Translate this page into:
MRI evaluation of predisposing factors in patellar instability

*Corresponding author: Vijinder Arora, Professor and Head, Department of Radiodiagnosis and Imaging, Sri Guru Ram Das Institute of Medical Sciences and Research, Sri Amritsar, Punjab, India. drvijinderarora338@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arora V, Kakkar A. MRI evaluation of predisposing factors in patellar instability. Indian J Musculoskelet Radiol 2021;3:75-81.
Abstract
Objectives:
In this study, we have attempted to evaluate the predisposing factors of patellar instability on magnetic resonance imaging (MRI) and to compare the significance of measurement at the level of trochlear bone versus cartilage for trochlear dysplasia.
Material and Methods:
Thirty patients of patellar instability were assessed on MRI for risk factors of patellar instability including trochlear dysplasia, tibial tuberosity to trochlear groove (TT-TG) distance, and patellar height ratio.
Results:
Twenty-one (70%) and 27 (90%) cases were positive for decreased trochlear depth when measured at the level of trochlear bone and cartilage, respectively. Eighteen (60%) and 25 (83.33%) cases were positive for trochlear facet asymmetry when measured at trochlear bone and cartilage, respectively. Twelve cases (40 %) were positive for patella alta. Ten cases (33.33%) were positive for decreased lateral trochlear inclination. Seven cases (23.3%) had increased TT to TG distance. Twenty-four cases (80%) were of age equal to or <25 years.
Conclusion:
According to our study, trochlear dysplasia is the most common predisposing factor of patellar instability (100%) followed by patella alta (40%) and TT-TG distance (23.3%). Trochlear depth and facet asymmetry produce better results as a predisposing factor for instability of patella when measured at the level of trochlear cartilage as compared to trochlear bone with P = 0.001.
Keywords
Intraosseous
Schwannoma
Pubic bone
Lytic lesion
Trucut biopsy
INTRODUCTION
Patellar instability is a condition in which patella is unable to contain itself in the femoral trochlea during normal movement of knee joint. Patellar instability is common in young adults involved in sports related activities with a female preponderance.[1,2] Lewallen et al. reported that with every 1-year increase in age, the recurrent dislocation risk is decreased by 8% and after the age of 40 years, there were no recurrences.[3,4] Mostly lateral patellar dislocations (LPDs) are transient in nature with very few cases presenting with fixed lateral dislocation.[2] Therefore, the term transient LPD or patellar instability is considered to be more appropriate. Its prevalence is about 6–77 patients/1 lac individuals.[1,2,5]
Femoral trochlea and patella articulate to form the patellofemoral joint. Lateral dislocation of patella is common due to the divergent pull of the patellar tendons and quadriceps, which is further aggravated by the normal rest state valgus configuration of knee.[5-9] The lateral trochlea must be high enough and the femoral sulcus must be deep enough to provide safe movement of patella along patellofemoral joint. Lateral dislocation of patella is prevented by various medial stabilizers, among which most important role is played by medial patellar retinaculum/medial patellofemoral ligament (MR/MPFL). When the knee joint is in full extension, there is no articulation of patella and femoral trochlea, rather it lies superolateral to the uppermost trochlea. With flexion at knee joint, patella articulates with trochlea at approximate 10° of flexion.[10-13]
Patients often complain of anteromedial knee pain which is attributed to MR/MPFL injury and osseous/chondral injury (involving medial aspect of patella and lateral aspect of femoral condyle).
The injury mostly occurs due to twisting of knee when knee is in mild flexion (<30°) which leads to injury of medial stabilizers and medial aspect of patella strikes against lateral femoral condyle. Damage to medial stabilizers leads to recurrent patellar dislocation, especially if there are additional anatomical risk factors such as lateralization of the tibial tuberosity, trochlear dysplasia, and patella alta.
