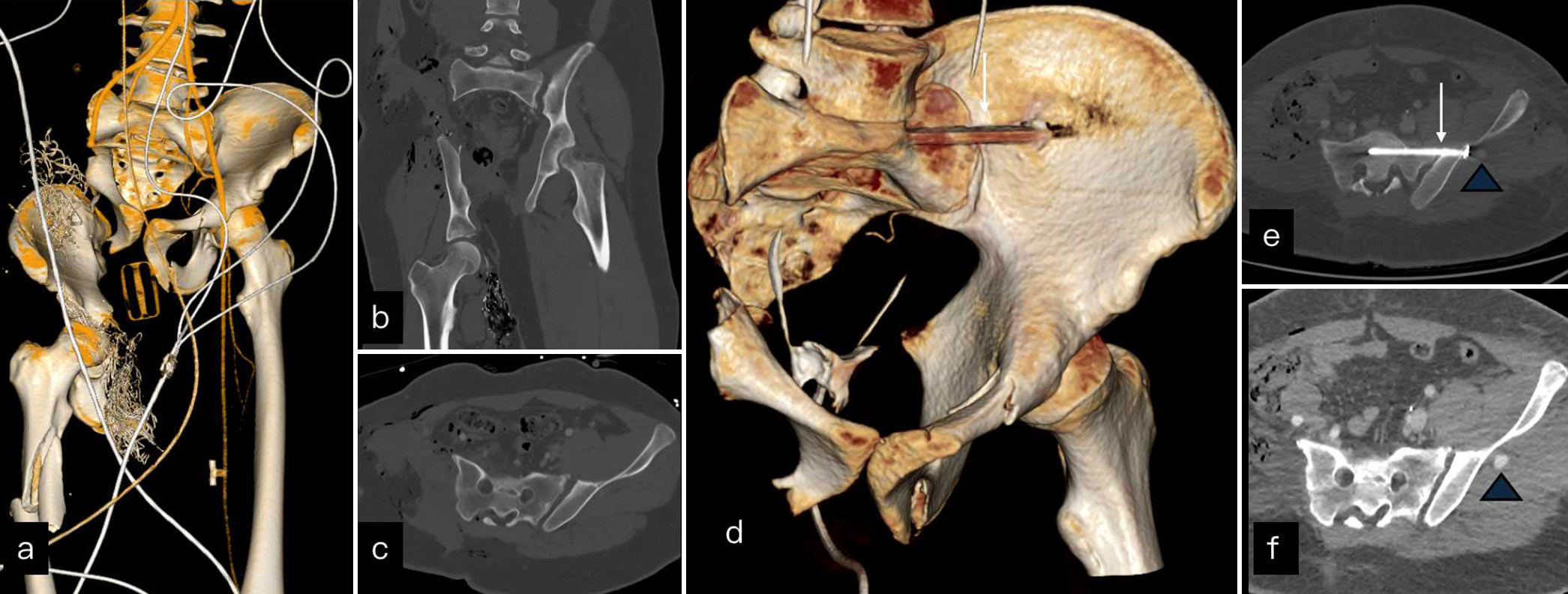
- A young cyclist was runover by a tractor. (a) 3D reconstruction shows displaced right hemipelvis and femur shaft fracture. (b and c) The coronal and axial images show degloving injury of right lower limb and diastasis of left sacroiliac joint (SIJ). (d) 3D reconstructed image shows right hemipelvectomy and lower limb amputation done with internal fixation screw (white arrow) across left SIJ. (e and f) Follow up contrast scan shows iatrogenic aneurysm (blue arrow head) post internal fixation.
ASSOCIATED SOFT TISSUE INJURIES
As pelvis hosts a few vital organs and vessels, the pelvic fractures are commonly associated with soft tissue injuries. It is important for radiologist to be aware of all the injuries and associated signs and should be able to pick up even on unenhanced scan.
