Translate this page into:
Patterns of injuries in sports groin: Review and pictorial essay

*Corresponding author: Riya Samanta, Department of Radiology, Mahajan Imaging and Labs, Safdurjung Hospital Sports Injury Centre, New Delhi, India. samanta.ria1011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Samanta R, KSV Abhinetri, Gupta H, Rajan S, Batta NS. Patterns of injuries in sports groin: Review and pictorial essay. Indian J Musculoskelet Radiol. 2025;7:65-76. doi: 10.25259/IJMSR_44_2024
Abstract
Sports-related groin injuries are prevalent in multidirectional sports and typically present with inguinal pain and localized tenderness. These injuries can be disabling, leading to missed practice and warranting prolonged absences from sports events, potentially compromising a professional athlete’s career. These injuries are difficult to diagnose due to the complex anatomy and pathophysiology. Imaging, particularly high-resolution magnetic resonance imaging, is excellent for evaluating cause, location, and severity of groin injuries. Understanding the anatomy of the groin and recognizing specific patterns of imaging findings is crucial for accurate diagnosis and targeted treatment planning.
Keywords
Common adductor-rectus abdominis aponeurosis injury
Osteitis pubis
Pre-pubic plate
Secondary cleft
Sports groin
INTRODUCTION
Sports-related groin injuries are prevalent across various sports, particularly in multidirectional activities involving repetitive lateral ambulation, frequent and forceful trunk twisting, and kicking, such as in soccer, ice hockey, basketball, baseball, football, and cricket.[1] These motions impose differential load shift and repeated significant stress on the pubic symphysis and its supporting musculature. Groin accounts for 2–8% of all athletic injuries, with nearly 13% of soccer-related injuries involving the groin.[2-5]
Athletes typically present with pain in the inguinal region with occasional radiation to the adductor muscle origin or the scrotum; physical examination reveals localized tenderness at the superficial inguinal ring, the pubic insertion of the rectus abdominis, the pubic tubercle, or the symphysis pubis without a palpable hernia.[2]
Groin pain presents a diagnostic and treatment challenge due to its complex pathophysiology and the intricate musculo-aponeurotic anatomy of the pubic symphysis. This interrelation of musculo-aponeurotic attachments results in the complex interplay between the forces generated by the muscles across the symphysis. Furthermore, the differential diagnosis is extensive, with overlapping clinical symptoms and findings from the physical examination [Table 1].[2,6] Multiple coexisting injuries can complicate the identification of primary pathology, making it difficult to establish which one cause is the main contributor. Given these complexities, both conservative and surgical treatments show variable success.[2] Many athletes struggle with groin pain due to a lack of a precise diagnosis or an effective cause-based management plan.[1]
| Osseous causes |
| Osteitis pubis |
| Overuse attritional changes |
| Stress fracture |
| Muscular causes |
| Common adductor-rectus abdominis aponeurosis injury |
| Rectus abdominis strain |
| Adductor muscle-tendon injury/dysfunction |
| Injuries of pyramidalis–anterior pubic ligament–adductor longus |
| Others |
| Inguinal hernias and varicoceles |
| Referred pain |
| Compression of upper lumbar nerves |
| Acetabular labral tears |
| Femoroacetabular impingement |
| Tendinosis/tears of muscles nearby, such as sartorius, |
| Nerve entrapment syndromes-nerves coursing through the groin region such as iliohypogastric, ilioinguinal, obturator, and femoral and genitofemoral nerves. |
High-resolution magnetic resonance imaging (MRI) is pivotal in evaluating sports-related groin pain, offering precise insights into injury location and severity. X-rays are a valuable adjunct to diagnosing pubic bone irregularity, pubic instability, and calcific tendinosis. Ultrasound is a quick and reliable modality for diagnosing adductor tears and guided injections. A knowledge of the anatomy of the groin and familiarity with the imaging findings allows accurate diagnosis and treatment planning, particularly in targeting specific pathologies.[2,6]
In this article, we discuss the anatomy and biomechanics of the pubic region and describe the pathophysiology of sports-related injuries occurring in this region. We, further, discuss the imaging features, chiefly focusing on the MRI features associated with sports-related groin pain. Finally, we review some common confounding causes with clinical manifestations similar to those of sports groin.
ANATOMY AND BIOMECHANICS
The “groin” lacks a fixed anatomical definition and is considered an area spanning the symphysis pubis, the contiguous thigh adductor compartments, and the inguinal regions.[7]
The symphysis pubis is a non-synovial diarthrodial joint formed by bilateral pubic bones separated by a fibrocartilaginous articular disc that stabilizes the pelvis surrounded by the joint capsule, reinforced by anterior, posterior, superior, and inferior pubic ligaments[6,8] [Figure 1]. The inferior pubic ligament (or arcuate ligament)[6] and anterior pubic ligament are the main passive stabilizers, the latter is part of the pre-pubic aponeurotic complex/pre-pubic plate[9] or the pyramidalis-anterior pubic ligament-adductor longus complex (PLAC).[10]
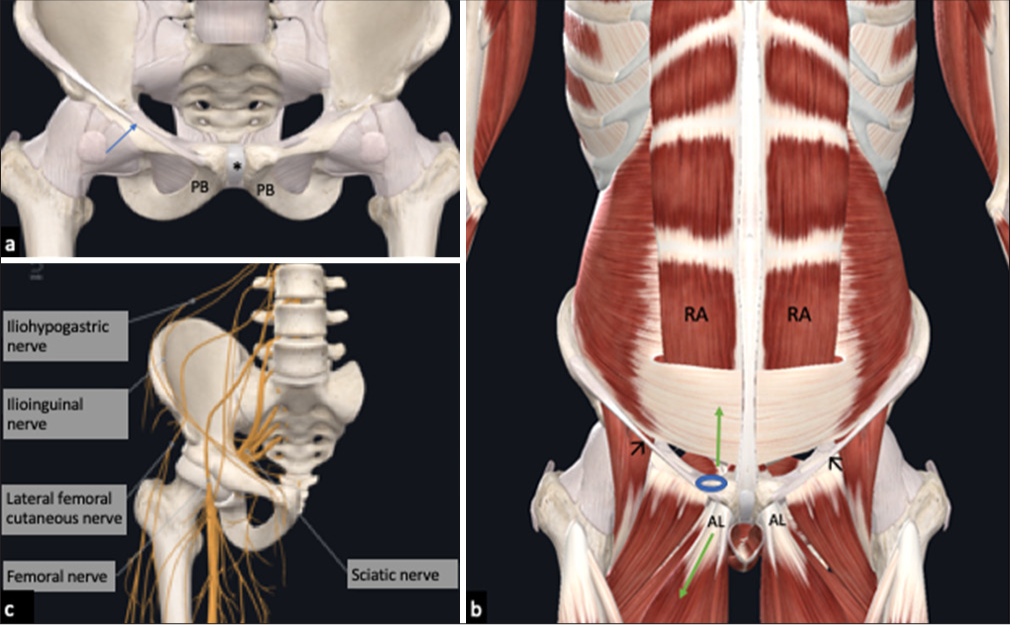
- Diagrammatic representation of the anatomy of the groin. (a) Normal anatomy of the symphysis pubis composed of bilateral pubic bones (PB) with intervening fibrocartilaginous articular disc (*). The blue arrow denotes the inguinal ligament. (b) Schematic representation of the relationships and sites of attachment of the major muscles—the rectus abdominis (RA), adductor longus (AL)— and the inguinal ligament (black arrows) to the symphysis pubis. Green arrows denote the direction of the major force vectors to which the PB is commonly exposed during athletic activities. The lateral margin of the common adductor-RA aponeurosis lies just deep to the superficial inguinal ring (blue circle). (c) Nerves coursing through the groin region.
Traditional descriptions of the symphysis pubis emphasize a pre-pubic aponeurotic complex/pre-pubic plate,[9] with the rectus abdominis muscles continuing with a pre-pubic aponeurotic layer, the adductor longus (AL) aponeurosis and merging with the arcuate ligament, pectineus, and the pubic periosteum. More recent work has revealed a pyramidalis-anterior pubic ligament complex (PLAC)[10] with the pyramidalis muscle continuous with the anterior pubic ligament and the AL aponeurosis that we discuss in more detail below in Figures 2 and 3.
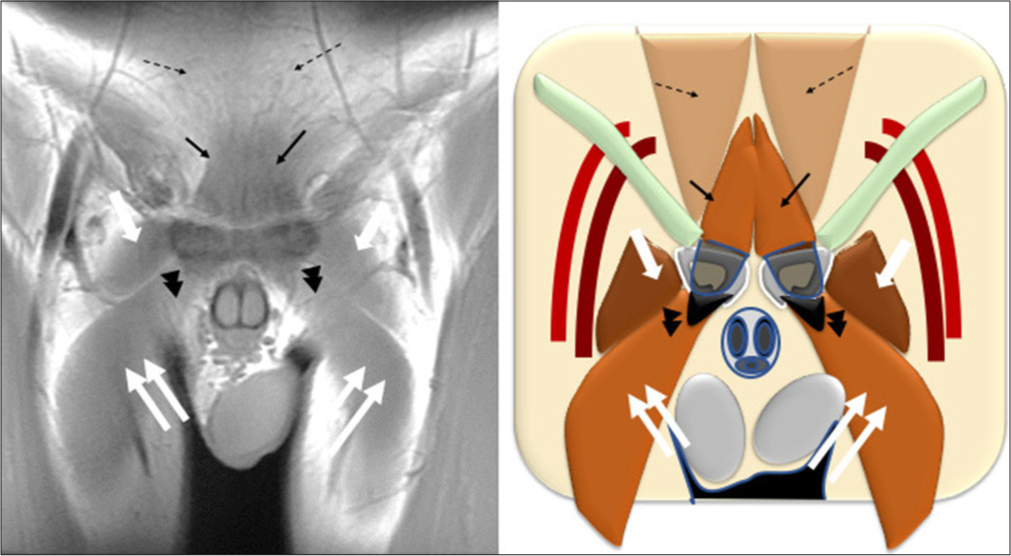
- Oblique coronal T1-weighted image through pubic tubercle (left) and diagrammatic representation (right). Pyramidalis (thin black arrow) continuing with the anterior pubic ligament (not as well seen enface) and thence to the adductor longus aponeurosis (black arrowheads) and adductor longus muscle (double white arrows). Pectineus (large white arrows) seen lateral to the adductor longus on this anterior coronal section. The rectus abdominis muscles (dashed black arrows) coursing posterosuperior to the pyramidalis and inserting on the superior surface of the pubic ramus.
