Translate this page into:
Multiossicle accessory navicular bones – A symptomatic presentation of rare variant anatomy

*Corresponding author: Pushpa Bhari Thippeswamy, Department of Radiology, Ganga Medical Center and Hospital, Coimbatore, Tamil Nadu, India. docpushpa@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shyam K, Bhari Thippeswamy P, D’Souza TD, Sundararajan SR. Multiossicle accessory navicular bones – A symptomatic presentation of rare variant anatomy. Indian J Musculoskelet Radiol 2023;5:40-3.
Abstract
The foot and ankle are common sites for variant anatomy, of which a known symptomatic entity is the accessory navicular bone. These accessory ossicles may have a varied appearance based on their relationship to the parent navicular and are usually solitary and bilateral. However, a rare multi-ossicle variant is also described, which may lead to an erroneous diagnosis of navicular avulsion fracture with fragmentation in the setting of an ankle injury. We describe such a case of the incidental multi-ossicle accessory navicular bone, which proved a diagnostic confounder in a lady with a history of an ankle injury.
Keywords
The accessory navicular bone
Tibialis posterior tendinitis
Multi-ossicle accessory navicular bone
Medial foot pain
Type 2 accessory navicular
INTRODUCTION
The accessory navicular (AN) bone is a commonly encountered anatomic variant of the foot, often leading to complaints of medial foot pain. Classification of AN is done based on its relationship to the parent navicular bone, and radiographic appearances are typical. However, a rare multi-ossicle variant is also described, which may lead to an erroneous diagnosis of a fragmented navicular avulsion fracture, especially with an antecedent history of an ankle injury. We describe one such case of the incidental multi-ossicle accessory navicular bone, which proved a diagnostic confounder in a lady with a history of an ankle injury.
CASE REPORT
A 53-year-old lady presented to the outpatient clinic with complaints of intermittent pain and swelling over the medial aspect of her right foot for a 1-year duration. She provided a history of having fallen on her right foot twice in the past year, most recently 2 months before the presentation. No significant injury was reported at the time and medical attention was not sought. On examination, tenderness was elicited around the medial malleolus along the course of the tibialis posterior tendon (posterior tibial tendon, i.e., PTT). The medial plantar arch was lost, with mild soft-tissue swelling anterior to the medial malleolus. No significant restriction of motion was seen. Laboratory parameters showed an elevated C-reactive protein and erythrocyte sedimentation rate. An oblique radiograph of the foot was taken, which revealed two well-defined and circumferentially corticated osseous structures medial to the navicular bone, with no gross fracture [Figure 1]. Clinical suspicion of PTT tendinitis with pes planus was raised. A magnetic resonance imaging (MRI) was performed, which showed thickening and edema of the PTT with surrounding soft-tissue edema [Figure 2a and b]. Two well-defined ossicles, one of which was sclerotic, were noted within the substance of the tibialis posterior tendon, just proximal to its attachment to the navicular bone [Figure 3a and b]. Synchondrosis was seen between the laterally placed ossicle and navicular bone. The spring ligament was normal. Ultrasound revealed thickened, heterogeneous PTT with peritendinous fluid, and also confirmed the intratendinous location of the ossicles seen on radiograph and MRI [Figure 4a and b]. A diagnosis of multiple accessory navicular bones with PTT tendinitis was made and was managed with anti-inflammatory medication, physiotherapy, and medial arch-supportive footwear.

- Radiograph of right foot with 45° external oblique projection showing two well-corticated osseous densities posteromedial to the navicular bone. No gross navicular fracture or defect is seen.

- (a and b) Axial proton density fat saturated (a) and T1W (b) Images show the sclerotic ossicle in question (white arrow) within the tibialis posterior tendon, which is thickened and displays an altered signal, suggestive of tendinosis.

- (a and b) Sagittal T2W images of right foot show the ossicles just posteromedial to the navicular, both being embedded within the tibialis posterior tendon (blue arrow). The ossicle (white arrow in a) appears sclerotic, which may be a post-traumatic sequel.