Magnetic resonance imaging (MRI) plays a key role in recognition of these anatomical risk factors associated with patellar instability, thereby guiding for subsequent treatment. Patients with absence of these anatomical risk factors and mild grade damage to medial stabilizers can be treated conservatively without any need for surgical intervention. On the other hand, the patient with severe damage to medial stabilizers with presence of these anatomical risk factors can be treated surgically.
The role of this study was to recognize the predisposing factors of patellar instability on MRI. Various MRI predisposing factors for patellar instability include lateralization of tibial tuberosity (which is recognized by increased tibial tubercle-trochlear groove [TT-TG] distance), trochlear dysplasia (which is recognized by decreased trochlear depth, increased lateral trochlear inclination, and trochlear facet asymmetry), and patella alta (which is recognized by increased patellar height ratio).[11,12] Through this study, we have also tried to compare the significance of measurement at the level of trochlear bone versus cartilage for trochlear facet asymmetry and trochlear depth using Student’s t-test.
MATERIAL AND METHODS
Thirty patients with clinical suspicion and MRI findings of patellar instability were enrolled in this single institutional observational study. This study received clearance from the Ethics Review Committee.
All patients underwent MRI examination on Philips Achieva dstream 1.5 Tesla MRI using Sense Body Coil. Various sequences used in our study included T1-weighted Turbo spin echo sagittal, fat-suppressed proton-density sagittal and axial (FSPD SAG and AXIAL), and gradient-echo fast-field echo coronal. Additional MRI sequences were used whenever required.
All patients were assessed for various risk factors for patellar instability including trochlear facet asymmetry (at the level of trochlear bone and trochlear cartilage), trochlear depth (at the level of trochlear bone and trochlear cartilage), lateral trochlear inclination, patellar height ratio, and TTTG distance. Normal and cutoff values for the same are depicted in Table 1. As we move distally, the TG deepens, so the chances of patellar dislocation are less likely in distal trochlea. Therefore, all trochlear measurements for diagnosis of patellar instability were made at the level of proximal trochlea. The superior most transverse image showing trochlear cartilage was used to measure all the parameters for trochlear dysplasia [Figure 1]. Two radiologists (one senior radiologist with 20 years of experience in MRI and other in training with 3 years of experience) independently evaluated all the cases in this study.
| Factor | Normal value | Cutoff value |
|---|---|---|
| Trochlear depth | >3 mm | <3 mm |
| Trochlear facet ratio | >40% | <40% |
| Patellar height ratio | <1.3 | >1.3 |
| Lateral trochlear inclination | >11° | <11° |
| TT-TG distance | <20 mm | >20 mm |
MRI: Magnetic resonance imaging, TT-TG: Tibial tubercle-trochlear groove

- To demonstrate the desired level for measurement of various parameters of patellar instability. (a) Superior most axial image showing trochlear cartilage (arrow) was carefully chosen from the dataset. (b) and (c) Level of the selected axial image on corresponding coronal and sagittal planes.
Trochlear dysplasia
The following parameters were used to evaluate trochlear dysplasia:
Lateral trochlear inclination
To calculate lateral trochlear inclination two lines were drawn, one along the subchondral bone of lateral trochlear facet and other along the posterior aspect of condyles of femur. The angle between these two lines is the lateral trochlear inclination. The cutoff for trochlear dysplasia was an inclination angle of <11° [Figure 2].[14]
- Lateral trochlear inclination measured on axial fat-suppressed proton-density MR images. (a) Normal trochlea with inclination of 38°. (b) Trochlear dysplasia with inclination angle of 8°.