- Parasagittal T1-weighted image through pubic tubercle (left) and diagrammatic representation (right). Pyramidalis (thin black arrows) inserting on anterior pubic ligament (double thin black arrows) and thence to the adductor longus aponeurosis (black arrowheads). Adductor fibrocartilage deep to the aponeurosis (thin white arrows). The rectus abdominis (thick white arrows) inserting on the superior surface of the pubic ramus.
Several fibrous/aponeurotic and muscular layers close to the symphysis pubis described on dissection, from anterior to posterior, are as follows-
Aponeurosis of the abdominal oblique and transversalis muscles connecting with the fascia lata through the superficial layer of the anterior pubic ligament (this may have functional significance for “sports hernia.”).
Paired pyramidalis muscles continuous with the anterior pubic ligament and the AL aponeurosis.
Aponeurotic layer separating the pyramidalis muscles from the distal rectus abdominis muscle insertions.
Rectus abdominis muscle slips inserting on the superior pubic ramus at a thin crest with thin internal and broader external tendons. The broader lateral/external tendon attaches to the superior pubis between the pubic tubercle and the symphysis pubis. It is continuous with the fascial lata and gracilis, while the medial/internal tendon interlaces with the opposite tendon and is continuous with the gracilis and fascia lata.
The AL originating from the inferior aspect of the pubic crest through a triangular fibro-cartilaginous enthesis at the pubic footprint (with a shark fin-like appearance), continuing as a flat and broad tendon, with the eventual broad insertion at the mid-thirds of the femur. This muscle helps stabilize the pelvis during gait and causes thigh adduction.
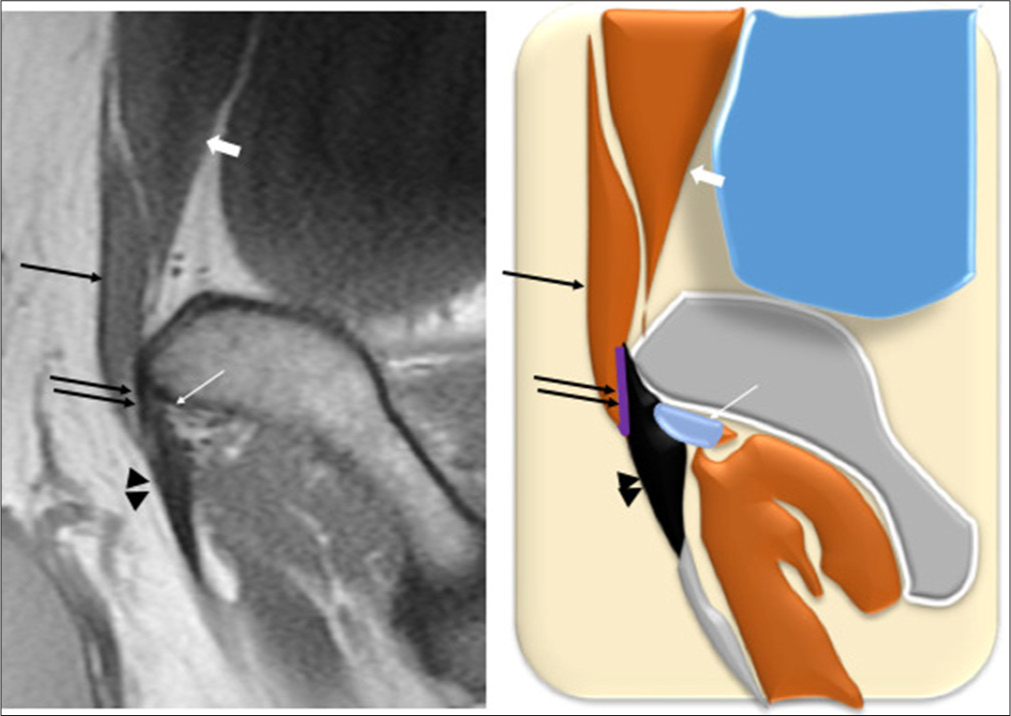
The adductor brevis and gracilis muscles originate further posterolaterally from the inferior aspect of the body of the pubis and inferior pubic ligament.[11,12] The pectineus muscle originates at the superior aspect of the pubic crest and lies lateral to the lateral head of the rectus abdominis. Of critical importance is that some of the medial fibers of the tendons of the AL and brevis attach directly to the pubic symphyseal capsule and articular disc [Figure 4].[6]
- Normal magnetic resonance imaging of the symphysis pubis. a-c T1-weighted axial MR images superior to, at and inferior to the symphysis pubis. (a) The medial and lateral heads of rectus abdominis muscles (white arrows) have been shown. The anterior wall rectus sheath continues with the external oblique aponeurosis and forms the anterior as well as the posterior walls of the inguinal canal (white arrowheads). (b) The rectus abdominis tendons blend anterior to the pubic bones and insert onto the anterior pubic ligament (white arrows). (c) Demonstrates the adductor longus tendons (black arrowheads), seen as areas of triangular dark signal arising inferior to the pubic crest. The adductor brevis (Ab), obturator externus (Oe), obturator internus (Oi), and pectineus (Pec) muscles are indicated. (d) Midline sagittal T2-weighted image showing normal rectus abdominis-adductor aponeurotic plate/pre-pubic plate (dotted arrow). (e) Sagittal T2-weighted image, some slices lateral to midline showing normal rectus abdominis-adductor aponeurosis/pre-pubic plate (black arrowhead) with origin of the adductor tendon inferiorly. (f) Coronal T1-weighted image showing both heads (M, L) of the distal right rectus muscle. The tendons from bilateral medial heads (M) blend with each other and merge with anterior pubic ligament. The lateral head (L) arises from the pubic tubercle and crest. The adductor longus tendon (black arrowhead) arises from the anterior part of pubic bone, inferior to the crest and blends with the contralateral tendon across the midline.
As the symphysis is a flat structure longitudinally oriented, it is most vulnerable to vertical shear stress[13] during the normal walk cycle, when the lower limbs alternate in weight bearing, shifting the load through the pelvis to the opposite limb. The horizontally oriented fibers of the internal oblique and transversus abdominis muscles impart horizontal compressive forces, resulting in the apposition of bilateral pubic rami and stabilization of the joint. With extension and rotation, the rectus abdominis and AL act as antagonists, with the recti elevating the pubic region and the adductors exerting an anteroinferior force vector. Injury to one tendon/muscle causes a tendency to injure the opposing tendon by disrupting the biomechanics and the anatomical interrelationship of the ordinary teno-periosteal origins, subsequently resulting in pubic symphyseal instability [Figure 1].[14] This symphyseal instability most often results in the development of osteitis pubis and eventually, chronic groin pain in many athletes. Once the symphysis region becomes unstable, athletes tend to carry on the activity with altered/abnormal biomechanics, leading to variable musculoskeletal injuries in the pelvis. When imaging sports groin patients, it is crucial to acknowledge these distinctive biomechanics.[15,16]
Furthermore, injury to the common adductor–rectus origin may also derange the attachment of the posterior inguinal canal wall to the anterior rectus sheath, causing a deficiency leading to a direct inguinal hernia formation.[6]
Multiple nerves coursing through the groin region and inter-abdominal musculature may be entrapped, such as the iliohypogastric, ilioinguinal, obturator, femoral, and genitofemoral nerves. These conditions are usually diagnosed based on clinical findings, with imaging used as a supplementary aid[6] [Figure 1].
Historically, a heterogeneous taxonomy has been used for athletic groin injuries, adding to much confusion in assessing this complicated area. Clinical practice becomes more challenging with clinicians using varying terminologies for groin pain, and even the same term can have differing interpretations. Hence, after a conference in Doha, a consensus on the definition of groin pain and various terminologies was held on November 04, 2014, to settle this problem. The aim was to agree on a standard vocabulary with accompanying definitions, and the following defined clinical entities were used to categorize groin pain: [17]
Adductor-related,
Iliopsoas related,
Inguinal related, and
Pubic-related groin pain.
Other subsequent consensus statements, including the Manchester and Italian consensus statements, are related to terminology and irrelevant to this discussion.
IMAGING APPROACH AND TECHNIQUE
This first radiological modality of radiographic (X-ray) assessment of the pelvis allows analysis of the pubic symphyseal alignment and arthropathy. Furthermore, it helps in screening of the sacroiliac joints, the lower lumbar spine, and hips. If X-rays reveal positive findings, this can be further investigated with MRI or ultrasonography (USG). While performing USG, clinical history can be obtained simultaneously and focus on the site of pain or symptoms can be made. Dynamic scanning can assess abnormalities of the inguinal canal, and interventions can be performed if necessary.[6] MRI is the preferred imaging modality due to its high sensitivity (98%) and specificity (89–100%) in evaluating sports-related groin pain, particularly for injuries involving the symphysis pubis, rectus abdominis, and adductor tendon origin.[14] It also offers the advantage of detecting abnormalities in adjacent muscles and tendons, symphyseal effusions, intra-articular disc extrusion, “secondary cleft,” and marrow edema.
MRI scanning protocols include large field-of-view (FOV) T1-weighted and fat-saturated fluid-sensitive sequences of the bony pelvis, hips, and groin. After review, these images help guide further high-resolution imaging. Typical high-resolution protocols for the groin involve sagittal T1-weighted and fat-saturated proton density or T2-weighted scans, followed by oblique scans. While some institutions follow oblique axial and coronal fat-saturated T2-weighted images parallel to and perpendicular to the iliac crests or symphysis pubis, respectively Figure 5, others follow oblique coronal images parallel and perpendicular to the adductor fibrocartilage (FC), rectus abdominis, and AL aponeurosis.
