Translate this page into:
Lipoma in olecranon bursa: A case report

*Corresponding author: Shalini Agarwal, Department of Radiodiagnosis, Pandit Bhagwat Dayal Sharma, Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India. dragarwalshalini@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agarwal S, Siwach J, Wadi R, Gupta N. Lipoma in olecranon bursa: A case report. Indian J Musculoskelet Radiol 2021;3(1):67-9.
Abstract
We report a case of a 55-year-old male patient who presented with swelling over his right elbow of 5-year duration. An ultrasound examination revealed an echogenic mass within the olecranon bursa. On magnetic resonance imaging, the mass revealed the signal intensity of fat, and it was attached to the bursal lining by means of a pedicle. There was no restriction on diffusion-weighted images and no significant contrast enhancement. Excision was performed under local anesthesia. The excised specimen revealed mature fat cells on histopathology.
Keywords
Olecranon bursa mass
Intrabursal lipoma
Lipoma
INTRODUCTION
Lipomatous soft-tissue tumors are the most typical soft-tissue neoplasms encountered in clinical practice.[1] They have rarely been reported in intra-articular locations, especially in Hoffa’s fat pad and the suprapatellar pouch of the knee joint.[2] Isolated lipoma in a bursa is extremely rare.[3] To the best of our knowledge, only three cases have been reported so far. These were in the olecranon bursa,[4] superficial infrapatellar bursa,[3] and subacromial subdeltoid bursa.[5] Hence, they can be difficult to diagnose, especially when they are small. We report the second case of lipoma in olecranon bursa.
CASE REPORT
We report a case of a 55-year-old male who presented with swelling over the right elbow. The lesion had been present for 5 years but had grown more rapidly over the past 6 months. There was no history of trauma or infection. Peripheral blood examination, erythrocyte sedimentation rate, total leukocyte count, and C-reactive protein were within normal limits. Clinically, there was swelling over the right elbow with no signs of inflammation nor did the patient complain of pain or numbness in the forearm distally. On ultrasonography, there was a well-defined homogenous hyperechoic lesion measuring approximately 2.0 × 1.6 × 1.7 cm over the dorsal aspect of the right elbow showing no significant flow on color Doppler. It was located within the olecranon bursa [Figure 1]. There was no evidence of joint effusion or involvement of the underlying bone.
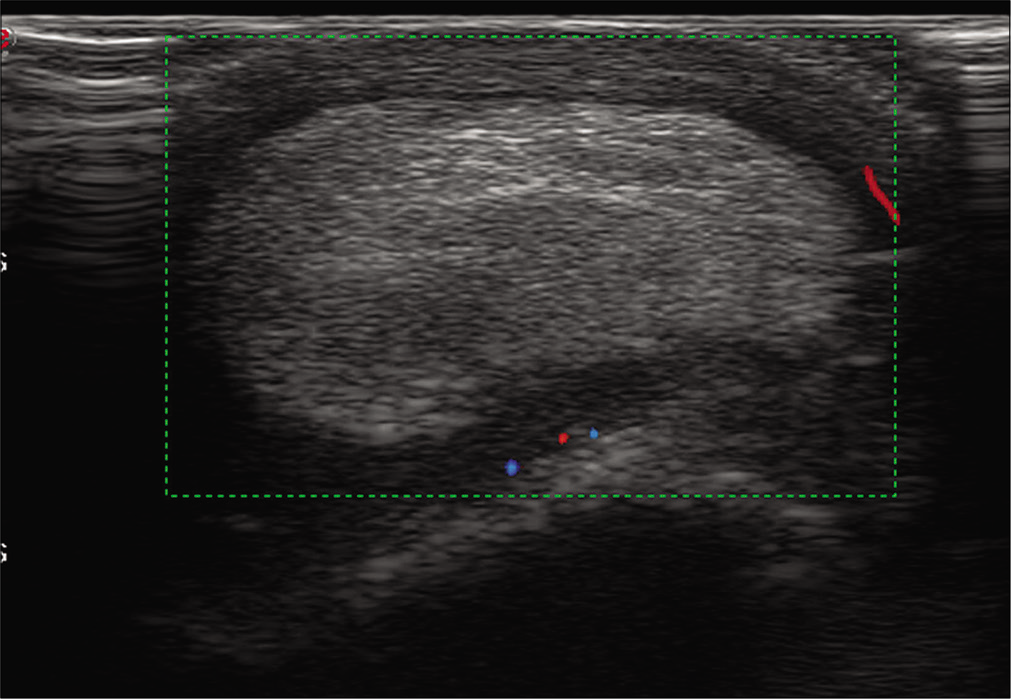
- Ultrasonography image reveals a well-defined echogenic mass lesion located within the olecranon bursa. There was minimal vascularity within the wall of the bursa and no vascularity within the mass itself.
