Translate this page into:
Role of computed tomography in glenohumeral joint deformity following obstetric brachial plexus injury: Proposed radiological classification

*Corresponding author: Joel Kevin Raj Samuel, Department of Radiodiagnosis, Stanley Medical College, Chennai, Tamil Nadu, India. joelkraj@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chellathurai A, Damodasamy K, Raju B, Samuel J, Ganesan S. Role of computed tomography in glenohumeral joint deformity following obstetric brachial plexus injury: Proposed radiological classification. Indian J Musculoskelet Radiol 2023;5:18-24.
Abstract
Objective:
The study aimed to study the usefulness of computed tomography (CT) in the measurement of glenoid version angle, humeral head dislocation, or subluxation and to propose a grading system for the severity of glenohumeral deformity following OBPI.
Material and Methods:
A prospective study conducted over a period of 3 years. The study group includes 21 children below the age of 12 years presenting with posterior dislocation of the shoulder, with prior history of OBPI. CT of both shoulders was done using a 128-slice CT scanner. The children were assessed clinically by a Modified Mallet Scale and graded by Waters classification.
Results:
We graded the severity of deformity on the affected side according to Waters et al. The difference between affected and normal shoulder glenoscapular angle (GSA), percentage of humeral head anterior to the scapular line (PHH), scapular height, and scapular width was statistically significant (P < 0.05). We propose grading for severity and assessed joint stability based on the CT parameters. GSA and PHH show a statistically significant difference between the three grades (P < 0.05). We also confirm that the higher the grade of the deformity, the more difficult the shoulder movements leading to worse scores on the Modified Mallet Scale.
Conclusion:
CT scan identifies glenohumeral deformities such as increased glenoid retroversion, posterior dislocation of the humeral head, smaller humeral head size, and smaller size of the scapula as deviations from normal status and helps in radiological grading.
Keywords
Obstetric brachial plexus injury
Glenoid retroversion
Glenohumeral dysplasia
Glenoscapular angle
INTRODUCTION
Obstetric brachial plexus palsy/obstetric brachial plexus injury (OBPP/OBPI) is flaccid paralysis of the arm, which occurs at birth.[1] The reported incidence ranges from 0.15 to 3/1000 live births.[2,3] The injury usually involves traction of the nerve roots C5 and C6, which results in weakness of shoulder functions and elbow flexion, with the arm adducted and internally rotated. If severe, C7, C8, and T1 roots are also affected, resulting in a claw hand, vasomotor disturbance, and Horner’s syndrome.[4-7] In the long-term, these lead to osseous deformity such as a non-spherical humeral head or an abnormal glenoid.[8]
Abnormalities such as scapular hypoplasia, elevation, and rotation are found in the developing glenohumeral joint and the scapula, affected by OBPI.[4,8,9] The paralysis of the abductors and internal rotators progressively causes the developing arm to be fixed in medial rotation, with the resulting muscular imbalance causing posterior subluxation of the humeral head. These changes cause impaired scapular growth and glenohumeral development. In the literature, the affected scapulae were hypoplastic by an average of 14%. The glenoid version and percentage of the humeral head anterior to the scapular line (PHH) were significantly different between the involved and uninvolved shoulders.[10] There was a restricted range of movements in the affected shoulder.[11] Sibinski et al.[12] showed that the side affected by OBPI had glenoid retroversion, smaller humeral head size, posterior subluxation or dislocation of the humeral head, and glenohumeral joint incongruity as compared to the normal side.
The role of this study is an early demonstration of deformity using computed tomography (CT) for initiation of the appropriate management. We propose a classification using CT measurements such as glenoid version angle and humeral head dislocation for grading the severity of the glenohumeral deformity.
MATERIAL AND METHODS
The Institutional Ethical Committee approval was obtained before commencing this study. It was a prospective study conducted in our institute between 2014 and 2017. The study group consisted of 21 children below the age of 12 years (pediatric population) with posterior dislocation of the shoulder, who were referred to our institute for imaging studies. The children with a history of OBPI were included and patients with post-surgical changes, anterior shoulder dislocation, primary glenoid dysplasia, postnatal traumatic brachial plexus injury, and patients with surgical clips and contraindications for magnetic resonance imaging (MRI) were excluded from the study.
The procedure was explained to the parents and a detailed antenatal and perinatal history, mode of delivery, and instrumentation during labor were elicited. The presence of fracture or nerve palsy at birth was recorded.