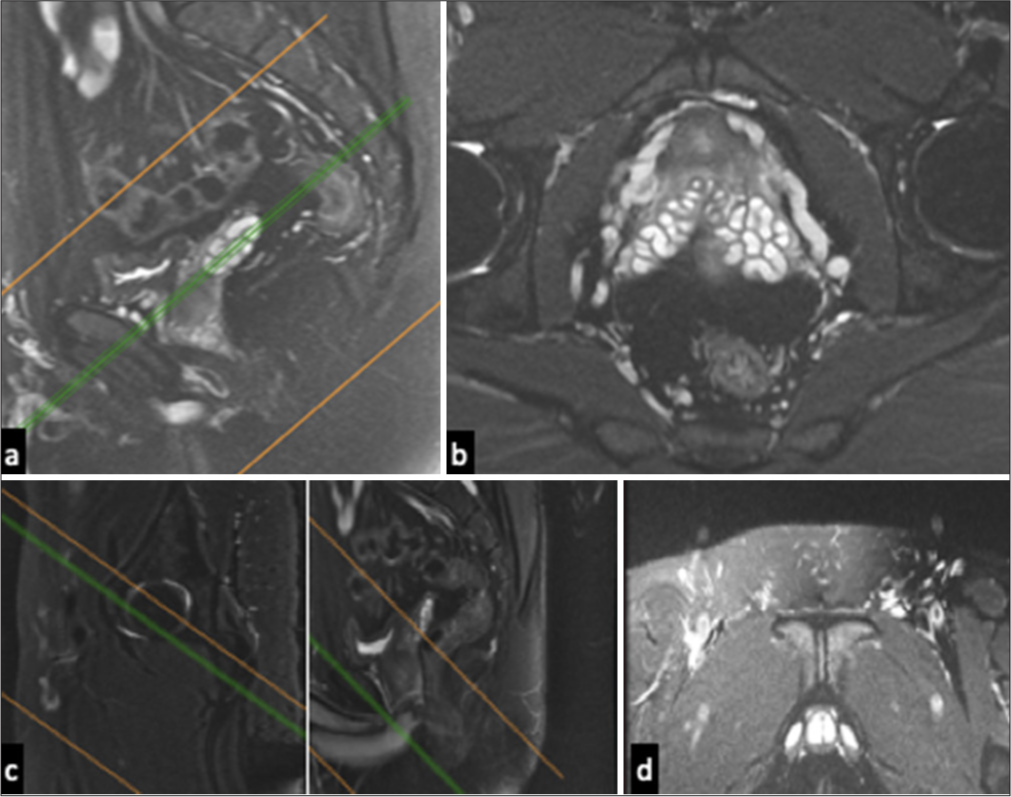
- (a) Sagittal T2-weighted fat-suppressed image obtained near the medial acetabulum shows the plane (lines) determined for axial oblique magnetic resonance (MR) imaging of the pubic region, which parallels the iliopectineal line and is perpendicular to pubic symphysis. (b) Axial oblique T2-weighted fat-suppressed image shows normal muscles around the pubic symphysis. (c) Sagittal T2-weighted fat-suppressed image shows the plane (lines) determined for coronal oblique MR imaging of the pubic region, which is perpendicular to the iliopectineal line and parallel to the pubic symphysis. (d) Coronal oblique T2-weighted fat-suppressed image shows normal muscles around the pubic symphysis.
IMAGING FINDINGS OF THE DIFFERENTIAL DIAGNOSES
The superior and secondary cleft
Distinct clefts on imaging reported at the symphysis pubis include the primary cleft, which is developmental and noted in 10% of adults at the central portion of the symphyseal articular disc posterosuperiorly. When seen at MRI, the primary cleft is a vertically oriented midline hyperintense signal on fluid-sensitive sequences.
The superior and inferior cleft signs first described in fluoroscopy-guided pubic symphyseal arthrography with contrast injected within the region of the primary cleft extended inferolateral to the symphysis unilaterally in a curvilinear pattern. Similar cleft signs described on fluid-sensitive sequences on magnetic resonance (MR) are linear signals.
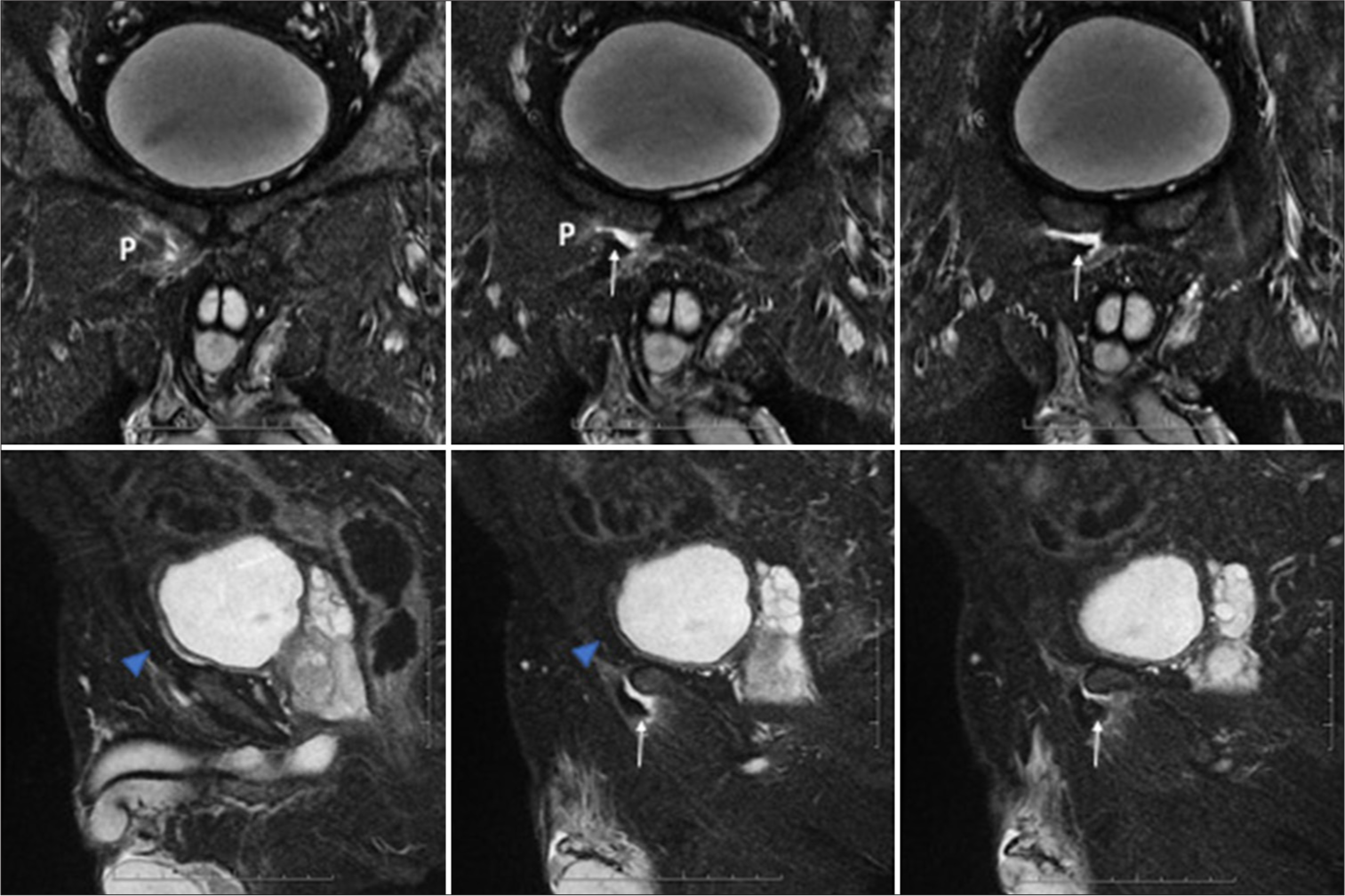
The “secondary cleft sign” describes a linear signal on MR extending from the symphysis pubis parallel to and inferior to the inferior pubic ramus, representing tears of the adductor brevis and gracilis tendon origins[1,2] [Figure 6].
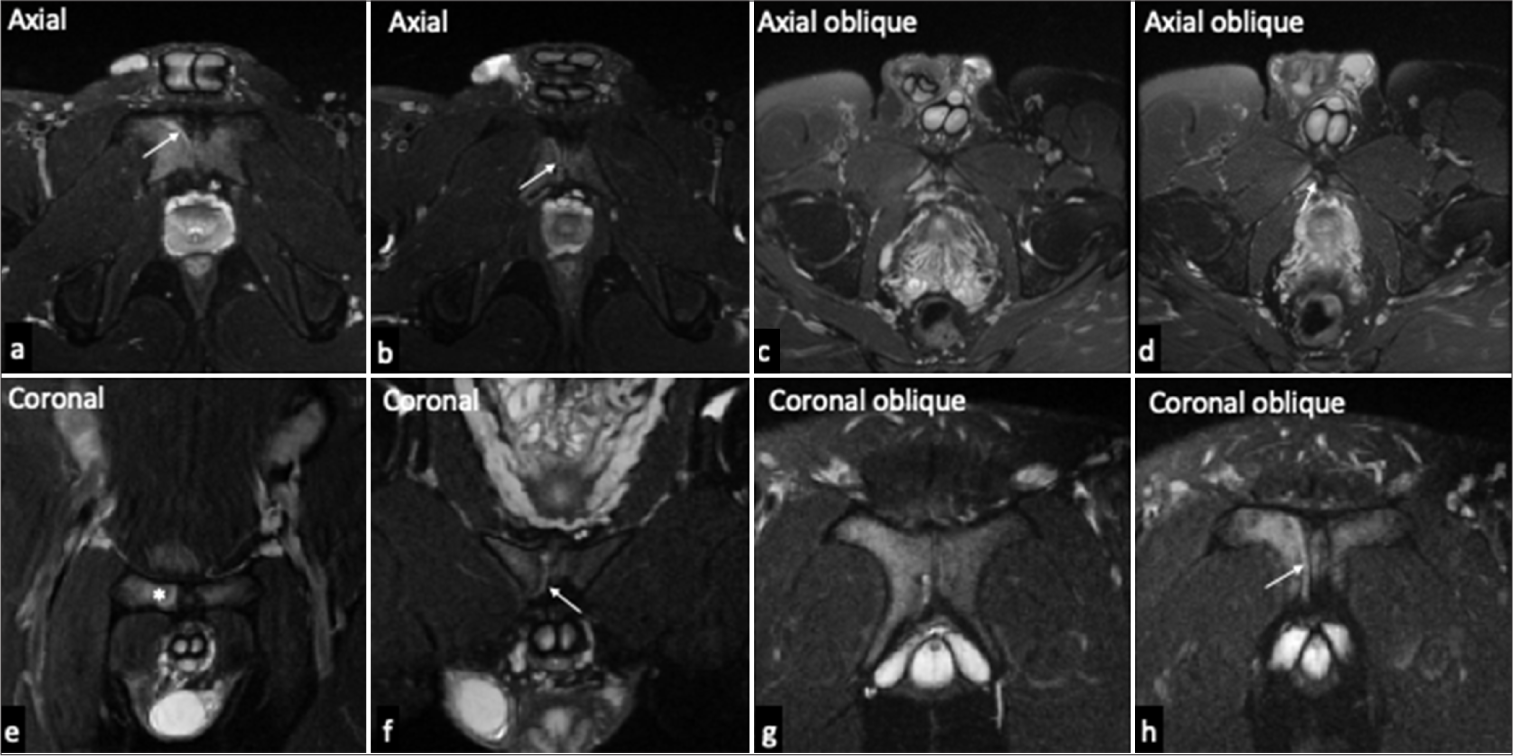
- Secondary cleft (white arrow) in a 24-year-old male basketball player with right sided groin pain. (a and b) Serial Axial (c and d) Axial oblique, (e and f) Coronal, and (g and h) Coronal oblique T2-weighted fat-suppressed serial images of the symphysis pubis depicts a crescentic hyperintense area adjoining the hyperintense signal interpubic articular disk along the anterior-inferior margin of the medial pubic body, close to the common adductor-rectus abdominis aponeurosis. Mild adjacent bone marrow edema osteitis pubis-denoted by * is noted on the right side.