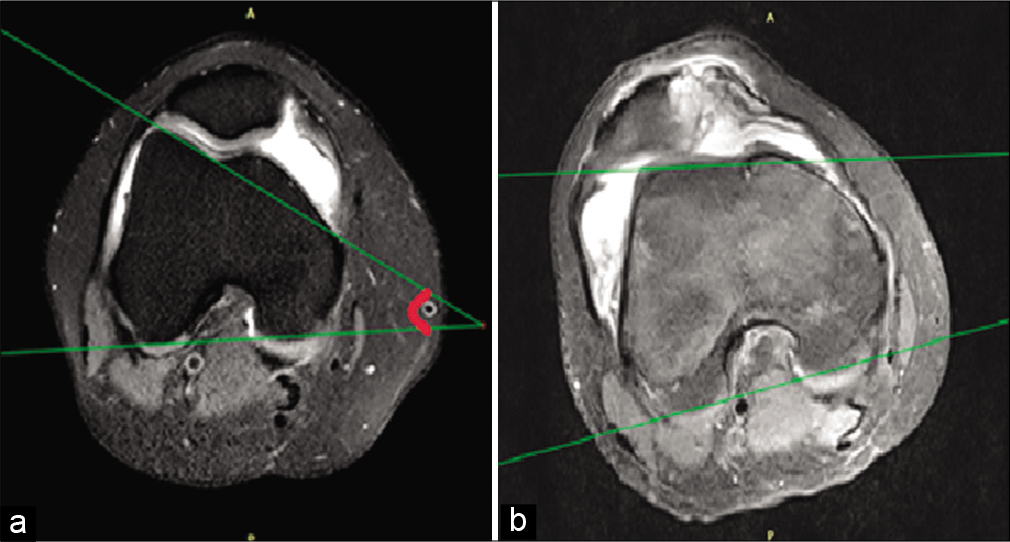
Trochlear facet asymmetry
To calculate trochlear facet ratio, length of the medial and lateral trochlear facets was measured. The ratio of medial to lateral trochlear facet was given as trochlear facet ratio and was measured both at the level of trochlear bone and cartilage. Trochlear facet asymmetry was characterized by a ratio which measured <40% and it indicated dysplasia [Figures 3 and 4].[15]

- Trochlear facet asymmetry measured at the level of trochlear bone on axial fat-suppressed proton-density MR images as A/B ×100. (a) Normal trochlea with a facet ratio of 55%. (b) Trochlear dysplasia with a face ratio of 32%.
- Trochlear facet asymmetry measured at the level of trochlear cartilage on axial fat-suppressed proton-density MR images as A/B ×100. (a) Normal trochlea with a facet ratio of 49%. (b) Trochlear dysplasia with a facet ratio of 31%.
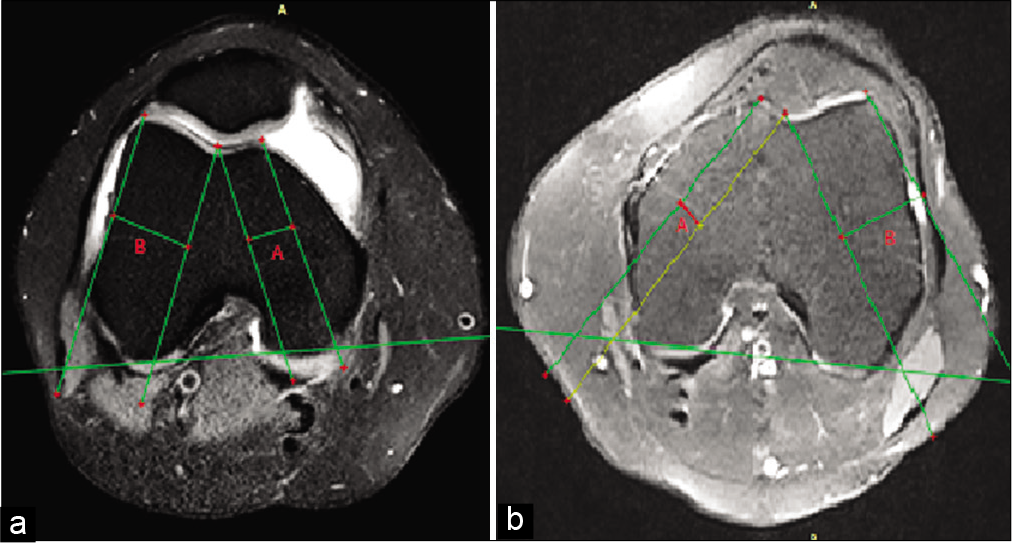
Trochlear depth
A line was drawn along the posterior plane of femoral condyle. Three lines were drawn perpendicular to the aforementioned line. These three lines were drawn such that they depict maximum anteroposterior distance of medial and lateral trochlear facets (Line C and A) and the deepest sulcal point (Line B). Trochlear depth was measured using the following equation: (A+C)/2–B. This value was measured both at the level of subchondral bone and trochlear cartilage. Trochlear dysplasia was diagnosed if trochlear depth was less than or equal to 3.0 mm [Figures 5 and 6].[15]
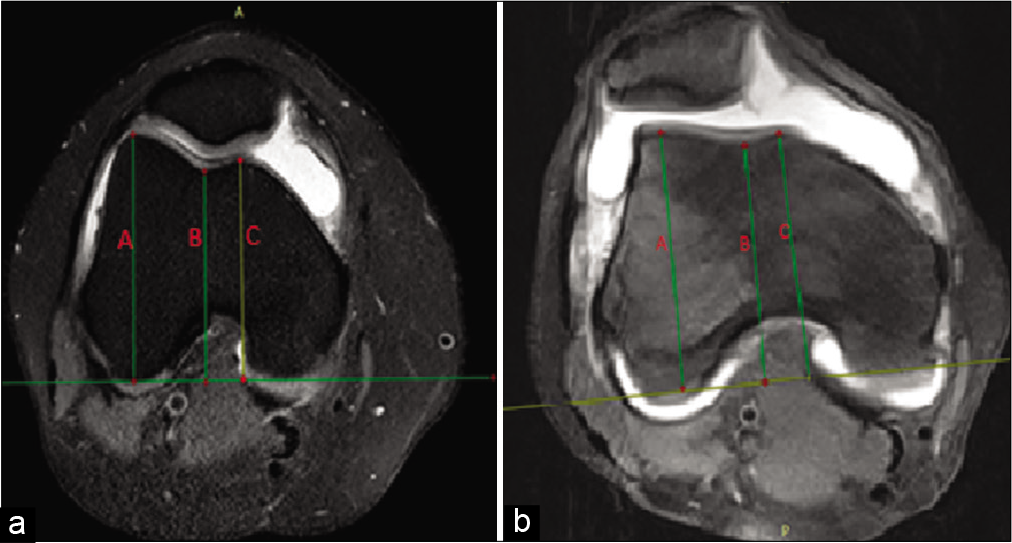
- Trochlear depth measured at the level of trochlear bone on axial fat-suppressed proton-density images as (A+B)/2–C. (a) Normal trochlea with a depth 5.5 mm. (b) Trochlear dysplasia with a trochlear depth of 2.8 mm.