Functional evaluation was done with a modified Mallet score[13] which included the following movements – Global abduction, global external rotation, hand to the neck, hand on spine, hand to mouth, and internal rotation. Each movement was awarded a score of 1–5 for six clinical parameters. A score of 1 indicated a total lack of function and a score of 5 indicated a normal function.
Clinical data were collected from all patients. Multi-slice CT imaging was performed using a GE Optima 128-slice scanner (GE Healthcare, USA). The patient was positioned supine with an arm by the side of the body. The field of view included both shoulders and scapulae. 0.6 mm thin helical sections were obtained. Volume rendering and reformatted images were obtained. The parameters were measured from the above images. Protective shielding of areas outside the field of view, low mA, and iterative reconstruction technique were used, so that dose to the child was reduced to a minimum. Further analysis of CT images was done in a GE workstation after transferring the acquired data. The following measurements were derived from the volume rendered and axial images of the study: Glenoscapular angle (GSA), PHH, scapular height (SH), and scapular width (SW).
GSA was measured as described in Nath et al.[9,13] Axial CT image at the mid-glenoid level was used. The scapular line was drawn from the medial aspect of the scapula to the midglenoid point. At this level, another line was constructed connecting the anterior and posterior glenoid labrum, intersecting the scapular line. The posteromedial angle between the two lines was measured and 90° was subtracted from the above-measured angle to get the glenoid version angle or GSA. At the same level as the GSA, the scapular line is extended laterally to pass through the humeral head. Another line passing through the greatest diameter of the humeral head is drawn perpendicular to the scapular line. The percentage of the length of the head anterior to the scapular line to the greatest diameter of the humeral head gives the PHH [Figure 1].

- Diagrammatic representation of glenoid version angle and percentage of humeral head measurement.
The height and width of the scapula were measured in the volume-rendered CT images [Figure 2]. The height of the scapula was measured in the posterior oblique scapular view. The distance from the superior angle to the inferior angle in the medial border of the scapula was measured. The width of the scapula was measured in the posterior view of the virtual reality images. The distance from the mid-glenoid level to the medial most aspect of the scapula was measured.[12]
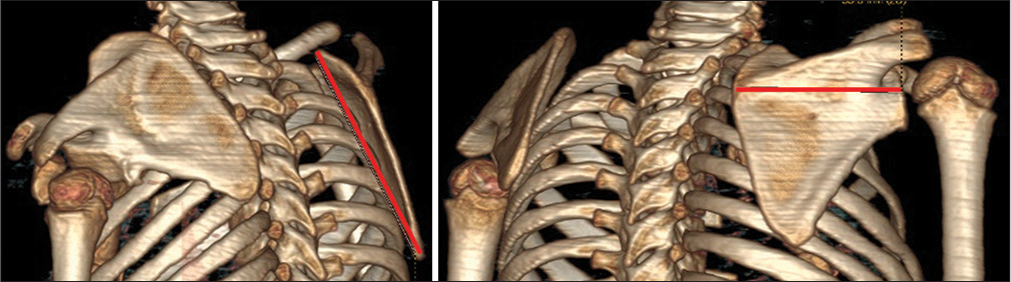
- Diagrammatic representation of scapular height and scapular width measurement.
RESULTS
We evaluated 21 children under 10 years of age, consisting of nine boys and 12 girls. The left shoulder was affected predominantly involving 13 children. There were predisposing antenatal and perinatal histories such as breech delivery, fetal macrosomia, maternal diabetes, the prolonged second stage of labor, and instrumental delivery in 16 children. The rest of the children presented with OBPI even without any predisposing factor. In our study, 20 children were born by normal delivery. However, one baby was delivered by cesarean section. Andersen et al.[1] in his study has also described that the above-mentioned causes and shoulder dystocia are the etiologies that can result in Brachial plexus birth injury. The images were analyzed by two radiologists.
The children were divided into three groups based on the age of appearance of proximal humeral epiphyses. Group I was children younger than 1 year (five subjects), Group II was children between 1 and 5 years (10 subjects), and Group III was children older than 5 years (six subjects). The degree of affection was compared among the three groups.
The GSA, PHH, SH, and SW were analyzed by parametric paired Student’s-t-test. These parameters were statistically significant measures (P < 0.05) in assessing the presence of glenohumeral deformity and grading it [Figure 3]. Comparison of the SH to width ratio on both sides by parametric paired Student’s-t-test showed that the difference on both sides was not significant. The mean measured values and statistical analysis are shown in [Table 1].