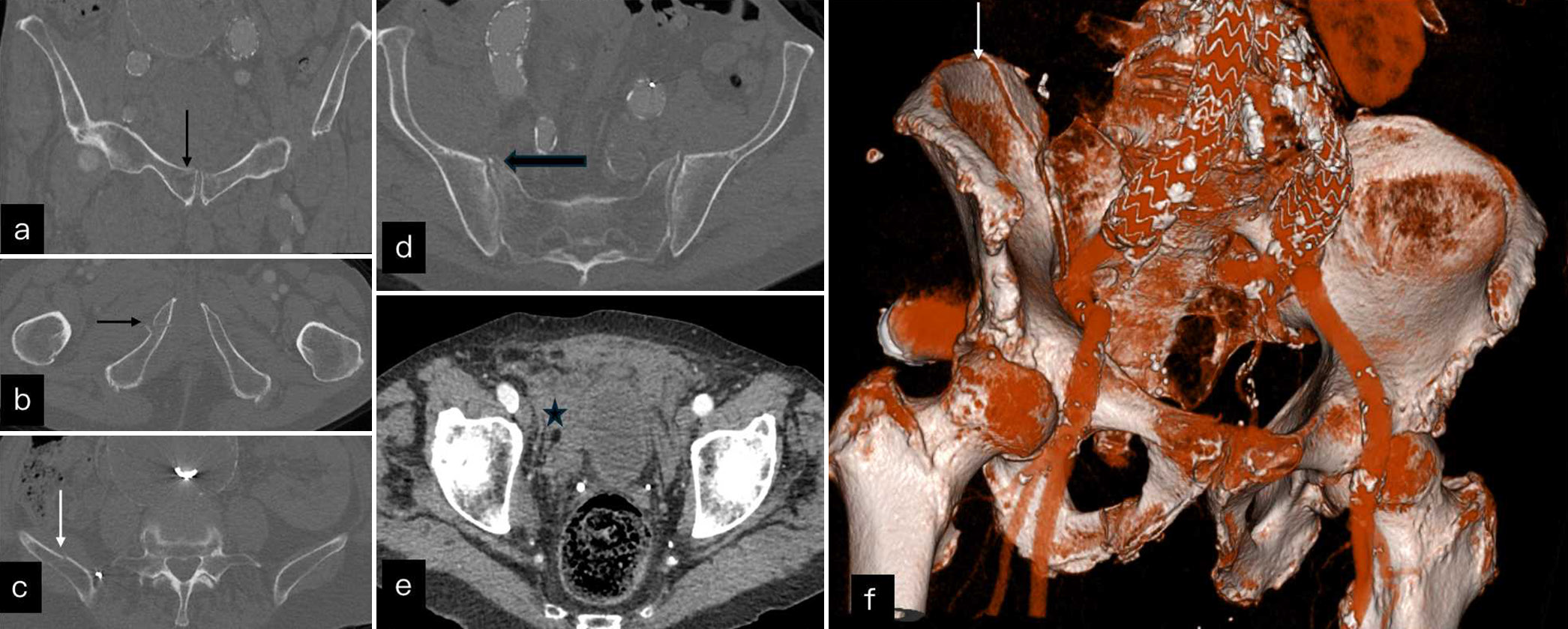
Vascular injuries
Vascular injuries associated with pelvic fractures can be life threatening if not urgently treated. Corona mortis is the variant anastomosis between external iliac and inferior epigastric artery overlying symphysis pubis.[16] When injured, it can be catastrophic. Dual-phase CT angiography should be done to look for vascular injuries. The routine trauma scan is acquired in mixed arterial and venous phase. If there is suspicion of vascular injury as evidenced by fluctuating vitals and BP, an additional venous phase should be acquired. Vascular injury can be identified as vascular blush persisting in the second phase. There can be free intraperitoneal or retroperitoneal spillage with surrounding hematoma. Alternatively, a traumatic pseudoaneurysm can also be formed. Figure 16 shows pseudoaneurysm developed in iliac wing fracture post-surgical fixation. Figure 16 shows degloving injury of lower limb which was treated with hemipelvectomy and lower limb amputation. Figure 17 shows different vascular injuries associated with pelvic fractures.