- Trochlear depth measured at the level of trochlear cartilage on axial fat-suppressed proton-density MR images as (A+B)/2–C. (a) Normal trochlea with a depth 4.9 mm. (b) Trochlear dysplasia with a trochlear depth of 2.5 mm.
TT-TG distance
It was measured as a maximum distance from the midpoint of tibial tubercle to the deepest point of trochlea. Here, a line was drawn perpendicular to the posterior plane of femoral condyles such that it depicted deepest sulcal point. This line was copied into the transverse section showing tibial tubercle. Another line from the midpoint of tibial tubercle was drawn parallel to the aforementioned line. The distance between two lines was given as TT-TG distance. A value of more than 20 mm was taken as a cutoff and indicated marked lateralization of the tuberosity [Figure 7].[16]

- TT-TG distance measured between line 1 and line 2 on axial FSPD images depicted by line A. (Line 1 drawn from the middle of the tibial tubercle and Line 2 extrapolated from the deepest part of the trochlea using posterior plane of condyle as reference line). (a) Normal TT-TG distance of 11 mm. (b) Increased TT-TG distance of 22 mm. TT-TG: Tibial tubercle-trochlear groove, FSPD: Fat-suppressed proton density
Patellar height ratio
Patellar height ratio was evaluated on sagittal sections of knee MRI as a ratio between patellar tendon length and longest craniocaudal diameter of patella (Insall-Salvati ratio). A ratio measuring more than 1.30 indicated patella alta [Figure 8].[10]

- Patellar height ratio measured on sagittal T1-weighted turbo spin-echo MR images as B/A. (a) Normal patellar height ratio of 1.1. (b) Increased patellar height ratio of 1.5.