![Computed tomography axial images of a 5-year child with the left obstetric brachial plexus injury. (a) Percentage of humeral head anterior to the scapular line (PHH) in normal side [right]. (b) PHH in affected side [left] showing posterior shoulder dislocation. (c) Glenoscapular angle (GSA) in normal side [right] 1.4° retroversion. (d) GSA in affected side [left] showing increased glenoid retroversion of 43.5°.](/content/107/2023/5/1/img/IJMSR-5-018-g003.png)
- Computed tomography axial images of a 5-year child with the left obstetric brachial plexus injury. (a) Percentage of humeral head anterior to the scapular line (PHH) in normal side [right]. (b) PHH in affected side [left] showing posterior shoulder dislocation. (c) Glenoscapular angle (GSA) in normal side [right] 1.4° retroversion. (d) GSA in affected side [left] showing increased glenoid retroversion of 43.5°.
| Parameter | Normal joint | Affected joint | P-value |
|---|---|---|---|
| Range GSA | −5.19±9.27° | −34.5±35.4° | <0.05 |
| Range PHH | 47.24±6.2% | 13.24±26.58% | <0.05 |
| Range SH | 71.95±32.03 mm | 66.86±30.5 | <0.05 |
| Range SW | 52.57±29.3 mm | 48.48±29.2 mm | <0.05 |
| Range SH: SW | 1.39±0.14 | 1.41±0.16 | |
| Mean SH ratio between affected and normal side was 0.92±0.06 | |||
| Mean SW ratio between affected and normal side was 0.91±0.44 | |||
CT: Computed tomography, GSA: Glenoscapular angle, PHH: Percentage of humeral head anterior to the scapular line, SH: Scapular height, SW: Scapular width
| Nath and Paizi | Sibinski et al. | Our study | |
|---|---|---|---|
| Study population | 30 | 24 | 21 |
| Age group | 10 months–10.6 years | 3–12 years | 6 months–10 years |
| Sex | 10 boys | 8 boys | 12 boys |
| 20 girls | 16 girls | 9 girls | |
| Affected side | 10 left | 13 left | |
| 14 right | 8 right | ||
| GSA (°retroversion) | Normal joint 2.9° | Normal joint 4.5° Affected | Normal joint 5.19° |
| Affected joint 20.4° | joint 23.3° | Affected joint 34.5° | |
| PHH (percentage) | Normal joint 49.0% | Beyond the scope of the study | Normal joint 47.24% |
| Affected joint 25.7% | Affected joint 13.2% | ||
| Mean affected to normal SH ratio | 0.89 | Beyond the scope of the study | 0.92 |
| Mean affected to normal SW ratio | 0.95 | Beyond the scope of the study | 0.91 |
GSA: Glenoscapular angle, PHH: Percentage of humeral head anterior to the scapular line, SH: Scapular height, SW: Scapular width
The SH and width were also reduced significantly on the affected side when compared to the normal side. There was no significant difference in the SH: SW ratio on both side. These findings show that the scapula was hypoplastic on the affected side.
The mean value of GSA and PHH in each group was comparable (almost equal) implying that the grade of affection of the angle was in extreme ranges in all the groups which is shown in [Table 3].
| Group | GSA (Retroversion in degree) | PHH (Percentage) | SH (mm) | SW (mm) | ||||
|---|---|---|---|---|---|---|---|---|
| Affected | Normal | Affected | Normal | Affected | Normal | Affected | Normal | |
| I | −33.5 | −5.92 | 16.06 | 45.68 | 47.8 | 52.4 | 30 | 34.2 |
| II | −32.09 | −4.95 | 12.9 | 47.44 | 66.2 | 71.2 | 47 | 51.1 |
| III | −39.5 | −4.8 | 11.2 | 48.3 | 83.83 | 89.5 | 66.33 | 70.33 |
CT: Computed tomography, GSA: Glenoscapular angle, PHH: Percentage of humeral head anterior to the scapular line, SH: Scapular height, SW: Scapular width
DISCUSSION
Brachial plexus injury leads to long-term morbidity by causing muscle imbalances and weakness around the shoulder (the deltoid and external shoulder rotators), and relative dominance of already strong internal rotators, which may progress to a fixed medial rotation position of the humerus. This constant position of the shoulder has a deleterious effect on glenohumeral development and results in bony deformities at the shoulder joint (glenohumeral dysplasia and joint incongruity) [Figure 4]. This is evidenced by decreased PHH in the affected joint. There is increased glenoid retroversion evidenced by decreased GSA on the affected side. This change is seen in varying severity in all study subjects.