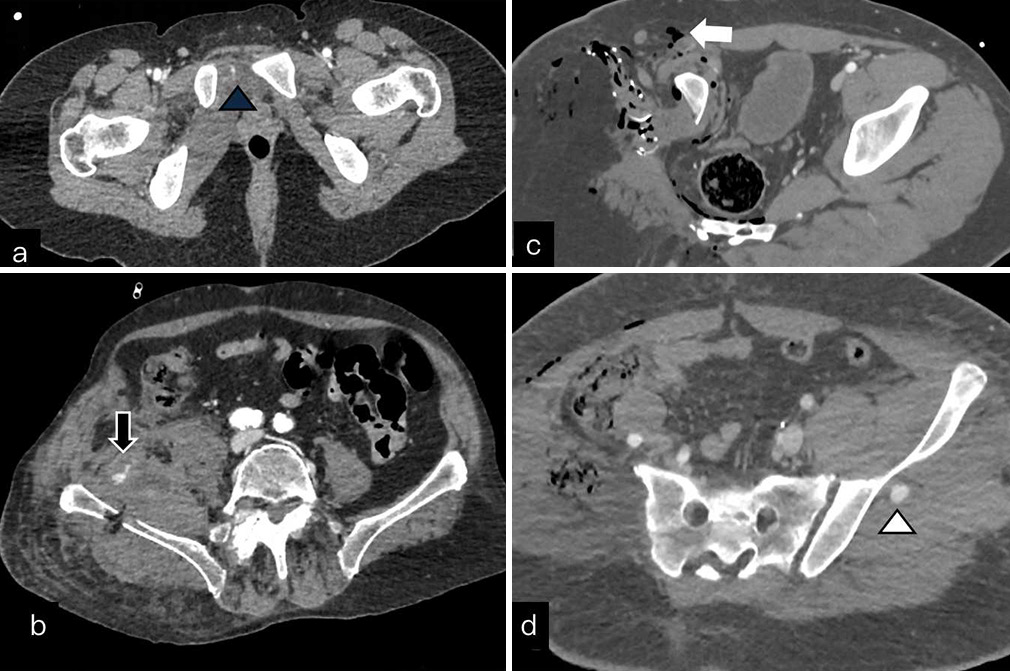
- Vascular injuries: (a) Axial images contrast CT show small contrast blush (blue arrow head) surrounding the pubis. (b) Axial images show comminuted iliac fracture with surrounding hematoma with active contrast extravasation (white block arrow) suggesting traumatic psueodaneurysm. (c) Axial CT in degloving injury of lower limb shows complete thrombus of femoral vessels (black arrow). (d) Post operative images show iatrogenic aneurysm (white arrow head) in left gluteal region. CT: Computed tomography
Bladder injuries
Bladder injuries can commonly occur in pelvic fractures. They can be divided into intraperitoneal and extraperitoneal rupture. The intraperitoneal rupture is characterized by defect in dome of urinary bladder which has peritoneal lining with associated urinary ascites.[17] A tear or injury of rest of the walls results in extraperitoneal bladder rupture. Extraperitoneal rupture is more common than intraperitoneal bladder rupture in traumatic injuries of the pelvis.[18] There should always be a radiologist doing a primary survey scan of polytrauma patients and if there is suspicion of bladder injuries, additional delayed phases are required to look for contrast extravasation. In cases with comminuted pelvic bone fractures and in patients with hematuria, CT cystography must be done for complete evaluation of the bladder injury.
As shown in Figure 18, intraperitoneal bladder rupture is characterized by rent in the dome of bladder, and extra-peritoneal rupture is characterized by contrast extravasation in extraperitoneal space.
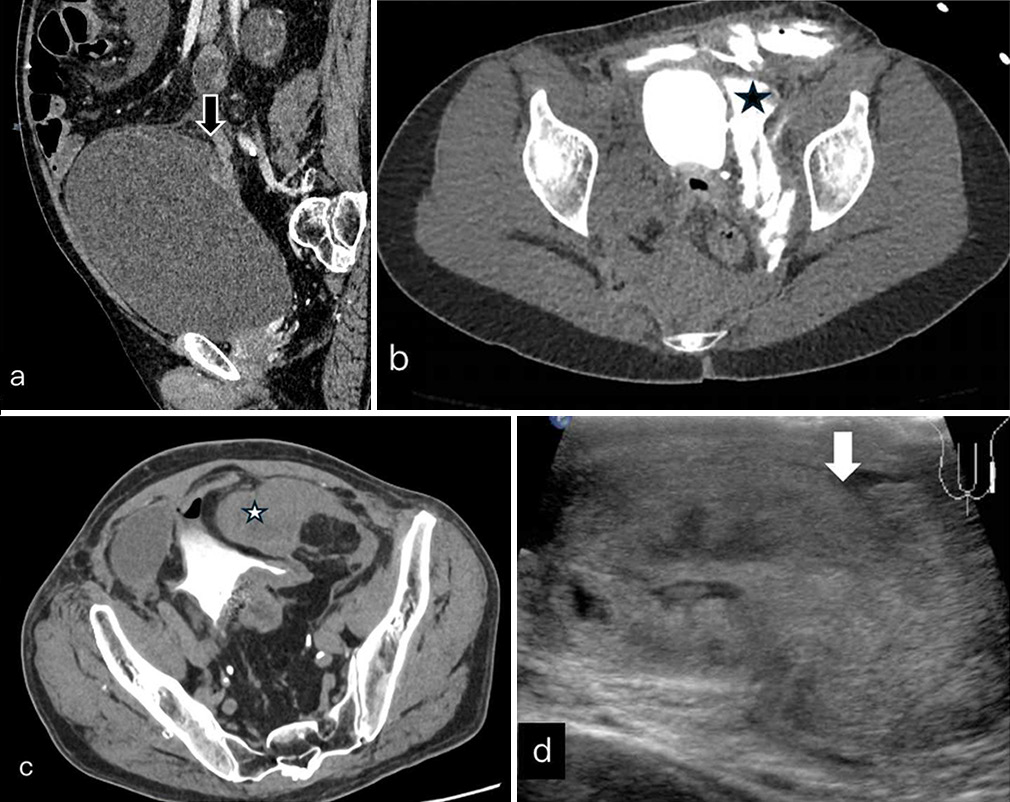
- (a) Sagittal soft tissue window show overdistended urinary bladder with large defect in dome of bladder (black block arrow). (b) Axial delayed images show hyperdense ascites (white star) suggesting intraperitoneal bladder rupture. (c) Axial post contrast delayed CT of another patient show extravasation of contrast in extra-peritoneal space (black star) and subcutaneous tissue of abdominal wall suggesting extra-peritoneal bladder rupture. (d) Ultrasound images of scrotum show large testicular hematoma with altered contour (white block arrow) in keeping with testicular rupture. CT: Computed tomography