Statistical method
The statistical evaluation was done using Student’s t-test and SPSS version 24.
Study design
This was an observational, cross-sectional study.
Statistical analysis
SPSS version 24 and Student’s t-test.
RESULTS
Twenty-one (70%) and 27 (90%) out of 30 cases were positive for decreased trochlear depth when measured at the level of trochlear bone and cartilage, respectively.
Eighteen (60%) and 25 (83.33%) out of 30 cases were positive for trochlear facet asymmetry when measured at the level of trochlear bone and cartilage, respectively.
Twelve cases (40 %) were positive for patella alta.
Ten cases (33.33%) were positive for decreased lateral trochlear inclination.
Seven cases (23.3 %) had increased TT-TG distance [Table 2 and Graph 1].
| Factor | Positive cases | Total cases | Percentage |
|---|---|---|---|
| Trochlear dysplasia | 30 | 30 | 100 |
| Trochlear depth at cartilage level | 27 | 30 | 90 |
| Trochlear facet asymmetry at cartilage level | 25 | 30 | 83.33 |
| Trochlear depth at bone level | 21 | 30 | 70 |
| Trochlear facet asymmetry at bone level | 18 | 30 | 60 |
| Patella alta | 12 | 30 | 40 |
| Lateral trochlear inclination | 10 | 30 | 33.33 |
| TT-TG distance | 07 | 30 | 23.33 |
MRI: Magnetic resonance imaging, TT-TG: Tibial tubercle-trochlear groove

- Prevalence of various predisposing factors in patellar instability on MRI.
Twenty-eight (93.7%) out of 30 cases showed more than 1 risk factors (multifactorial) for patellar instability, out of which 12 patients (40%) had two risk factors, 9 patients (30%) had three risk factors, 5 patients (16.6%) had four risk factors, and 2 patients (6.7%) had all the five risk factors [Table 3].
| Number of MRI risk factors present | Number of patients | Total cases | Percentage |
|---|---|---|---|
| 5 | 2 | 30 | 6.7 |
| 4 | 5 | 30 | 16.6 |
| 3 | 9 | 30 | 30 |
| 2 | 12 | 30 | 40 |
| 1 | 2 | 30 | 6.7 |
MRI: Magnetic resonance imaging
Twenty-four (80%) out of 30 cases were of age equal to or <25 years and only 4 (13.3%) out of 12 cases were of age more than 30 years.
Seventeen (56.7%) out of 30 cases were female and 13 (43.7%) were male.
Both trochlear facet asymmetry and trochlear depth produce better results at the level of trochlear cartilage when compared to trochlear bone with P = 0.001 [Table 4 and Graph 2].
| S. No. | Factor | Number of cases | Bone | Cartilage | P value | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| 1. | Trochlear depth (in mm) | 30 | 2.942 | 1.096 | 2.127 | 0.932 | 0.001 |
| 2. | Trochlear facet asymmetry (M/L×100) | 30 | 42.587 | 11.480 | 36.273 | 7.860 | 0.001 |

- Comparison of mean values of trochlear facet asymmetry and trochlear depth at the level of trochlear bone and trochlear cartilage.
DISCUSSION
Instability of patellofemoral joint is associated with the presence of various anatomic predisposing factors. MRI plays an important role to identify various risk factors for patellar instability which includes trochlear dysplasia, high-riding patella (patella alta), and abnormal TT-TG distance.