Magnetic resonance imaging (MRI) of the mass showed high signal intensity on T1W and T2W images with suppression of signal on fat-saturated images [Figures 2 and 3]. There was no restriction on diffusion-weighted images and no significant contrast enhancement. Further, there was no connection with the joint. However, it was attached to the bursal lining by a stalk [Figure 4]. The lesion was excised under local anesthesia. A well-defined, oval lobulated smooth yellowish mass measuring 2 × 1.7 cm was excised and sent for histopathological examination. It was surrounded by a fibrous capsule and attached to the synovial lining of the olecranon bursa by a short stalk. Histology of excised specimen revealed sheets of mature fat cells without cellular atypia or metaplasia covered with a thin fibrous layer. There were few scattered lymphocytic infiltration, fibroblasts, and capillary network noted in the synovium. Immunohistochemistry with S100 antigen showed membrane positivity.
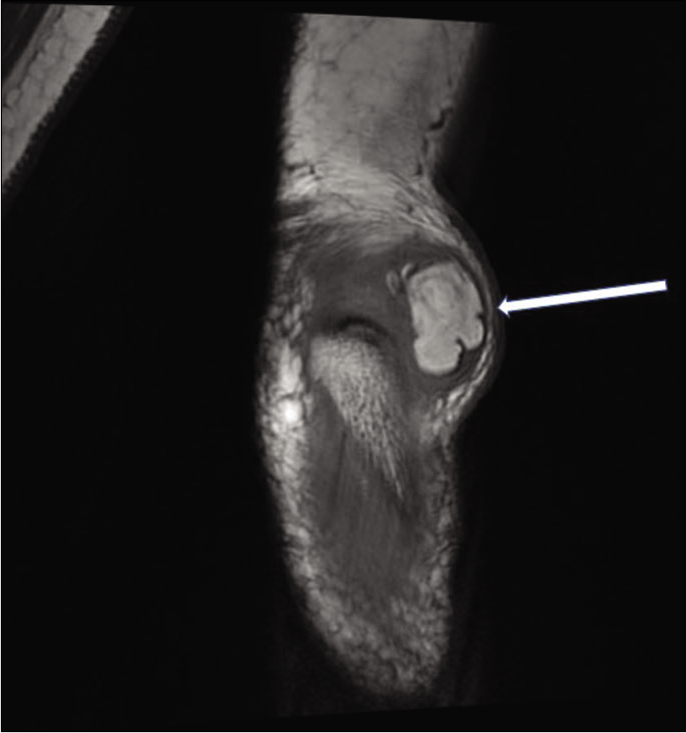
- T1-weighted coronal MR image reveals a well-defined uniformly hyperintense mass (arrow) lesion within the olecranon bursa.