Urethral injuries
They can be associated with high-energy pelvic trauma affecting mainly the posterior urethra.[19] For suspected urethral injuries, retrograde urethrography is the first investigation to be done. CT diagnosis is made by contrast extravasation in the extraperitoneal space and proximal thigh. The urinary catheterization is first-line treatment and long-term sequelae can be urethral stenosis which can be managed by delayed urethroplasty.
Neural injuries
Neural injuries are associated with sacral fractures involving zone II and III. They present with bladder/bowel dysfunction, erectile dysfunction, or neurogenic pain in lower limbs. Sometimes, large hematoma compression lumbar plexus can present with radiating type of pain in the legs. VS injuries of the pelvis are associated with lumbosacral plexus injuries.[20]
Scrotal and testicular injuries
Scrotum and testis injuries are common due to superficial location. They may or may not be associated with pelvic fractures. Scrotal hematoma can be identified on CT scan. USG is the investigation of choice for testicular trauma.[21] As shown in Figure 18, the testicular rupture requires orchidectomy.
Muscle injuries
The pelvic muscle injury is a common cause of traumatic hip pain. They can rarely be associated with high-energy pelvic trauma or are isolated in sports injuries. Muscle, musculotendinous junction, tendon and tendon attachment site injuries of adductor, hamstring and quadriceps compartments are common in sports like soccer. The radiographs are usually normal or sometimes demonstrate soft tissue swelling. MRI is the most sensitive investigation for muscle injuries and hence investigation of choice.[22] When MRI is not readily accessible, USG can be a cost effective and non-invasive alternative. USG can identify both active and chronic injuries. Figures 1, 19-21 show three different patients presenting with muscle injuries of hip and proximal high.