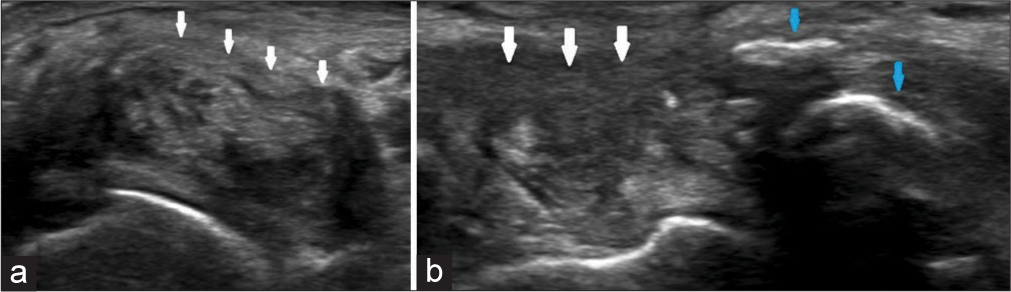
- Transverse (a) and longitudinal (b) ultrasound images of the tibialis posterior tendon, which is thickened and heterogeneous, consistent with tendinosis (white arrows). Also seen are the ossicles, as dense intratendinous structures with acoustic shadowing (blue arrows).
DISCUSSION
The foot and ankle are sites of frequent variant anatomy, of which the most commonly seen relate to accessory ossicles or sesamoid bones. The most common accessory ossicles are the os trigonum (present posterior to the talus), the os naviculare (posteromedial to navicular bone), and the os intermetatarsum (commonly at the bases of first and second metatarsals).[1] Usually being asymptomatic and discovered incidentally, they may occasionally produce symptoms or may act as a red herring on diagnostic imaging. Hence, awareness of these anatomic variations helps in accurate clinical evaluation.
Of particular interest here is the AN, also known as os tibiale, os tibiale externum, prehallux, or naviculare secundarium, which results from the failure of fusion of the secondary ossification center of the navicular. Miller estimated the prevalence of AN to be 4–21%.[2] The AN is present adjacent to the posteromedial tubercle of the navicular. Depending on the type of articulation shared with the parent bone, they may be of three types. Type I AN is a small and rounded ossified structure within the substance of the tibialis posterior tendon, with no navicular articulation, and has an incidence of 30%.[3] Type II AN, the most common variant (incidence of 50%), is typically triangular or hemispherical and shows a thin synchondrosis with the navicular bone. These may eventually fuse with the parent bone. Type III (incidence of 30%) is a prominent navicular tuberosity and is considered a fused version of Type II; also referred to as a “cornuate navicular” due to its shape.[1] Type II AN most commonly produces symptoms, and this is attributed to altered biomechanics,[4] stretching of the tendon[5], or shearing movement across the synchondrosis.[6] The result may be disruption of synchondrosis, ossicular osteonecrosis, or pes planus due to chronic PTT tendinosis or tear.[1] Tears of the PTT are of three types: Type I is intrasubstance partial-thickness tears, Type II tears show tendon attenuation, and Type III is complete tears with the segmental absence of tendon and fluid gap. A history of trauma, present in 74% of cases of symptomatic AN in athletes, is a possible catalyst in producing symptoms with an otherwise occult AN.[6]
Type II AN may be bilateral in up to 50–90% of cases.[7] Although they are commonly solitary, a multiossicle appearance has been described by Perdikakis et al.,[3] whose study established a prevalence of 14.7%, of which nearly 60% were the 2-ossicle variant and the rest, the 3-ossicle variant. Seen only in mature skeletons, the multi-ossicle variant may arise due to repetitive microtrauma to the navicular ossification center, which leads to osteochondritis, fragmentation, and ossification.[3]
Clinical presentation is typical with pain over the medial aspect of the foot, with associated tenderness and an inability to single-heel lift. Radiography in the 45° external oblique projection demonstrates a loss of the medial plantar arch and the presence of ossicle(s) medial to the navicular. Associated soft-tissue changes can be seen on ultrasound. This includes the presence of the ossicle within the substance of the PTT, tendon heterogeneity and peritendinous fluid (representing tendinitis), and disruption of the synchondrosis.[8] MRI shows the presence of ossicles and associated tendinous changes. The presence of osteonecrosis or synchondral disruption may be demonstrated as edema within the ossicle. In addition, chronic tears of the PTT may also lead to injuries of the spring ligament in 74–92% of individuals.[7] Our patient presented with pain and swelling over the medial aspect of her foot. Clinical suspicion of PTT tendinitis was raised. Radiograph showed osseous densities with regular borders adjacent to the navicular bone, and these were confirmed to be intratendinous in location and coexist with tendinitis on MRI and ultrasound.