The “superior cleft sign” describes a linear signal on MR extending from the symphyseal cleft along the inferior curve of the superior pubic ramus, representing a tear of the AL aponeurosis.[2,18-20]
Osteitis pubis
Osteitis pubis is a painful inflammatory response from altered biomechanics at the symphysis. It leads to osteochondral changes, instability, and degeneration of the central articular disc, rendering the articular surfaces vulnerable to trauma during activity.
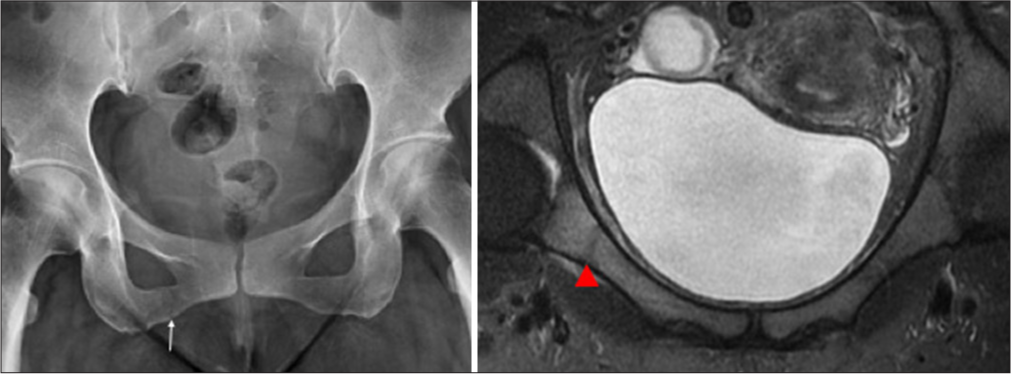
X-Rays show erosive changes, surface irregularities, and sclerosis,[12] with positive findings emerging about a month after symptom onset [Figures 7 and 8].
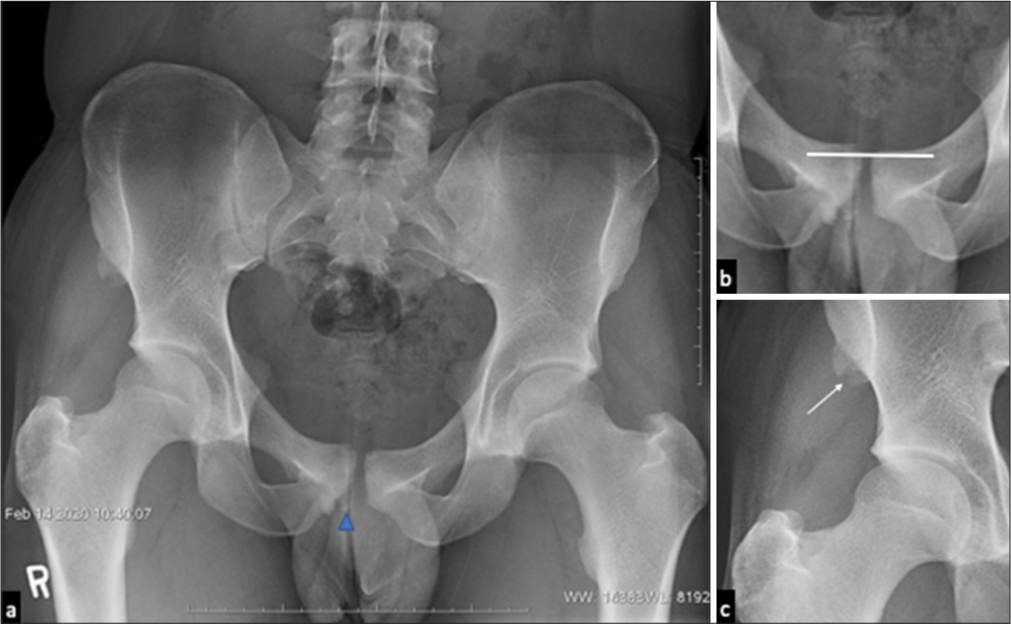
- (a) Plain radiograph of a 20-year-old male footballer with right-sided groin and hip pain reveals osteitis pubis with subchondral erosive change, articular surface irregularity and sclerosis of the symphysis pubis-findings being more prominent on the right side. Small soft-tissue ossification (blue arrowhead) at the site of adductor tendon attachment likely representing calcific tendinopathy. (b and c) Magnified radiographic images reveal a prominent offset at the symphysis pubis (straight horizontal line showing the offset) representing macro-instability and old avulsion injury (white arrow) at the right anterior superior iliac spine, site of sartorius origin.
- (a) Plain radiograph of pelvis of a 21-year-old footballer with osteitis pubis showing prominent step-off (straight horizontal line) at the symphysis suggesting macro-instability and chronic apophyseal avulsion injury at the hamstring origin, right ischial tuberosity (white arrow). (b) Plain radiograph of pelvis of a 20-year-old male footballer showing sclerosis related to chronic osteitis pubis with insignificant articular step-off (straight horizontal line) at the symphysis suggesting micro-instability.
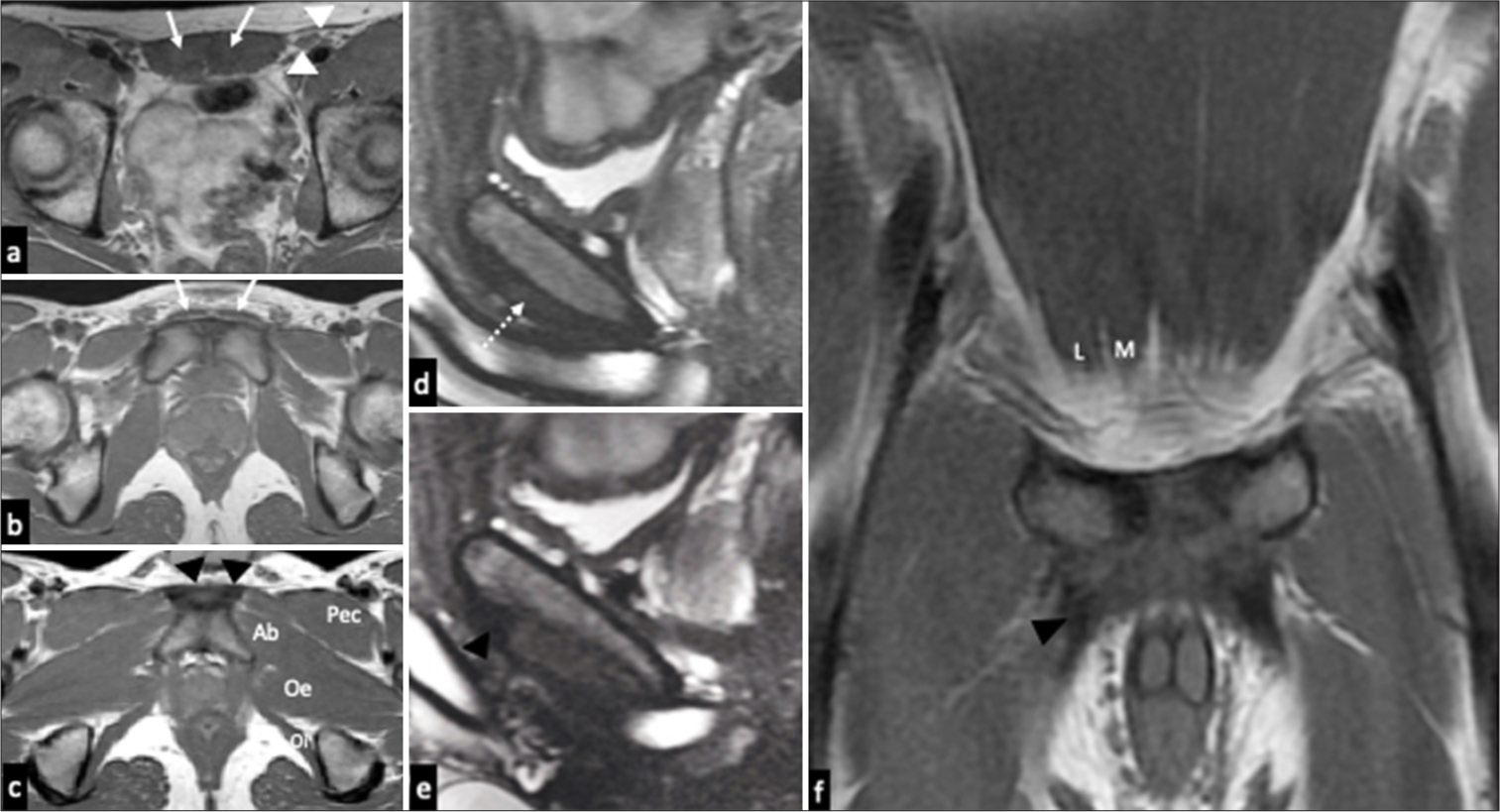
On MRI, acute osteitis pubis is seen in the subarticular location, either unilateral or bilaterally. In contrast, edema due to tendon avulsion/stress injuries at the pubic tubercle is in a subcortical or subperiosteal location. Chronic osteitis pubis exhibits arthritic changes such as subchondral cysts, sclerosis, and osseous resorption [Figure 9]. However, osteitis pubis and parasymphyseal soft-tissue injuries can coexist and identified together on MRI [Figures 10 and 11].[1,21-23]