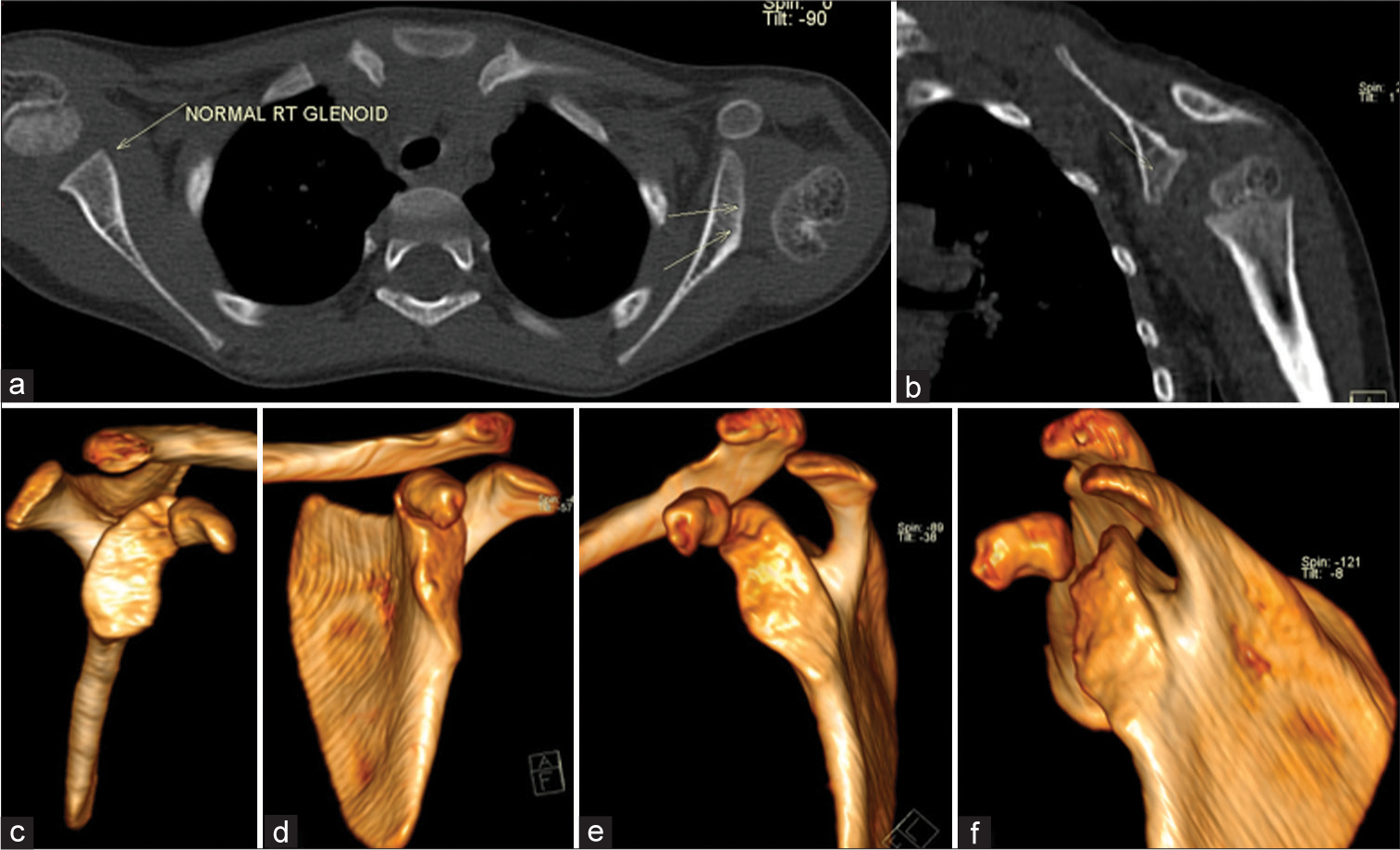
- (a) Computed tomography axial image showing normal right glenoid, retroverted and dysplastic left glenoid with posterior dislocation of humeral head. (b) Coronal reformatted image showing retroverted glenoid. (c) Virtual reality (VR) image showing normal right glenoid cavity. (df) VR image showing retroverted glenoid with false glenoid cavity formation in the inferior aspect of anatomic glenoid.