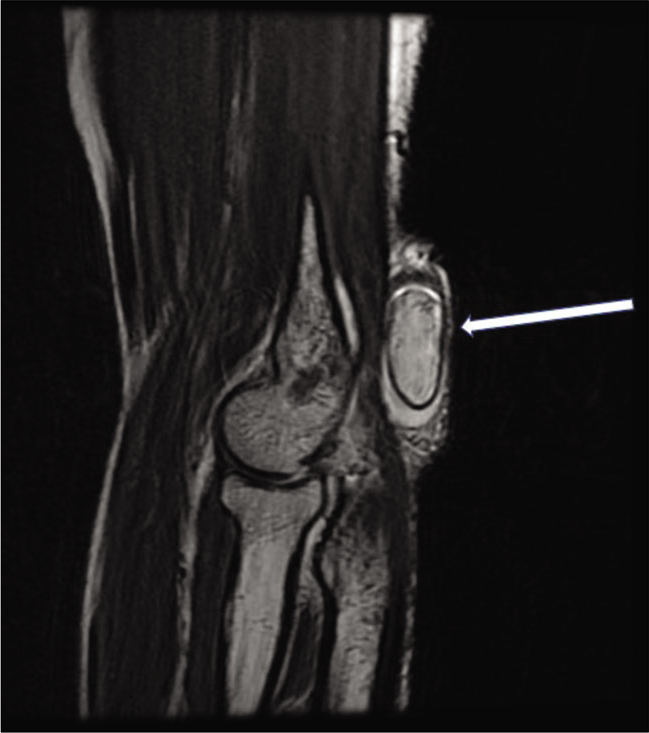
- T2-weighted sagittal MR image reveals a well-defined hyperintense mass lesion with a uniform hypointense capsule (arrow) within the olecranon bursa.
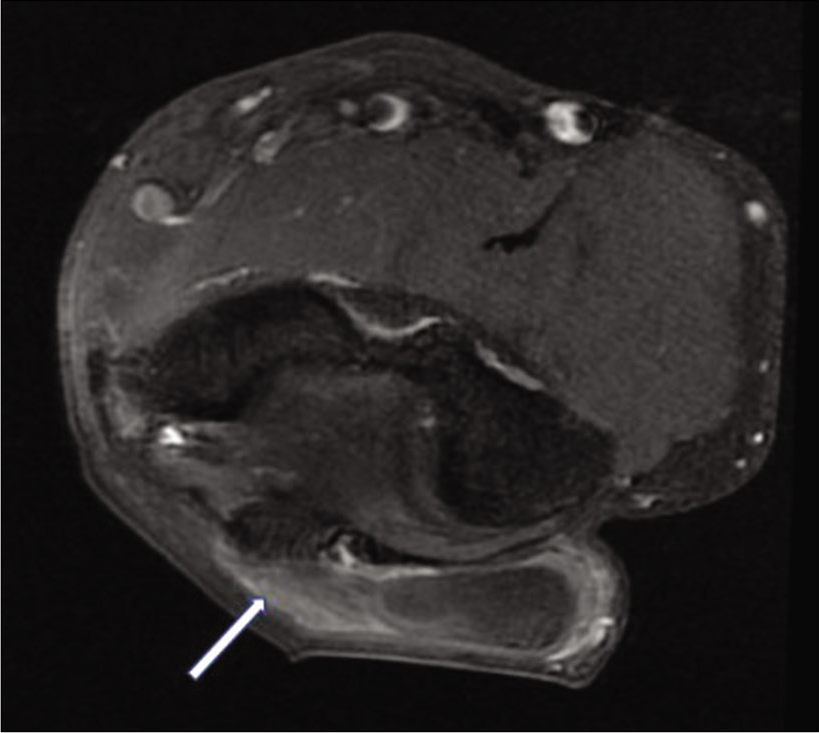
- Fat-suppressed contrast-enhanced axial T1-weighted image reveals a well-defined, non-enhancing mass lesion within the olecranon bursa. It is seen to be attached to the wall of the bursa, by means of a poorly enhancing stalk (arrow).