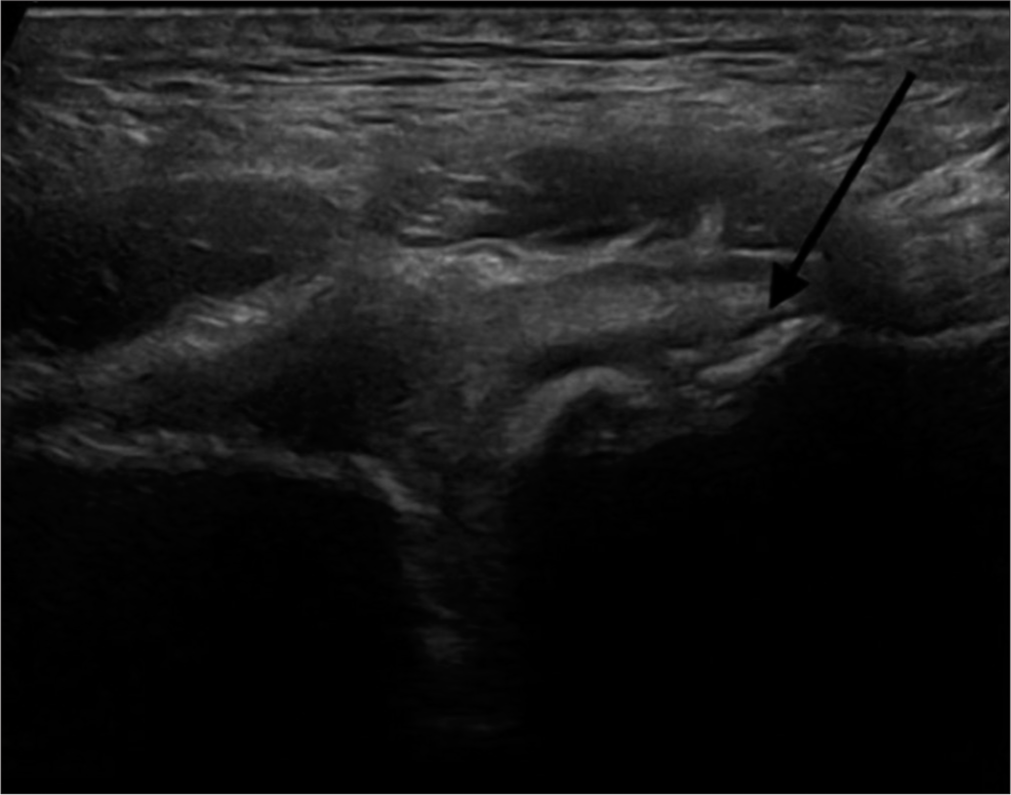
- Ultrasonography in a 36-year-old male footballer demonstrating chronic changes at pubis with diffuse bony irregularity of osteitis pubis (long black arrow)-evolved changes over time.
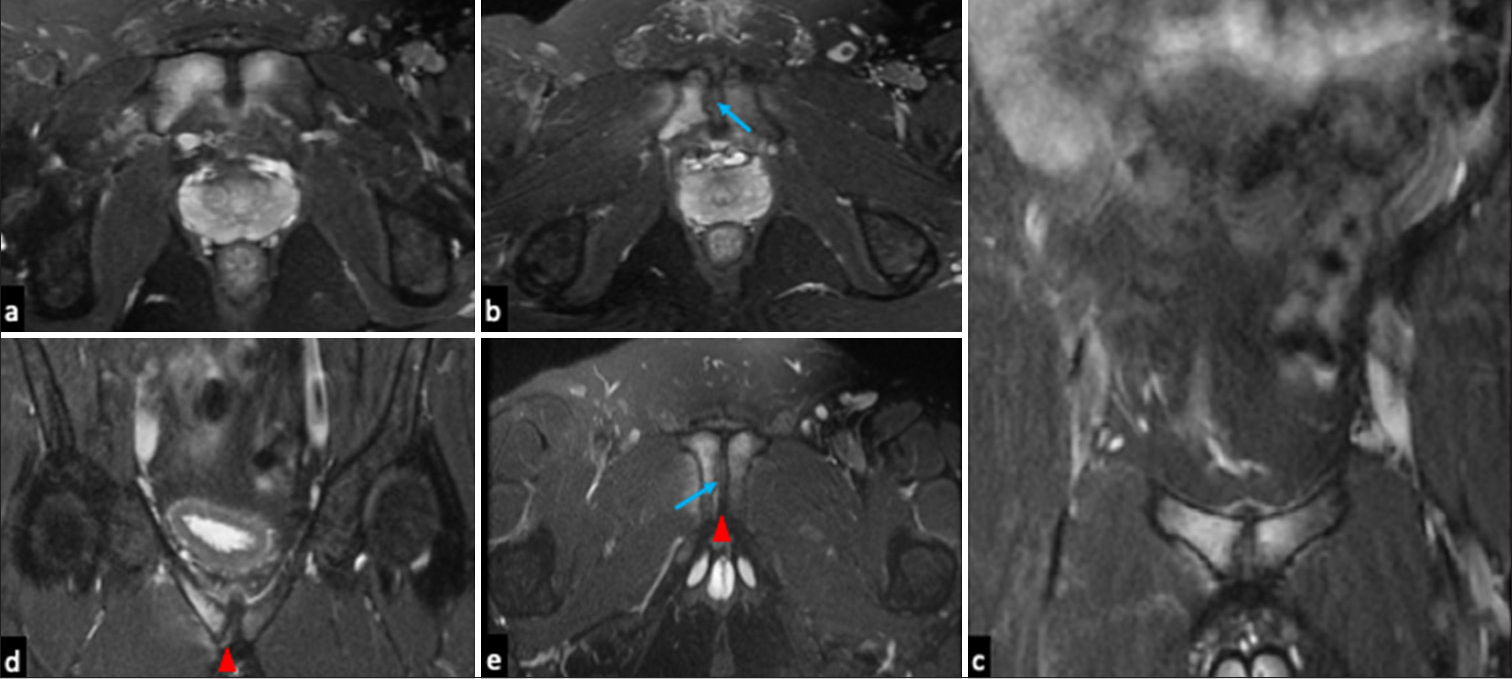
- Magnetic resonance images of osteitis pubis in a 17-year-old athlete with groin pain. (a and b) Axial T2 fat-suppressed images (c and d) coronal T2 fat-suppressed images and (e) coronal oblique fat suppressed images reveal bilateral parasymphyseal bone marrow edema with articular surface irregularity (blue arrow in b and e) showing right-sided dominance and presence of small right secondary cleft (red arrowhead in d and e).
- 17-year-old cricketer, painful left groin. Coronal T2 fat-suppressed images of the symphysis pubis reveals advanced degenerative changes with pubic symphyseal widening and marked irregularities in the pubic articular surface, more on the left side (white arrows).
Core muscle injury
Adductor dysfunction, particularly of the AL muscle, is the primary cause of groin and medial thigh pain due to its significant influence on the symphysis pubis. AL injuries are most prevalent, especially among soccer players, with a prevalence ranging from 44% to 60%.[9,24-26] Isolated injury to the rectus abdominis origin occurs in 27% of cases, while combined injury of the common adductor and rectus abdominis origin accounts for 27% of cases.[6,27]
Common Adductor-Rectus Abdominis Aponeurosis Injury typically involves concurrent damage to the caudal pyramidalis/rectus abdominis, the origin of the AL, and the periosteum of the pubic tubercle or the capsule of the pubic symphysis. This injury commonly results in interstitial tear or detachment of one or both rectus abdominis muscles at the symphysis and the AL tendons, often leading to chronic debilitating groin pain. However, in cases of acute or severe trauma, a complete disruption may occur between these structures, resulting in detachment and subsequent retraction.