Nath and Paizi[9] in his study also evaluated the CT parameters of the scapula and compared the affected and normal sides. The mean GSA on the affected side was −20.4 ± 11.34° and the normal side was −2.9 ± 3.74°. The mean percentage subluxation of the humeral head on the affected side was 25.7 ± 20.75%, the normal side was 49.0 ± 3.5%. The mean affected to contralateral SH ratio was 0.89 ± 0.10 and the mean affected to contralateral SW ratio was 0.95 ± 0.07. There was no statistically significant difference in the scapular length-to-width ratio on both sides in their study also, showing that the scapula was hypoplastic on the affected side. Sibinski et al.[12] in their study showed the GSA in non-affected joints was 4.5° and in affected joints was 23.3° retroversion. The parameter in our study and the above two studies were in correlation with each other, but the differences in the mean GSA and PHH is because the severity of the deformity was more in our study group [Table 2].
This study shows that there are significant differences in the GSA and PHH between the affected shoulder and contralateral shoulder in all children. A child with an age of 22 months had hypoplastic humeral head epiphysis and absent epiphysis for greater tuberosity in the affected shoulder while the epiphysis had appeared in the contralateral side [Figure 5a]. The age of the youngest child was 6 months and the child had posterior dislocation of the humeral head with the hypoplastic posterior aspect of the glenoid [Figure 5b].
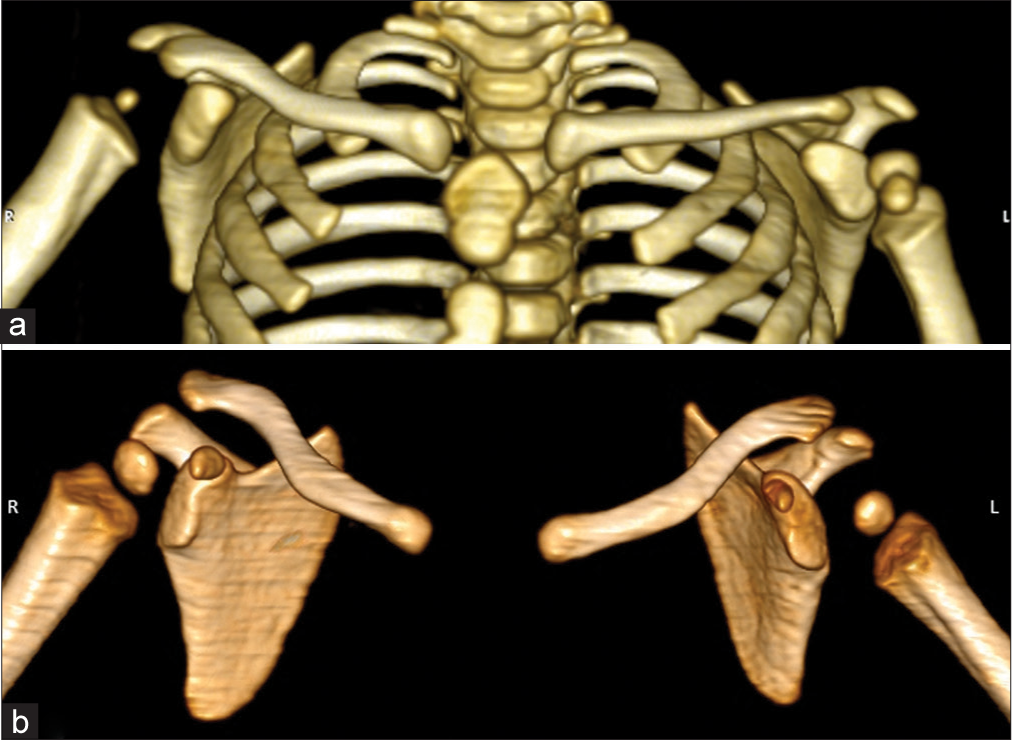
- Computed tomography virtual reality images. (a) Child with the right obstetric brachial plexus injury (OBPI) with hypoplastic right humeral head, absent greater tuberosity epiphysis and retroverted right glenoid cavity. (b) Child with the left OBPI with hypoplastic and retroverted left glenoid cavity.
