Translate this page into:
Osteopetrosis: A rare disease with unusual presentation as non-neutropenic typhlitis

*Corresponding author: Rashmeet Kaur, Department of Radiodiagnosis, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India. dr.rashmeet@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur R, Dahuja A, Tapasvi C, Kaur S. Osteopetrosis: A rare disease with unusual presentation as nonneutropenic typhlitis. Indian J Musculoskelet Radiol 2023;5:68-71.
Abstract
Osteopetrosis is a rare inherited disorder characterized by the inability to reabsorb and remodel bone due to osteoclast dysfunction. There is a resultant increased bone mass and density with skeletal malformation and bone marrow failure, which may be fatal. There is extramedullary hematopoiesis, which causes hepatosplenomegaly and anemia. In our case, the presentation of typhlitis in osteopetrosis proved to be life-threatening, and hence, the early diagnosis of osteopetrosis will help to improve the management and quality of life of the patient.
Keywords
Non-neutropenic
Osteopetrosis
Typhlitis
INTRODUCTION
Osteopetrosis has been referred to as marble bone disease and is a rare inherited sclerosing bone dysplasia that was first described in 1904.[1] The disease is characterized by diminished osteoclast-mediated bone resorption leading to increased bone density; however, these bones are brittle. Thus, “osteopetrosis” is a misleading term as bones are extremely brittle and prone to fractures instead of the literal meaning of “hard as stones.” The disease apart from being a gamut of clinic-radiological findings also has a different spectrum of severity according to the inheritance pattern.[1,2] Here, we discuss the imaging of a patient with osteopetrosis with a very rare presentation.
CASE REPORT
An 18-year-old male presented with abdominal pain and tenderness in the right iliac fossa to the emergency of our hospital. The patient was referred to the Department of Radiodiagnosis for an abdominal X-ray. There was abnormal sclerosis in the vertebrae and pelvic bones with bone within-bone appearance. There was also seen localized mottled appearance of air shadows in the right iliac fossa [Figure 1] and sandwich appearance of the vertebrae due to densely sclerotic endplates. Further, the complete skeletal survey was planned and an abdominal contrast-enhanced computed tomography (CECT) was performed. The CECT abdomen shows a [Figure 2a and b] large heterogeneous collection with air foci in the right iliac fossa, with diffuse wall thickening of the cecum and right-sided colon. The X-ray of the right leg shows characteristic Erlenmeyer deformity as flaring and elongation of the distal and proximal tibial metaphysis [Figure 3a]. The X-ray of the pelvis shows bone within-bone appearance in iliac wings with characteristic changes in the femur [Figure 3b]. The X-ray hand revealed diffuse sclerosis of all the bones with no corticomedullary differentiation and alternating radiolucent bands in phalanges [Figure 3c]. The hematological findings on the contrary showed leukocytosis with neutrophilia. The presumptive diagnosis of osteopetrosis with non-neutropenic enterocolitis and perforation peritonitis was made. The patient was planned for laparotomy and intraoperatively perforation was observed in the right colon near the cecum and signs of ischemia involving the terminal ileal loop, cecum, right colon up to hepatic flexure with necrosis, and thickening of the walls which correlated with the imaging findings. Due to the poor general condition of the patient, an ileostomy was done and major resection was postponed. The patient was shifted to the intensive care unit. Unfortunately, the patient could not survive due to sepsis and multisystem failure with underlying bone disorder and typhlitis causing perforation peritonitis.

- X-ray abdomen showing mottled air shadows in the right iliac fossa with sclerosis in visualized ribs and loss of corticomedullary differentiation giving sandwich appearance of the vertebrae. Alternating bands are also noted in visualized bilateral iliac wings.