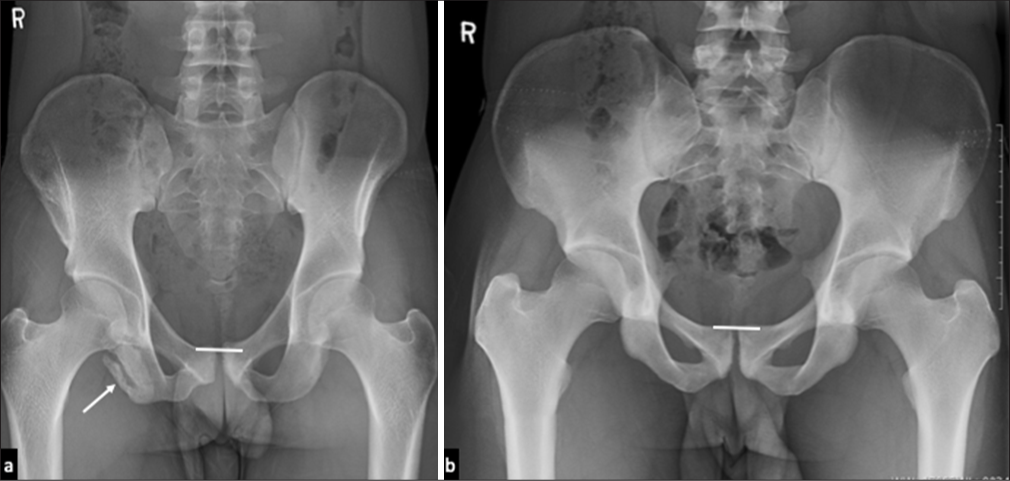
Common adductor-rectus abdominis aponeurosis injury is unilateral, affecting the lateral aspect of the caudal rectus abdominis, often leaving a gap near the posteromedial wall of the superficial inguinal ring. This injury presents with focal tenderness at the pubic tubercle and the superficial inguinal ring, resembling the condition frequently termed sportsman’s hernia.[1] Radiographs are usually normal in these cases; the earliest apparent abnormality is enthesopathy at the origin of each muscle, manifesting as ill definition of the bony cortex, which, when severe enough, can form a definite erosion.[6] Occasionally, bony avulsion at the rectus insertion can be the cause of groin pain which can be well visualized on plain radiographs [Figure 12]. The MRI findings of this injury are periosteal or subenthesial marrow edema on the pubic tubercle at the site of attachment of the rectus abdominis and thickening/interstitial tear at the origin of AL or interstitial delamination at the pre-pubic plate [Figure 13].[1] This type of injury is more likely to be treated surgically than isolated injuries of the rectus abdominis or adductor tendon.[1] Edema or atrophy of the rectus abdominis may also be noted near its tendinous attachment at the pubis.[2] Often, a unilateral secondary cleft is present.

- Plain radiograph in a 41-year-old female tennis player showing osseous avulsion at the site of right rectus abdominis insertion (white arrows).
- (a) Sagittal fat saturated MR images showing prepubic plate delamination (blue arrowhead). (b) Coronal oblique fat saturated MR images showing left sided osseous irregularity at pubic margin (white arrow).
In other cases, the rector-adductor aponeurosis injuries appear to be centered at the symphysis pubis on MRI and appear to extend to the medial edge of the two aponeuroses.
These midline injuries usually manifest as delamination/lifting of the entire apparatus from the symphysis region and may be called midline aponeurotic plate disruption. Both distal rectus abdominis muscles are affected, spanning the midline in transverse plane, creating confluent bilateral secondary clefts.[1]
Adductor syndromes
Several syndromes of the adductor compartment of thigh have been detailed in the literature of sports medicine and lesions of the adductor origin have been known to be a common cause of incapacitating groin pain in many athletes worldwide. The injuries may range from acute avulsions of the tendon origins [Figure 14] to strains of the muscle bellies or myotendinous junctions. Chronic injuries include degenerative proximal adductor tendinopathies and sometimes calcific tendinosis (hydroxyapatite deposition).
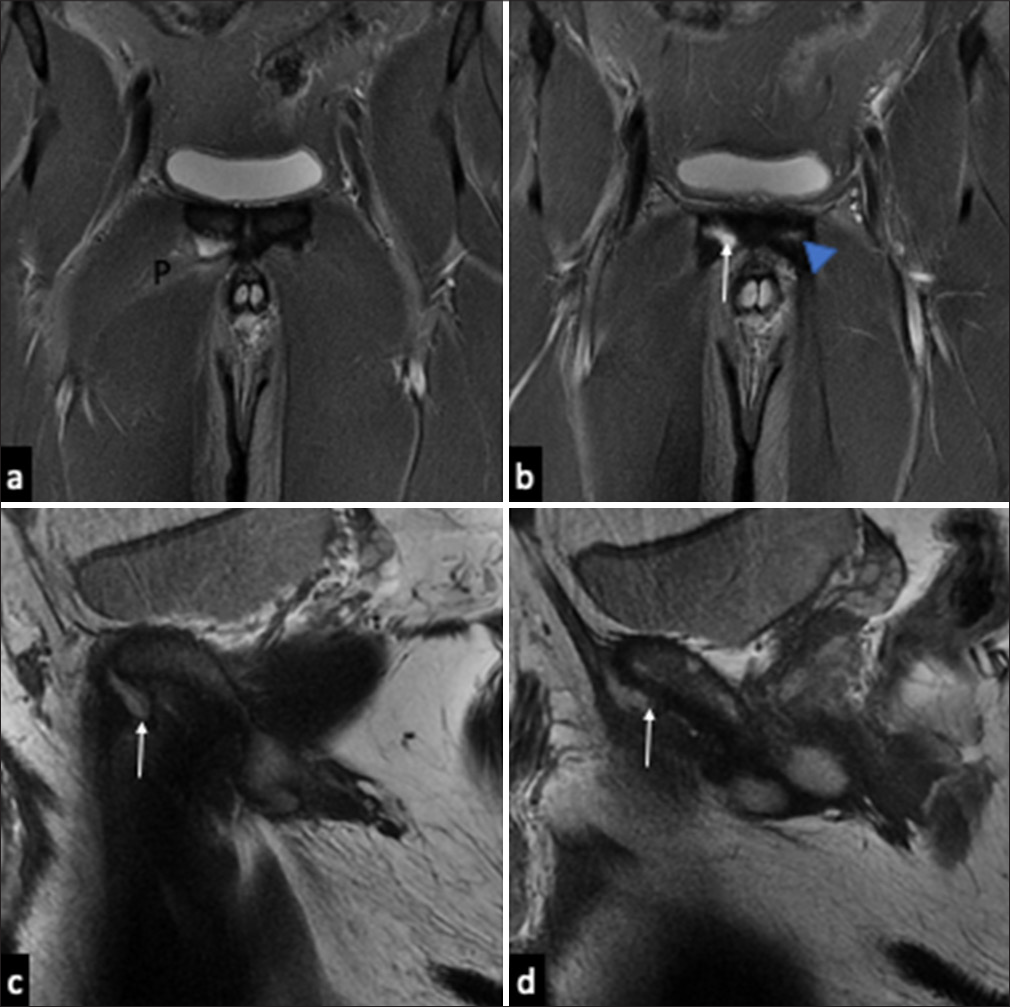
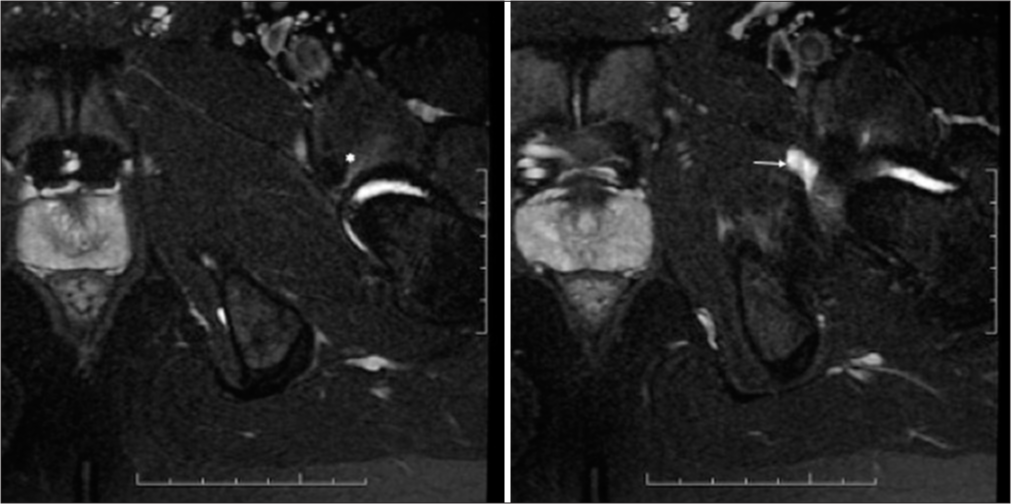
- 31-year-old footballer, right sided acute groin pain post play. (a and b) Coronal magnetic resonance images show traumatic avulsion of the right adductor longus tendon (white arrow) without significant retraction, and edema in the pectineus (P) muscle. Note the pre-existing tendinosis at the left adductor longus (blue arrowhead) giving credence to chronic adductor weakness predisposing to this tear. (c and d) Sagittal images reveal fluid marginating the adductor origin, with loss of normal hypointense triangular tendinous signal (white arrows).