DISCUSSION
Sir James Paget first described lipoma in 1856, and in 1925, Bufalini first described the radiographic characteristics of this tumor. They named the radiolucency within the soft tissue, which is characteristic of this tumor, as the “Bufalini sign.” These tumors have been reported mainly in the subcutaneous planes. However, atypical lipoma presentations such as angiolipoma, chondroid lipoma, intramuscular, and intra-articular lipomas have also been reported.[1] Isolated lipoma in a bursa is extremely rare.[3]
Benign lipomas have a typical appearance. In the soft tissues, they appear echogenic on ultrasonography.[1] While on MRI, benign lipomas have a very typical imaging characteristic and are hyperintense on both T1W and T2W sequences, analogous to the intensity of subcutaneous fat.[6] In cases of malignancy, the soft-tissue component of these masses displays an heterogeneous signal intensity, and their signal is not isointense to subcutaneous fat. MRI is considered as the imaging modality of choice for lipoma and is indicated for any deep mass or subcutaneous lesion >5 cm.[7] The characteristic appearance of lipoma on MRI excludes the need for biopsy from the lesion before treatment.[1]
Bursae are small fluid-filled sac lined by the synovial membrane, and their primary function is to reduce friction and provide a cushion between muscles and bones. They are susceptible to inflammation due to acute and repetitive trauma or by infection. Olecranon bursa is located between the olecranon and overlying skin, which allows the elbow to bend and straighten freely underneath the skin.[4] Chronic olecranon bursitis may present as a hypointense collection on T1W with variable signal intensity in T2W sequences. Further, it also shows enhancement of bursa margin. However, it is a clinical diagnosis, and MRI is rarely performed.[7] Lipoma arborescens is the other fat-containing lesion that is more commonly seen to involve the synovium. There is a complete replacement of bursa by mature fat cells with the villous proliferation of the synovial membrane, which appears as frond-like outgrowths.[4] In lipoma arborescens, the subsynovial fatty tissue proliferates in three morphological forms,[8] out of which nodular form can mimic bursal lipoma. However, it appears as fatty infiltration into the synovium, while our lesion was held through a pedicel to the synovium. The most common site of both intra-articular true lipoma and lipoma arborescens is the knee joint. In the knee joint, the lipomas have been seen to involve Hoffa’s fat pad, suprapatellar pouch, and the posterior compartment of the knee.[5] Other sites of lipoma in a bursa that has been reported so far are subacromialsubdeltoid bursa [6] and superficial infrapatellar bursa.[3] The case being reported by us is the only other report of a lipoma in the olecranon bursa. It appeared as a solid echogenic mass on ultrasound and had typical features of a lipoma on MRI.
Nodal causes for the swelling involve the medial aspect of the elbow and include cat scratch disease, tubercular lymphadenitis, and lymphoma. The lymphadenitis associated with cat scratch disease is often confused with neoplasm. The stage of disease infection can be identified by enhancement patterns as (1) homogeneous, moderate enhancement on MRI scan in early stage, (2) heterogeneous enhancement with progressively “spoke wheel-like” enhancement of the central patchy low-density area on CT scan in intermediate stage, and (3) astral low density/hypointensity areas with marked enhancement or the “rose-flower sign” on CT/MRI in late stages of infection.[9]
Another rare tumor that has been reported in the region of olecranon bursa is the glomus tumor. This lesion was excised following radiographs, and a diagnosis was made on histopathology.[9]
CONCLUSION
This case report aims to present the imaging appearance of a common tumor in a rare location. These can be confusing for the diagnosticians, especially when they are small.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Lipomatous soft-tissue tumors. J Am Acad Orthop Surg. 2018;26:779-88.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-articular lipoma of the knee joint located in the posterior compartment: A rare location. North Clin Istanb. 2016;4:89-92.
- [CrossRef] [Google Scholar]
- Lipoma in the superficial infrapatellar bursa. Eur J Dermatol. 2011;21:97-8.
- [CrossRef] [PubMed] [Google Scholar]
- A case of lipoma in olecranon bursa. Cent Japan J Orthop Surg Traumatol. 2004;47:1273-4.
- [Google Scholar]
- IntraArticular synovial lipoma of the right tarsometatarsal joint-a rare case report. J Clin Diagn Res. 2014;8:FD03-4.
- [Google Scholar]
- Lipoma of the subdeltoid bursa of the shoulder joint: A case report. Orthop Traumatol. 2012;61:608-11.
- [CrossRef] [Google Scholar]
- Diagnosis and management of soft tissue masses. J Am Acad Orthop Surg. 2014;22:742-50.
- [CrossRef] [PubMed] [Google Scholar]
- Large intra-articular true lipoma of the knee. BMC Musculoskelet Disord. 2019;20:110.
- [CrossRef] [PubMed] [Google Scholar]
- Glomus tumour of the elbow: A case of mistaken identity. Shoulder Elbow. 2014;6:134-6.
- [CrossRef] [PubMed] [Google Scholar]