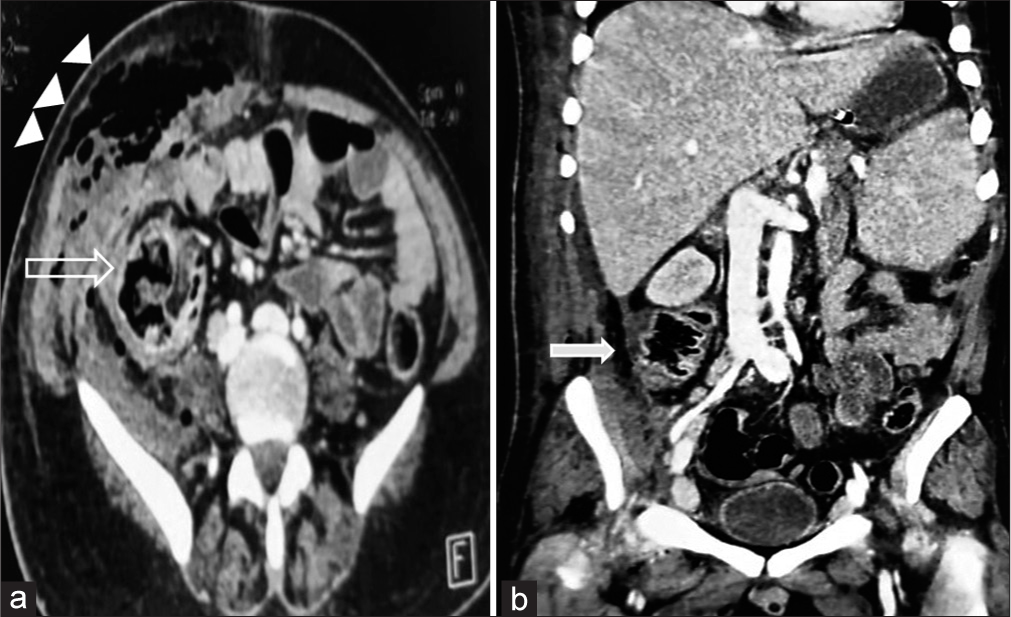
- Axial (a)and coronal (b) contrast-enhanced computed tomography image showing diffuse wall thickening of caecum (open arrow) and ascending colon with pneumatosis coli and localised collection in right paracolic gutter with air foci in it s/o perforation peritonitis (solid arrow). There are also seen multiple air foci and abscess formation in the abdominal wall on right side (arrowheads).
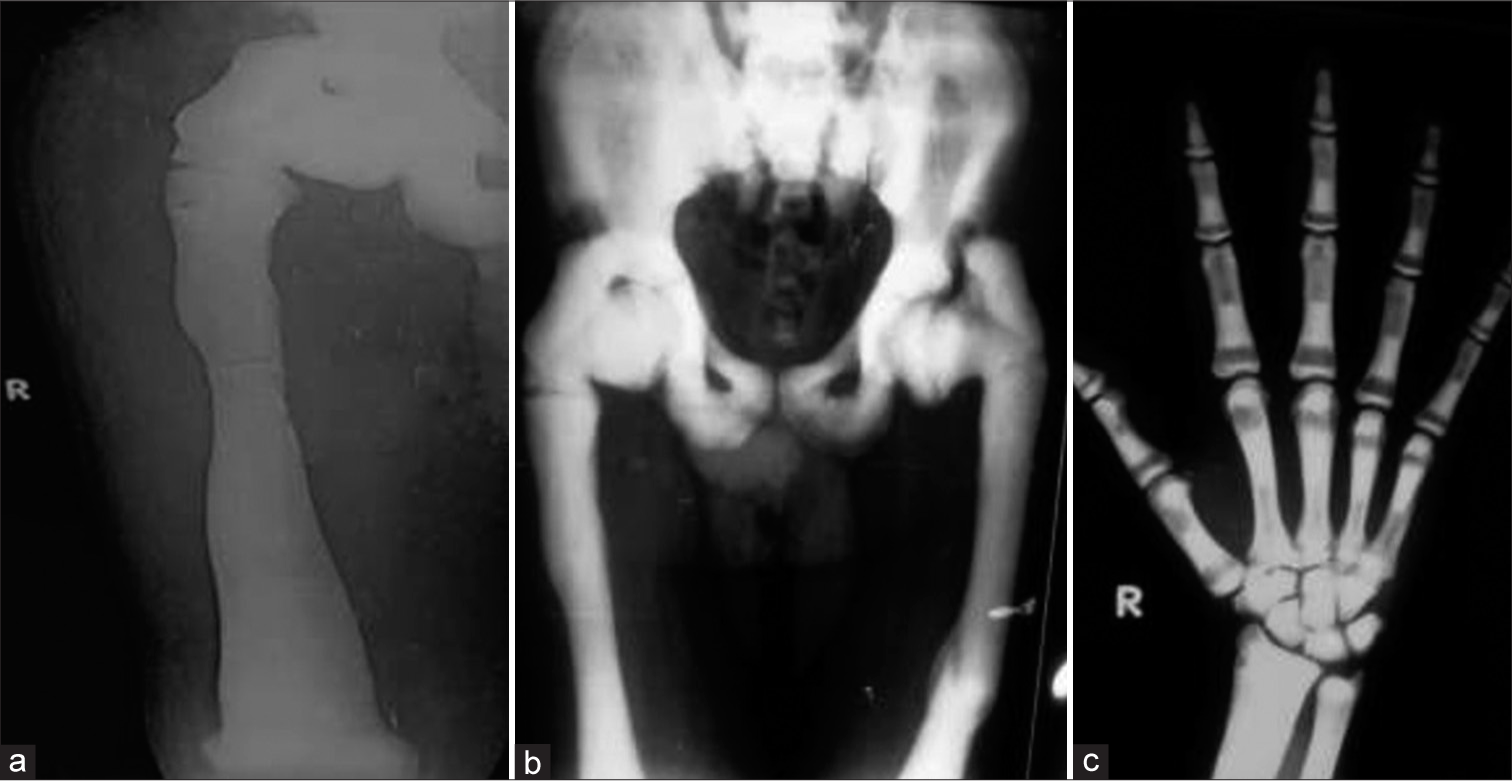
- (a) X-ray right thigh showing flaring of the distal femoral metaphyses (Erlenmeyer flask deformity). There are also seen a fracture in subtrochanteric region. (b) X-ray pelvis showing bone within bone appearance in iliac crest and densely sclerotic deformed femurs with old healed fracture in femur. (c) X-ray posteroanterior view hand seen showing dense sclerosis with loss of corticomedullary differentiation and radiolucent and dense alternating lines with bone in bone appearance.
DISCUSSION
Osteopetrosis presents mainly as autosomal recessive or dominant inheritance with an incidence of 1 in 250,000 and 1 in 20,000, respectively.[2] Autosomal dominant osteopetrosis (ADO) is also known as Albers Schonberg after a German Radiologist who described it for the 1st time. This is a milder manifestation of the disease which has a late incidental presentation in the form of multiple fractures, osteomyelitis, and related complications. However, the recessive form has a much more aggressive course in the form of compression of cranial nerves and marrow dysfunction. Imaging plays an important role in diagnosing osteopetrosis and detecting its various complications. According to the literature, there are two more types which include an intermediate recessive type which has lesser severity, and lastly, a recessive type presenting with renal tubular acidosis which is also known as carbonic anhydrase II deficiency syndrome.[3]
The spectrum of features of osteopetrosis includes cranial nerve palsies due to foraminal stenosis at the skull base and bone marrow dysfunction with extramedullary hematopoiesis, causing hepatosplenomegaly. There is seen an increased risk of infections due to poor bone marrow function. The normal balance between bone formation and resorption is altered in osteopetrosis with osteoclastic dysfunction resulting in persistent primitive osteoid tissue of primary spongy bone. This interferes with the formation of normal mature adult trabeculated bone causing abnormally dense sclerotic but brittle bones.[4,5] In our present case, the patient presented with pain in the abdomen as the chief complaint due to underlying typhlitis.