In this study, we have used three different parameters to assess trochlear dysplasia, namely, trochlear depth, lateral trochlear inclination, and trochlear facet ratio. Carrillon et al.[14] and Diederichs et al.[10] also described the use of these three parameters in the assessment of trochlear dysplasia with excellent values in discriminating cases and controls.
In trochlear dysplasia, there is diminished engagement between femoral trochlea and patella due to a shallow TG, thereby leading to patellar instability.[13] Twenty-one (70%) and 27 (90%) out of our 30 cases were positive for decreased trochlear depth when measured at the level of trochlear bone and cartilage, respectively, while 18 (60%) and 27 (83.33%) out of 30 cases were positive for trochlear facet asymmetry when measured at the level of trochlear bone and cartilage, respectively. This corresponds to the study done by Pfirrmann et al.[15] where a specificity and sensitivity of 96% and 100%, respectively, were established for both trochlear facet asymmetry and trochlear depth as a diagnostic tool for patellar instability.
Trochlear depth and trochlear facet asymmetry were measured both at the level of trochlear cartilage (in accordance with Escala et al.[17]) and at the level of trochlear bone (in accordance with Diederichs et al.[10] and Pfirrmann et al.[15]). In our study, we found that both these factors show statistically significant improvement in results when measured along trochlear cartilage as compared to trochlear bone (P = 0.001).
Ten cases (33.33%) were positive for decreased lateral trochlear inclination. This is in discordance with the study done by Carrillon et al.[14] where they proved that lateral trochlear inclination has a sensitivity and specificity of 93% and 87%, respectively, as a diagnostic tool for patellar instability.
Increased TT-TG pertains to laterally placed TT in relation to TG which leads to increased lateral pull of patellar tendon over patella leading to increased risk of lateral dislocation. Camp et al.[18] in their study showed that TT-TG distance was increased in 56–93% of patients suffering from patellar instability. However, only 7 cases (23.3 %) were positive for increased TT-TG distance in our study.
In cases of high-riding patella (patella alta), contact between the femoral trochlea and patella is reduced during early phase of knee flexion which leads to patellar dislocation.13Patellar height can be evaluated using different parameters. We used Insall-Salvati ratio to measure patella alta with a cutoff of more than 1.3. Twelve out of 30 cases (40 %) were positive for patella alta in our study. Escala et al.[17] used Insall-Salvati ratio with a cutoff of more than 1.2 to diagnose patella alta in patient with patellar instability and found a sensitivity of 79% and specificity of 67.6%. The smaller number of cases in our study could be attributed to higher cutoff used in our study. In one of the study, patella alta was present in 36% of subjects in control group, therefore, patella alta holds higher utility as a risk factor in patellar instability when it is present along with other risk factors such as increased TT-TG distance and dysplastic trochlea.
Askenberger et al. evaluated 103 patients with age <14 years for dysplastic trochlea, TT to TG distance, patellar tilt, and patella alta on MRI. It was found that 79% of patients with LPD had at least two out of four above-mentioned risk factors of patellar instability, in comparison to only 7% of patients in the control group. This corresponds to our study in which 93.3% had at least two of the five risk factors of patellar instability.[19]
First episode of dislocation at a younger age group has constantly been recognized as a major risk factor for recurrent LPD in majority of studies. Balcarek et al.[20] in their study established a statistically significant odds ratio for recurrence of patellar dislocation, when the first episode of dislocation was at an age <16 years in comparison to a later onset of the first episode.[15] According to Fithian et al., maximum cases of recurrent LPD were found in the age group of 10–17 years with females more commonly affected than males. In their study, they also calculated median age for the first episode and recurrence of patellar dislocation as 16 years and 21 years, respectively.[1] This partly goes with our study considering the fact that in our study, 80% of cases were up to 25 years of age. Furthermore, in our study, female patients predominated (56.7%) over male (43.3%), which clearly corresponds to available literature. Fithian et al.[1] also described a very low incidence of patellar instability in more than 30 years of age. This also corresponds to our study with only 4 out of 30 cases (13.3%) of age more than 30 years.