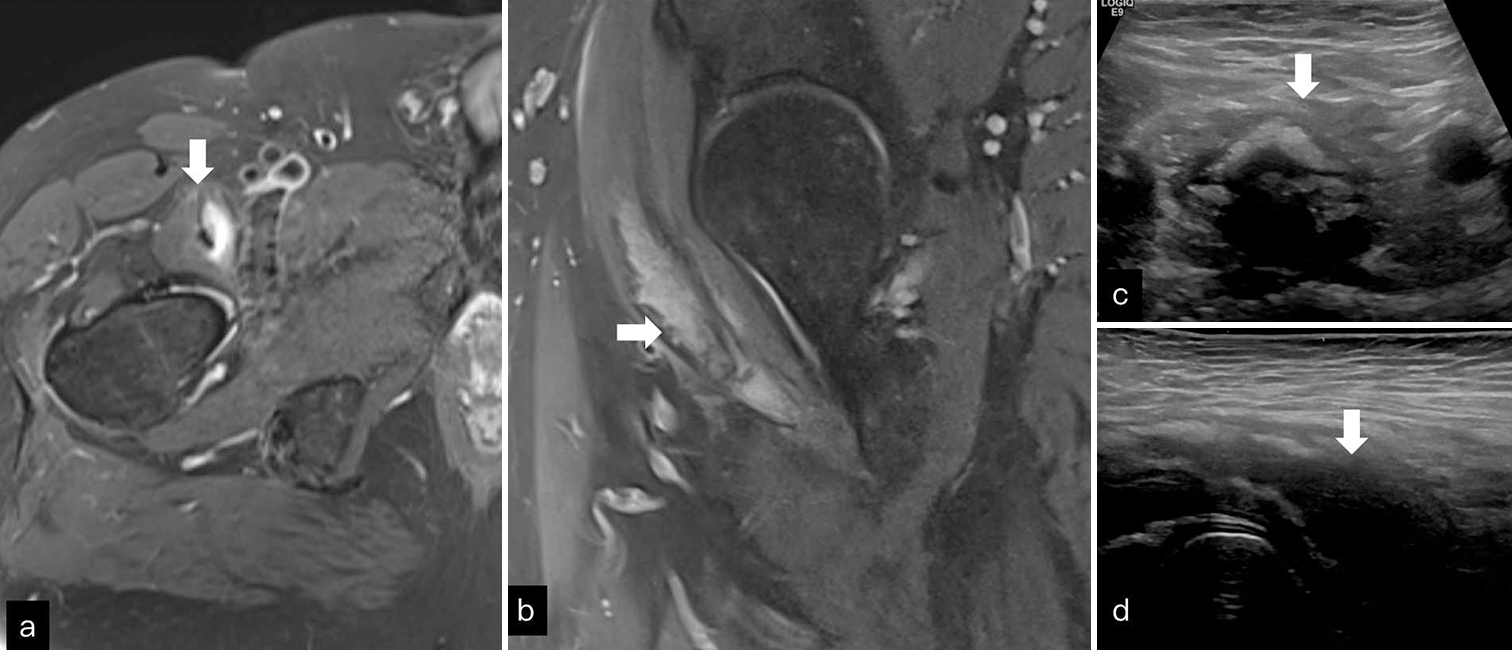
- (a and b) Axial and coronal T2FS images through right hip shows intrasubstance collection (white block arrow) within iliopsoas suggesting partial tear. (c and d) Short axis and long axis ultrasound images of iliopsoas show hypoechoic collection with calcification (white block arrow).

- (a-c) Axial and coronal T2 fat saturated images through thigh show irregularity of vastus origin (white block arrow) from femur and intramuscular edema (black block arrow) within the axial images through distal thigh.
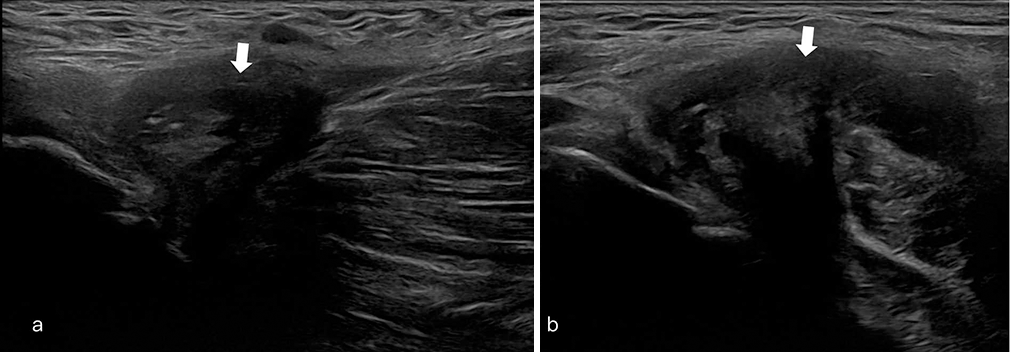
- (a) and (b) Short axis and long axis ultrasound images through adductor origin show intramuscular hematoma (white arrow).