The imaging findings which are characteristic of the disease help in the early diagnosis and appropriate management of the patient. Apart from seeing diffuse sclerosis causing obliteration of the medullary cavity, there is seen Erlenmeyer deformity which is flaring and elongation of ends of long bones. There are seen alternating lucent and sclerotic bands in metaphysis due to the cyclical nature of the disease process. There is a bone-in-bone appearance due to this alternating course of the underlying process which is also seen in our case. This finding differentiates osteopetrosis from other sclerosing dysplasia.[6] The same findings, when seen in the spine, are also called sandwich vertebrae due to endplate sclerosis. There are certain imaging features favoring the characteristic types of osteopetrosis on radiographs. The radiographic features of ADO type I showing more pronounced sclerosis of skull vault with thickened enlarged cranial vault can be helpful in differentiating from ADO type II which shows more sclerosis at skull base. The hematological manifestations as myelophthisic anemia with neutrophilia, immature granulocytes, and nucleated red blood cells on peripheral blood smear.[7] Hepatosplenomegaly is seen due to extramedullary hematopoiesis. However, thrombocytopenia, leukopenia, and hemolytic anemia may also occur due to hypersplenism.
Neutropenic enterocolitis, also known as typhlitis as cecum, is referred to as typhlon (“blind”) in Greek. It is an acute life-threatening condition characterized by transmural inflammation of the cecum, often with the involvement of the ascending colon and ileum, in patients who are severely myelosuppressed.[8,9] Typhlitis is seen due to uncontrolled bacterial growth causing impairment of organ irrigation with progression to transmural ischemia and necrosis. At present, the incidence of typhlitis varies from 0.8% to 26% with around 5.3% of adult patients hospitalized for treatment of hematologic or solid malignancies, or bone marrow aplasia.[10] Moreover, further, the incidence of non-neutropenic colitis is only much rarer with few cases reported in the literature. These cases are attributed to some specific bacilli which can induce inflammation and necrosis of the cecum even in the absence of any underlying condition causing neutropenia.[10]
Differential diagnosis includes pyknodysostosis in which diffuse sclerosis is less pronounced and heavy-metal poisoning is the characteristic history of the patient. Classical features of osteopetrosis are seen on skeletal survey. These are also highlighted on the CT study which additionally revealed right side colon thickening with perforation and localized collection in the region.[2,3,6] Despite all early efforts, the patient could not survive attributed to the immune dysfunction related to the underlying bone disease. The disease carries high morbidity and mortality due to associated marrow and neurological dysfunction.[3,8]
The treatment of this disease is largely based on symptoms. While some may be asymptomatic, many of these patients will require orthopedic surgery at some point in their lives for fractures. Hepatosplenomegaly, thrombocytopenia, leukopenia, and hemolytic anemia are commonly seen due to marrow dysfunction which can be only definitively cured with a bone marrow transplant.
CONCLUSION
Although there could be a late presentation of the disease, still it carries high morbidity and mortality due to associated bone marrow and neurological dysfunction. This rare presentation of typhlitis with osteopetrosis led to adverse consequences in the present case. Therefore, it is contemplated to diagnose this disease as early as possible so that effective multidisciplinary management could be sought to reduce the morbidity and mortality associated with this disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Osteopetrosis: Radiological and radionuclide imaging. Indian J Nucl Med. 2015;30:55-8.
- [CrossRef] [PubMed] [Google Scholar]
- Carbonic anhydrase II deficiency. Clin Orthop Relat Res. 1993;294:52-63.
- [CrossRef] [Google Scholar]
- Sclerosing bone dysplasias: Review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31:1865-82.
- [CrossRef] [PubMed] [Google Scholar]
- Radiological, biochemical and hereditary evidence of two types of autosomal dominant osteopetrosis. Bone. 1988;9:7-13.
- [CrossRef] [PubMed] [Google Scholar]
- Typhlitis; is it just in immunocompromised patients? Med Sci Monit. 2008;14:CS67-70.
- [Google Scholar]
- Recurrent typhlitis. A disease resulting from aggressive chemotherapy. Dis Colon Rectum. 1989;32:206-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neutropenic enterocolitis in adults: Systematic analysis of evidence quality. Eur J Haematol. 2005;75:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Nonneutropenic acute typhlitis associated to gram-positive Bacillus: Clinicopathological series. Int J Colorectal Dis. 2016;31:1227-8.
- [CrossRef] [PubMed] [Google Scholar]