Differential diagnoses include avulsion fracture of the navicular and calcific tendinitis of the PTT. Prior history of injury with an irregular fragment of separated bone suggests an avulsion fracture. Furthermore, if in doubt, radiography of both feet may be obtained, as AN tends to be bilateral.[7] Due to an eversion mechanism, the avulsion of AN may also be associated with cuboid impaction fracture.[9] Tendinous attachment to an avulsed fragment may be appreciated on ultrasound. Calcific tendinitis of the PTT may have a similar clinical presentation, though rare. Acute presentations of calcific tendinitis may show amorphous, fluffy calcifications adjacent to the medial malleolus (in contrast to defined borders of AN). Chronic presentations show linear, so-called comet tail patterns of tendinous calcification at the tendon insertion site. Ultrasound shows a heterogeneous tendon with peritiendinous fluid and calcification which may or may not cause acoustic shadowing.
In our instance, with the background of a remote history of trauma, a diagnostic dilemma between chronic sequel of a navicular avulsion fracture, primary calcific tendinitis of PTT, or accessory navicular bones were encountered. Due to the rarity of primary calcific tendinitis of PTT and the well-defined, rounded appearance, and intratendinous location of the calcified bodies, the possibility of the former two conditions was deemed less likely. However, the present imaging appearance may still be attributed to post-traumatic fragmentation of an initially singular ossicle which, over time, has resulted in tendinitis. Examination of prior imaging (unavailable in our instance) may help with this distinction.
Treatment is aimed at pain relief and restoration of the medial plantar arch. In a majority of cases, conservative management through anti-inflammatory medication, rest, cast application, or supportive footwear is sufficient,[10] the latter being done in our instance. Once an acute avulsion fracture is ruled out, pain relief may be attained through local injection of corticosteroid. In refractory cases, surgical management may be done through the removal of the offending ossicles and reattachment of the tibialis posterior to the navicular. Recalcitrant pain due to AN or widening of synchondrosis may be treated through the surgical fusion of the ossicle to the parent bone, provided that the fracture fragment is large enough to afford adequate purchase by screws.[3]
CONCLUSION
Medial ankle and foot pain may be attributed to painful syndromes secondary to anatomic variants such as an accessory navicular bone, or a navicular avulsion fracture in the setting of acute injury. An unusual multipartite appearance of the navicular bone is a rare entity and a lack of awareness of the same may lead to the misdiagnosis of this incidental finding as an avulsion fracture and lead to inappropriate management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Anatomical variation in the ankle and foot: From incidental finding to inductor of pathology. Part II: Midfoot and forefoot. Insights Imaging. 2019;10:69.
- [CrossRef] [PubMed] [Google Scholar]
- Painful accessory bones of the foot. Semin Musculoskelet Radiol. 2002;6:153-61.
- [CrossRef] [PubMed] [Google Scholar]
- Os naviculare: The multi-ossicle configuration of a normal variant. Skeletal Radiol. 2011;40:85-8.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging and CT in the assessment of osseous abnormalities of the ankle and foot. Magn Reson Imaging Clin N Am. 2001;9:567-78. xi
- [CrossRef] [PubMed] [Google Scholar]
- Accessory navicular syndrome in athlete vs general population. Foot Ankle Int. 2016;37:862-7.
- [CrossRef] [PubMed] [Google Scholar]
- The painful accessory navicular. Skeletal Radiol. 1984;12:250-62.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical use of high-resolution ultrasonography for the diagnosis of Type II accessory navicular bone. Am J Phys Med Rehabil. 2012;91:177-81.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures and dislocations of the foot. Semin Roentgenol. 1994;29:152-75.
- [CrossRef] [PubMed] [Google Scholar]
- Mann’s Surgery of the Foot and Ankle: Expert Consult-Online Philadelphia, PA: Elsevier Health Sciences; 2013.
- [Google Scholar]