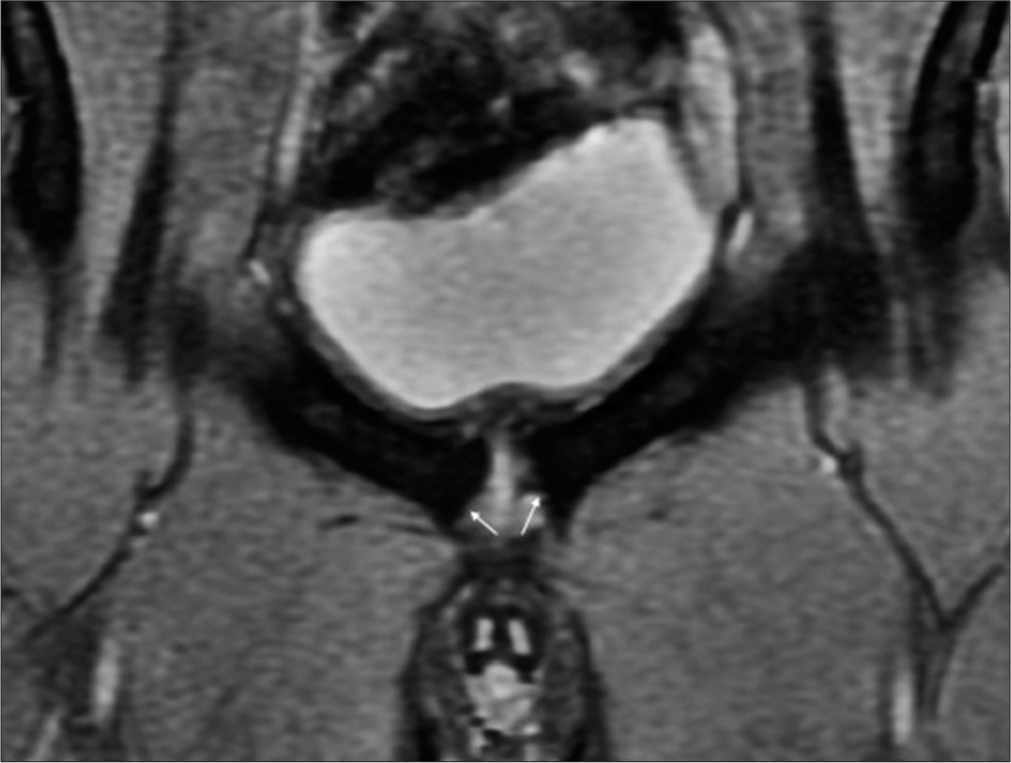
Complete AL avulsion with retraction should raise concern to search for a likely ipsilateral rectus abdominis injury on imaging [Figures 15 and 16]. An osseous avulsion may occur in isolation, but most frequently results in a large hematoma in the adductor compartment [Figure 17].[28]
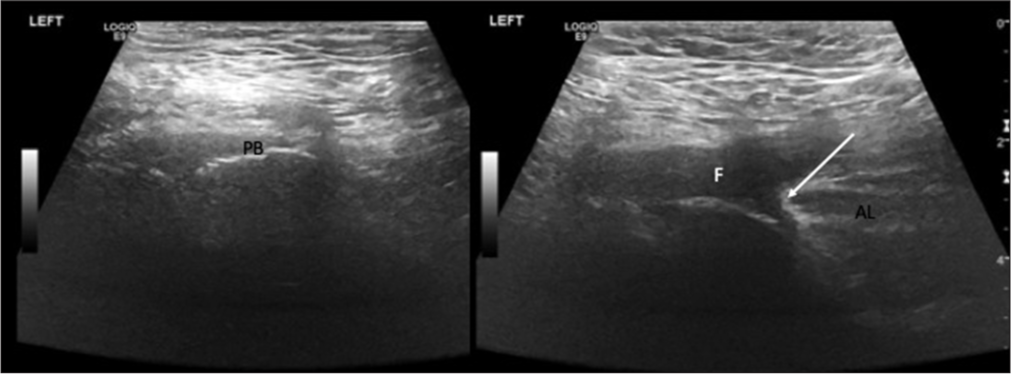
- Ultrasonography in a 52-year-old male with sports related groin injury showing adductor longus (AL) tendinous avulsion. A retracted AL tendon stump (white arrow) located at the proximal insertion near the pubic bone (PB) associated with a fluid (F) collection (sero-hematoma).
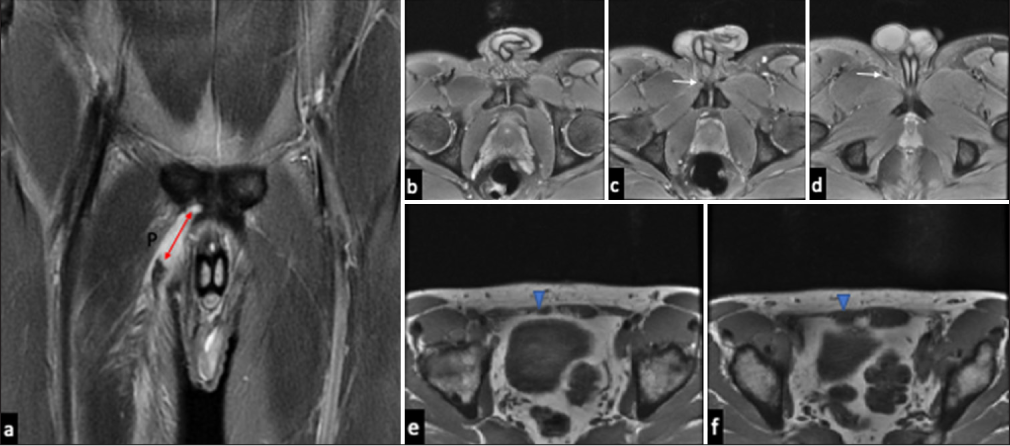
- (a) Coronal oblique images in a 22-year-old cricketer demonstrate a full-thickness tear of the right adductor longus tendon from its origin (double headed red arrow), with 5 cm retraction and intramuscular tear at the medial fibers of pectineus (P). (b-d) Serial axial images show diminished asymmetrical tendon size with peritendinous free fluid (white arrows). (e and f) Noteworthy asymmetric atrophy (blue arrowheads) of the right rectus abdominis muscle (lateral head more than the medial head) on T1-weighted axial images lends evidence to the predictable unsupported/unopposed force vectors at the pubis.
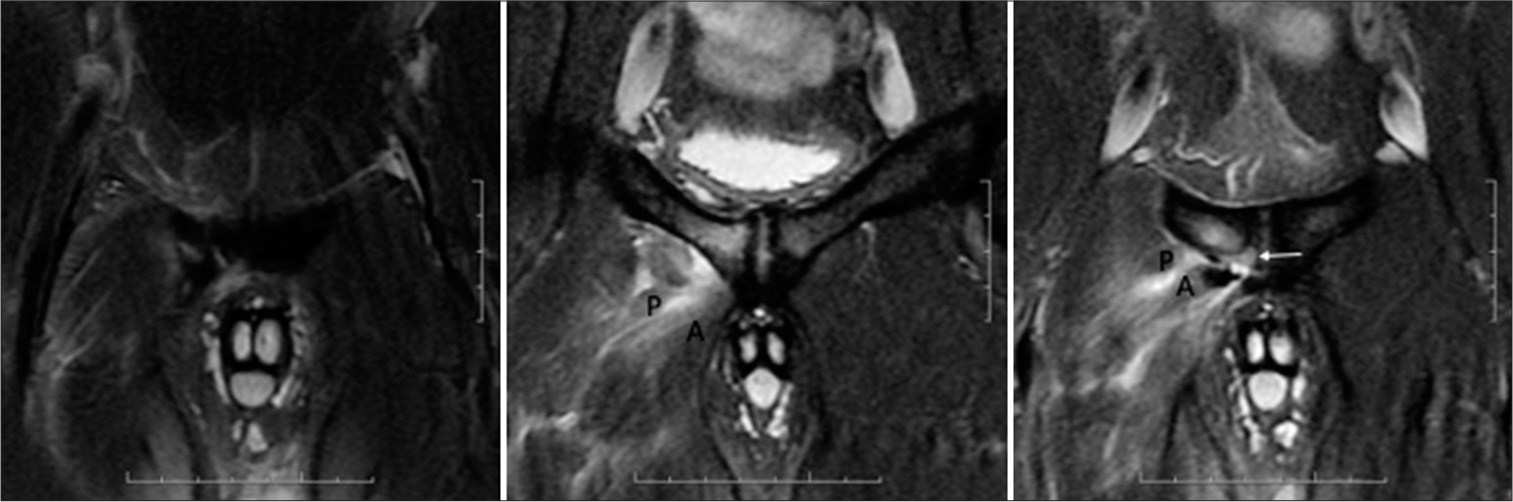
- 32-year-old footballer with acute groin pain. Coronal T2 fat-suppressed magnetic resonance images reveal full thickness tear of the right adductor longus (A) and pectineus (P) origins with bony avulsion (white arrow) at the pubis.
An exceedingly challenging pathology arises when a distal myotendinous junction injury leads to the rupture of the muscular sheath and subsequent herniation of muscle fibers through the resulting defect, resulting in a muscle strain resistant to conventional conservative treatment. This condition is termed “Hockey Goalie–Baseball Pitcher Syndrome.” At present, no specific MRI findings have been definitively established for this syndrome. However, akin to other myofascial herniations observed elsewhere in the body, typical imaging manifestations include edema within the AL muscle belly at the site of herniation and a small muscular protrusion indicative of the herniated tissue. Surgical debridement becomes necessary for the management of refractory pain.[2]
Rectus abdominis strain
While the rectus abdominis muscle may experience strain along its course akin to other abdominal muscles, it is commonly afflicted in the mid to lower abdomen, often in conjunction with the external or internal oblique muscles. This strain presents as a feathery hyperintensity on fluid-sensitive sequences during MRI, with the hyperintensity aligning along the muscle belly. Although isolated occurrences are rare, rectus abdominis strain typically denotes an injury involving the rectus abdominis-adductor aponeurosis. Vigilant examination of the tenoperiosteal distal rectus attachment is imperative in this context, as isolated muscle injuries generally resolve with conservative management; however, aponeurotic injuries may lead to chronic pain and pelvic instability if not addressed appropriately.[1] Rectus abdominis atrophy is often encountered in sports related groin pain and may be a representation of long-standing tendinous lesion, previous strain, or secondary to denervation injury[1] [Figure 16].