Occult injuries in elderly
Minor trauma and falls are common in elderly population. As the bones of the elderly are severely osteopenic, radiographs are often normal and MRI is preferred investigation of choice.[23] MRI can detect subtle fracture due to marked edema surrounding the fracture. Usually, a fast protocol is adopted, containing T2W fat saturated axial and coronals and T1-weighted coronal. Sagittal images are optional. Figure 22 shows elderly patient with fall. The X-ray is normal, but MRI shows undisplaced fracture of pubic symphysis as well as stress fractures of the sacrum.
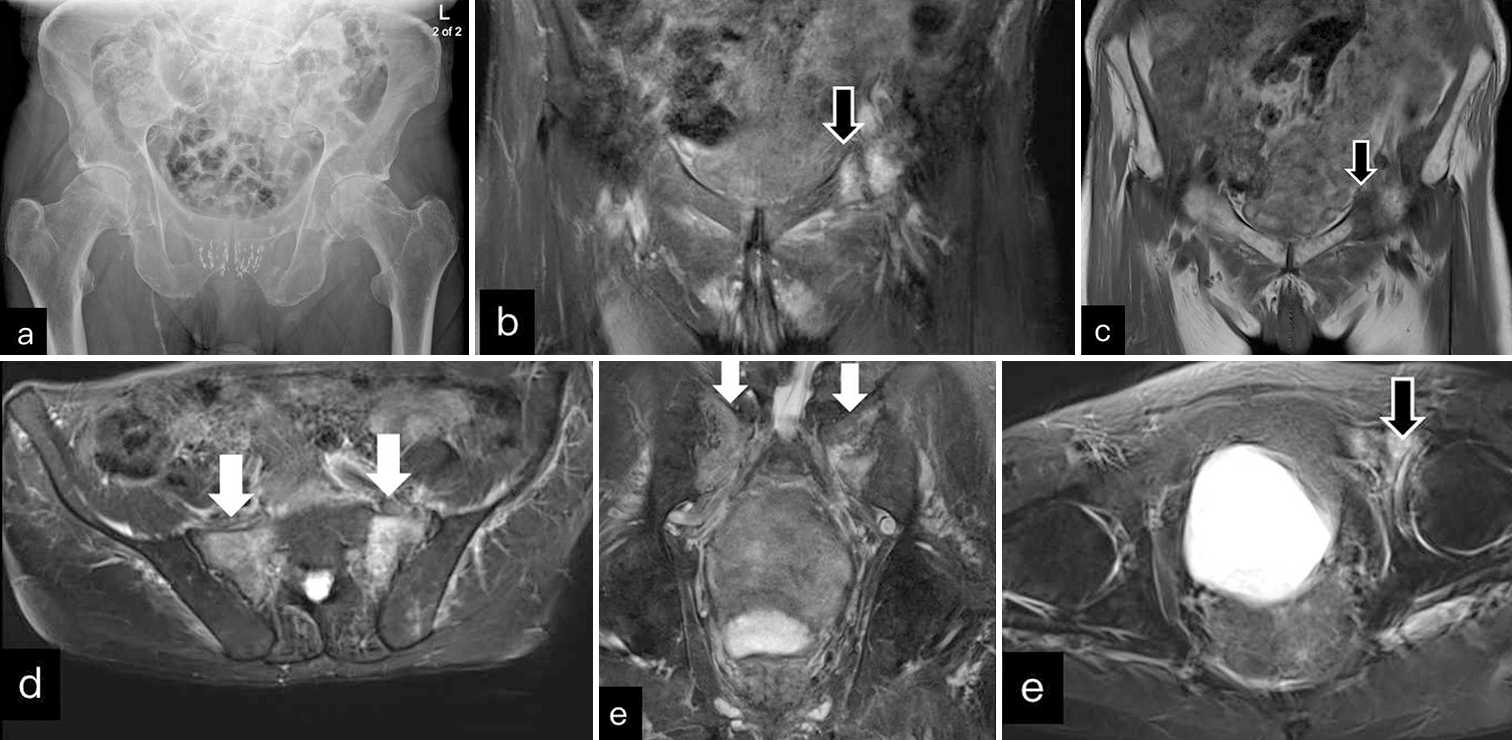
- An elderly patient presented with fall. (a) AP radiograph was unremarkable. (b and c) Coronal T2 fat saturated (FS) and T1WI images show undisplaced left superior pubic ramus fracture (black block arrow). (d and e) Axial and coronal T2FS show extensive bilateral sacral edema with hypointense line (white block arrows) in keeping with sacral insufficiency fracture. (f) Axial T2FS image show undisplaced left superior pubic ramus fracture (black block arrow) with surrounding edema. AP: Anteroposterior
CONCLUSION
Pelvic trauma is usually associated with osseous as well as non-osseous injuries. A radiologist should be aware of the pattern of injuries and management. Various pelvic fracture classifications stress on importance of mechanical stability. The integrity of posterior ring is crucial in deciding conservative versus surgical approach. The pelvic ligaments play a crucial role in the integrity of pelvic ring and ligament injuries can result in instability. The association of vascular and soft tissue injuries requires multimodality involvement in the treatment. CT is investigation of choice in polytrauma, and radiologist should provide comprehensive description of injuries, based on which management is decided. Timely diagnosis and referral can be life saving for the patient.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Open pelvic fractures: Epidemiology, current concepts of management and outcome. Injury. 2005;36:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures (complex): assessment and management. 2016. Guidance NICE. Available from: https://www.nice.org.uk/guidance/NG37/chapter/recommendations. [Last accessed on 2024 Oct 19]
- [Google Scholar]
- Pelvic fractures and associated genitourinary and vascular injuries: A multisystem review of pelvic trauma. Am J Roentgenol. 2019;213:1297-306.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of periprosthetic fractures of the hip and knee. Semin Roentgenol. 2021;56:90-105.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic disruption: Assessment and classification. Clin Orthop Relat Res. 1980;151:12-21.