CONCLUSION
We would like to conclude that MRI is a good modality for the evaluation of patellar instability.
According to our study, trochlear depth and facet asymmetry produce better results as a predisposing factor for instability of patella when measured at the level of trochlear cartilage as compared to trochlear bone.
Our results highlight that the most critical factor responsible for patellar instability is trochlear dysplasia. Out of three parameters that define trochlear dysplasia, shallow trochlear depth was found to be strongest determinant responsible for patellar instability followed by trochlear facet asymmetry and lateral trochlear inclination. Patellar height ratio and TT-TG showed relatively less contribution for unstable patella.
Prevalence of patellar instability is higher in younger population, more frequently involving age equal to or <25 years. Patellar instability is more prevalent in females than males.
All radiologists must keep in mind all the risk factors for patellar instability measurable on MRI and should document them in their reports so that the appropriate treatment can be selected. A systematic radiological approach should be followed for the patient, right from the selection of the highest transverse section showing trochlear cartilage for the evaluation of various risk factors to the corrective placement of calipers for measuring parameters.
A major strength of our study was measuring trochlear facet asymmetry and trochlear depth both at the level of trochlear bone and trochlear cartilage and comparing their results, since it has always been a matter of conflict whether to use trochlear bone or cartilage for these measurements. Another strength of our study was the criteria used for deciding the level at which various measurements for diagnosis of patellar instability were performed. Unlike study conducted by Pfirrmann et al.[15] in which all these parameters were measured at a particular distance from the joint line, we decided the level of measurement by choosing the superior most axial section showing trochlear cartilage. The disadvantage of choosing a fixed distance from joint line is that it does not consider into account the variation of height among study group.
Limitations
A major limitation of our study was a small sample size of only 30 patients. Another limitation was lack of controls in our study. A larger sample size with a control group would definitely be more validating.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114-21.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40:606-11.
- [CrossRef] [PubMed] [Google Scholar]
- First-time patellofemoral dislocation: Risk factors for recurrent instability. J Knee Surg. 2015;28:303-9.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41:575-81.
- [CrossRef] [PubMed] [Google Scholar]
- Transient lateral patellar dislocation: Review of imaging findings, patellofemoral anatomy, and treatment options. Emerg Radiol. 2013;20:11-23.
- [CrossRef] [PubMed] [Google Scholar]
- Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34:385-96.
- [CrossRef] [Google Scholar]
- Imaging of patellofemoral disorders. Clin Radiol. 2004;59:543-57.
- [CrossRef] [PubMed] [Google Scholar]
- Acute knee dislocation: Review of an elusive entity. Curr Probl Diagn Radiol. 2009;38:237-50.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of patellar instability: Injury patterns and assessment of risk factors. Radiographics. 2010;30:961-81.
- [CrossRef] [PubMed] [Google Scholar]
- Acute lateral patellar dislocation at MR imaging: Injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736-43.
- [CrossRef] [PubMed] [Google Scholar]
- Modern management of patellar instability. Int Orthop. 2012;36:2447-56.
- [CrossRef] [PubMed] [Google Scholar]
- Disorders of the Patellofemoral Joint (4th ed). Philadelphia, PA: Lippincott, Williams, and Wilkins; 2004.
- [Google Scholar]
- Patellar instability: Assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216:582-5.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858-64.
- [CrossRef] [PubMed] [Google Scholar]
- Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26.
- [CrossRef] [PubMed] [Google Scholar]
- Knee Surg Sports Traumatol Arthrosc. 2006;14:264-72.
- [CrossRef] [PubMed] [Google Scholar]
- CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41:1835-40.
- [CrossRef] [PubMed] [Google Scholar]
- Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: A prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med. 2017;45:50-8.
- [CrossRef] [PubMed] [Google Scholar]
- Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc. 2014;22:2308-14.
- [CrossRef] [PubMed] [Google Scholar]