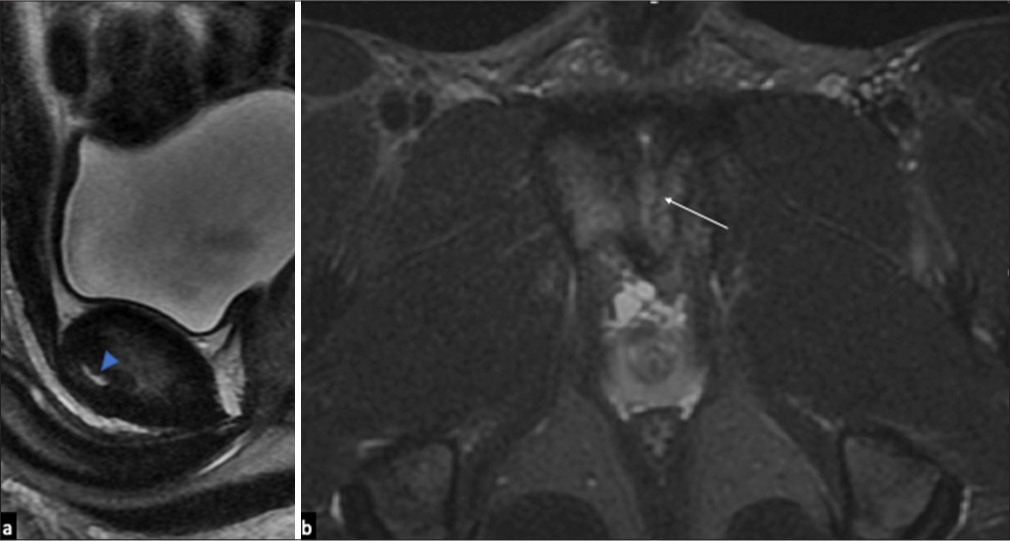
Pyramidalis–anterior pubic ligament AL complex (PLAC) injuries
Numerous studies have revealed that avulsion of the proximal adductor tendon seldom occurs in isolation but frequently entails injuries to the proximal AL complex (PLAC) and frequently the pectineus muscle. Research indicates a heightened occurrence of injuries to the anterior pubic ligament spanning the symphysis pubis in cases of partial avulsion of the pectineus. Moreover, there is increased displacement of AL FC in instances of partial or complete separation between the AL and the pyramidalis muscle. This displacement is further exacerbated with an associated injury to the pectineus, rendering the injury more significant and necessitating a more intricate surgical approach to address each injured component. A comprehensive understanding of the anatomy and corresponding imaging findings is imperative for accurate diagnosis of these intricate injuries and consequently guiding appropriate treatment modalities. Six different kinds of PLAC injury have been identified on MRI based on the status of the AL FC, the pyramidalis and pectineus muscles and tendons [Table 2 and Figure 18].[29]
| Type 1 | Complete avulsion of FC-separation of pyramidalis from AL-pectineus intact |
| Type 2 | Complete avulsion of FC-separation of pyramidalis from AL-pectineus partially torn |
| Type 3 | Complete avulsion of FC-pyramidalis attached to AL-pectineus intact |
| Type 4 | Complete avulsion of FC-pyramidalis attached to AL-pectineus partially torn |
| Type 5 | Complete avulsion of FC-partial separation of pyramidalis from AL-pectineus partially torn |
| Type 6 | Partial avulsion of FC-pyramidalis attached to AL-pectineus intact |
MR: Magnetic resonance, AL: Adductor longus, FC: Fibrocartilage
- Coronal and sagittal T2 fat-suppressed serial magnetic resonance images showing complete avulsion of adductor longus fibrocartilage (white arrow), partial tear of the pectineus (P), and intact pyramidalis (blue arrowhead) representing type 4 pubic bone and adductor longus complex injury.
Inguinal hernias
Inguinal hernias are accountable for 24–51% of cases of sports-related athletic groin pain. Acquired inguinal wall deficiency results from overuse, occurring in nearly 15% of athletes having groin pain, and is essentially traumatic attenuation and weakening of the inguinal canal which is not sufficient in severity to form a discrete hernia. Anterior inguinal wall deficiency, traditionally known as the “Gilmore groin” results from degeneration and partial tear of the external oblique aponeurosis, ending up in dehiscence between the inguinal ligament and eventually causing superficial inguinal ring dilatation. As the posterior inguinal wall is attached over the anterior rectus sheath, posterior inguinal wall deficiency is frequently seen in relation with abnormalities of the rectus abdominis. Dynamic MRI reveals asymmetric focal protrusion of the inguinal wall without herniation in comparison to the contralateral side. The benefit of MRI is that it permits direct visual comparison with the contralateral side [Figure 19].[6]

- T1-weighted axial magnetic resonance images revealing atrophy of the right rectus abdominis muscle (blue arrowhead) and presence of ipsilateral inguinal hernia (white arrow demonstrating the hernial sac).
It has been observed that, in athletes, direct inguinal hernia and femoral hernia are more frequent. Conventionally, clinicians have depended upon physical examination for detecting hernias. However, when there is inguinal region pain and indeterminate physical examination findings, USG/MRI come into play. Both USG and MRI are effective in depicting the hernial sac well. Imaging can also help distinguish between possible etiologies for a palpable inguinal region abnormality.[2]
Referred pain
Pain may be referred to groin from other regions, for instance compression of upper lumbar nerves, [Figure 1] hence, further imaging may be required if no local abnormality is evident. Abnormalities in the hip may also contribute to groin pain, as in premature osteoarthritis, acetabular labral tears, femoroacetabular impingement, stress fractures [Figure 20], and intra-articular loose bodies. Tears and tendinosis of the muscles nearby, such as sartorius, rectus femoris, tensor fascia lata, iliopsoas tendinitis, and bursitis, may manifest primarily as groin pain [Figure 21]. For this reason, some athletes with groin pain can present for imaging of the groin and hip.[6]
- Plain radiographs in a 33-year-old soccer player with recent onset right groin region pain showing stress fracture of the right inferior pubic ramus (white arrow). Subsequent magnetic resonance (Coronal T2 fatsuppressed) images in the same player revealed an additional stress fracture of the right superior pubic ramus (red arrowhead) as well with surrounding bone marrow and soft-tissue edema.
- Axial T2-weighted fat-suppressed magnetic resonance images in a 21-year-old mail with groin pain showing traumatic iliopsoas tendinitis (*) and iliopsoas bursitis (white arrow).
Sports groin in women
Many studies have consistently identified a notably higher prevalence of groin injuries among males compared to females. This gender discrepancy may potentially be attributed to anatomical distinctions in the male and female pelvis. The broader pelvic structure in females results in a more oblique angle for the action of the short adductor muscles, thereby diminishing the tractional force exerted at their origins and consequently reducing the occurrence of insertional muscle tears in females. In addition, it has been noted that cam-type morphology of the femoral head-neck junction occurs more frequently in males, predisposing male athletes to labral injuries, which commonly present as groin pain.[7]
Although sports-related groin injuries are uncommon in females, aponeurotic injuries in females generally exhibit greater severity compared to those in males. While aponeurotic injuries in many male athletes are typically unilateral, in female athletes, they frequently originate in the midline and extend bilaterally.[2]
CONCLUSION
The significance of imaging, specifically MRI in the clinical evaluation of sports-related groin pain, is underscored by the radiologist’s proficiency in recognizing injury patterns in the anatomical structures surrounding the symphysis pubis. Utilizing unenhanced MRI with a tailored protocol for groin assessment enables the detection of subtle abnormalities, identification of involved structures, and evaluation of injury extent in patients presenting with sports-related groin pain. The endorsed MRI protocol for assessing potential sources of referred groin pain encompasses both small FOV high-resolution scans targeting the symphysis pubis and large FOV pelvic surveys. A thorough understanding of typical clinical and imaging findings associated with various injuries empowers the radiologist to accurately identify the pathologic process and guide the referring clinician toward an appropriate management strategy.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- The spectrum of MR imaging in athletic pubalgia. Radiol Clin North Am. 2010;48:1179-97.
- [CrossRef] [PubMed] [Google Scholar]
- Athletic pubalgia and “sports hernia”: Optimal MR imaging technique and findings. Radiographics. 2008;28:1415-38.
- [CrossRef] [PubMed] [Google Scholar]
- The avoidability of soccer injuries. Int J Sports Med. 1983;4:124-8.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence and differential diagnosis of acute groin injuries in male soccer players. Scand J Med Sci Sports. 1999;9:98-103.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for groin injuries in hockey. Med Sci Sports Exerc. 2001;33:1423-33.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging review of groin pain in elite athletes: An anatomic approach to imaging findings. Am J Roentgenol. 2008;191:962-72.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of groin pain in athletes: Patterns of injury at MRI and gender differences therein. Irish J Med Sci. 2023;192:1411-8.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of sports-related hip and groin injuries. Sports Health. 2010;2:252-61.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of groin pain. Magn Reson Imaging Clin. 2009;17:655-66.
- [CrossRef] [PubMed] [Google Scholar]
- The pyramidalis-anterior pubic ligament-adductor longus complex (PLAC) and its role with adductor injuries: A new anatomical concept. Knee Surg Sports Traumatol Arthrosc. 2017;25:3969-77.
- [CrossRef] [PubMed] [Google Scholar]
- The topography and morphometrics of the pubic ligaments. Ann Anat. 2021;236:151698.
- [CrossRef] [PubMed] [Google Scholar]
- The adult symphysis pubis: Normal and abnormal. Am J Roentgenol Radium Ther Nucl Med. 1971;112:517-25.
- [CrossRef] [PubMed] [Google Scholar]
- The symphysis pubis: Anatomic and pathologic considerations. Clin Orthop Relat Res. 1983;203:261-72.
- [CrossRef] [Google Scholar]
- Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247:797-807.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy, pathology, and MRI findings in the sports hernia. Semin Musculoskelet Radiol. 2008;12:54-61.
- [CrossRef] [PubMed] [Google Scholar]
- Patterns of bone and soft-tissue injury at the symphysis pubis in soccer players: Observations at MRI. AJR Am J Roentgenol. 2007;188:W291-6.
- [CrossRef] [PubMed] [Google Scholar]
- Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med. 2015;49:768-74.
- [CrossRef] [Google Scholar]
- Secondary cleft sign as a marker of injury in athletes with groin pain: MR image appearance and interpretation. Radiology. 2005;235:162-7.
- [CrossRef] [PubMed] [Google Scholar]
- Adductor-related groin pain in athletes: Correlation of MR imaging with clinical findings. Skeletal Radiol. 2004;33:451-7.
- [CrossRef] [PubMed] [Google Scholar]
- Symphyseal cleft injection in the diagnosis and treatment of osteitis pubis in athletes. AJR Am J Roentgenol. 2002;179:955-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diseases of pubis and pubic symphysis. MR imaging appearance. AJR Am J Roentgenol. 1997;169:849-53.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance findings of osteitis pubis. J Magn Reson Imaging. 2007;25:535-9.
- [CrossRef] [PubMed] [Google Scholar]
- Osteitis pubis syndrome in the professional soccer athlete: A case report. J Athl Train. 2001;36:437-40.
- [Google Scholar]
- Chronic groin injuries in athletes: Recommendations for treatment and rehabilitation. Sports Med. 1994;17:141-8.
- [CrossRef] [PubMed] [Google Scholar]
- The pubic bone-adductor-syndrome in football players [in German] Zentralbl Chir. 1967;92:2656-60.
- [Google Scholar]
- Proximal adductor avulsions are rarely isolated but usually involve injury to the PLAC and pectineus: Descriptive MRI findings in 145 athletes. Knee Surg Sports Traumatol Arthrosc. 2021;29:2424-36.
- [CrossRef] [PubMed] [Google Scholar]