- [CrossRef] [Google Scholar]
- Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 1996;4:143-51.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic ring disruptions: Effective classification system and treatment protocols. J Trauma. 1990;30:848-56.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging review of pelvic ring fractures and its complications in high-energy trauma. Diagnostics (Basel). 2022;12:384.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic ring fractures: what the orthopedic surgeon wants to know. Radiographics. 2014;34:1317-33.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5.
- [CrossRef] [PubMed] [Google Scholar]
- Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67-81.
- [CrossRef] [Google Scholar]
- Classification of common acetabular fractures: radiographic and CT appearances. AJR Am J Roentgenol. 2006;187:915-25.
- [CrossRef] [PubMed] [Google Scholar]
- Proximal femoral fractures: What the orthopedic surgeon wants to know [published correction appears in Radiographics 2015;35:1624] Radiographics. 2015;35:1563-84.
- [CrossRef] [PubMed] [Google Scholar]
- Intramedullary nailing for atypical femoral fracture with excessive anterolateral bowing. J Bone Joint Surg Am. 2017;99:726-35.
- [CrossRef] [PubMed] [Google Scholar]
- The floating hip injury: A descriptive study and case-control analysis. HIP Int. 2024;34:122-33.
- [CrossRef] [PubMed] [Google Scholar]
- "Crown of Death"; Corona Mortis, a common vascular variant in pelvis: Identification at routine 64-slice CT-angiography. Bull Emerg Trauma. 2020;8:193-8.
- [Google Scholar]
- Imaging of genitourinary trauma. Am J Roentgenol. 2009;192:1514-23.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic bladder ruptures: A ten-year review at a level 1 trauma center. Adv Urol. 2019;2019:2614586.
- [CrossRef] [PubMed] [Google Scholar]
- Management of male pelvic fracture urethral injuries: Review and current topics. Int J Urol. 2019;26:596-607.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of vertical shear pelvic fracture associated with a lumbosacral plexus injury through the lateral-rectus approach: Surgical techniques and preliminary outcomes. Orthop Surg. 2022;14:1723-29.
- [CrossRef] [PubMed] [Google Scholar]
- Scrotal trauma: Interest of preoperative ultrasound in the prediction of the rupture of the tunica albuginea. Med Glas (Zenica). 2021;18:128-32.
- [CrossRef] [PubMed] [Google Scholar]
- Management of anterior thigh injuries in soccer players: Practical guide. BMC Sports Sci Med Rehabil. 2022;14:41.
- [CrossRef] [PubMed] [Google Scholar]
- Hip fracture: Diagnosis, treatment, and secondary prevention. Am Fam Physician. 2014;89:945-51.
- [Google Scholar]