Waters and Peljovich[14] had classified glenohumeral deformities (Type I–VII) caused by OBPI as shown in [Table 4].
| Grading | Type | Description | No. of subjects |
|---|---|---|---|
| I | Normal glenoid | <5° difference in retroversion compared with that on the normal, contralateral side | 1 |
| II | Minimum deformity | More than a 5° difference in retroversion compared with that on the normal side, with no posterior subluxation of the humeral head |
3 |
| III | Moderate deformity | Posterior subluxation of the humeral head, defined as <35% of the head anterior to the bisecting line |
7 |
| IV | Severe deformity | A false glenoid | 3 |
| V | Severe deformity | Severe flattening of the humeral head and glenoid, with progressive or complete posterior dislocation of the head |
5 |
| VI | Severe deformity | Dislocation of the glenohumeral joint in infancy | 1 |
| VII | Severe deformity | Growth arrest of the proximal aspect of the humerus | 1 |
It was evident from our study that the Modified Mallet score was lower for higher grades of deformity [Table 5], showing that higher grades of deformity are associated with restriction of movements. Sibiński et al. in his study[11] observed that the most common problem found in 60% of children was a limitation of active external rotation of the shoulder. One-fourth of patients had posterior dislocation or subluxation in the glenohumeral joint.[11]
| Joint stability (as per our study) |
Criteria | Number of subjects |
Waters et al. grade |
Mean modified mallet score |
Treatment plan |
|---|---|---|---|---|---|
| Normal (grade 0) | <5° difference in retroversion compared with that on the normal |
0 | I | ||
| Stable Joint (grade I) | More than a 5° difference in retroversion compared with that on the normal side, with no posterior subluxation of the humeral head |
3 | II | 18 | Tendon transfer |
| Subluxation (grade II) | Posterior subluxation of the humeral head, defined as <35% of the head anterior to the bisecting line |
9 | III | 13.56 | Contracture release and tendon transfer |
| Dislocation (grade III) | A false glenoid, complete posterior dislocation of the head, flattening of humeral head |
9 | IV, V, VI, VII | 9.33 | Osteotomy, arthrodesis |
CT: computed tomography
Analysis showed that the severity of deformity was independent of age as shown in [Figure 6]. Sibinski et al.[12] in his study also found that there was no correlation between the degree of dislocation and the age of the patient. de Souza Silva et al.[13] in his study demonstrated that there was a significant correlation between the physical examination and severe shoulder dysplasia in children under 24 months of age. Their study insisted on an early CT scan to assess the onset of deformity. In our study, the Group I subjects which consisted of infants had shoulder dislocation, this was in correlation with de Souza Silva et al.
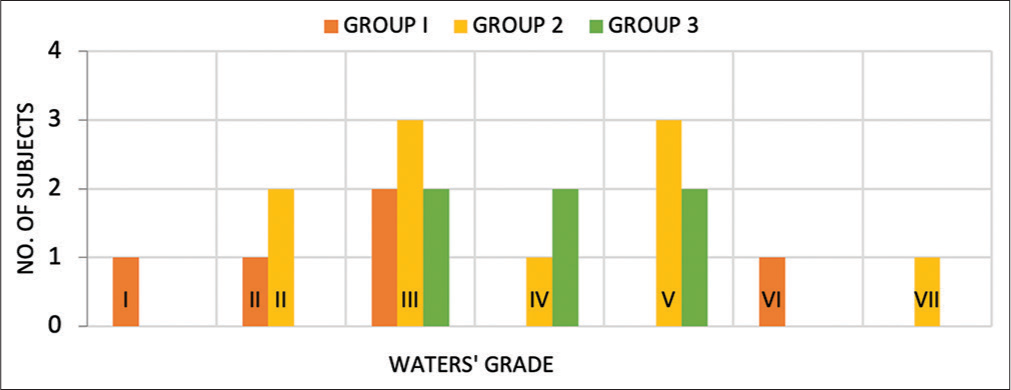
- Distribution of severity of deformity in three group of children across Waters et al. grade.
The present study showed that the higher the grade of deformity, the more difficult will be the active internal rotation and passive external rotation, with much worse scores on the Modified Mallet scale. It seems that this is an effect of highly disturbed muscular balance due to the lack of physical contact between the humeral head and the glenoid and because of the parallel deformation of articular surfaces.[15] Sibinski et al.[12] in his study showed that the more posterior dislocation, the worse the active internal rotation and passive external rotation. Hoeksma et al.[16] in their study have also found that there is a strong association between shoulder contracture and osseous deformity with OBPP.
Posterior joint dislocation or subluxation was observed in 18 of 20 patients. Decreased GSA and posterior dislocation or subluxation of the humeral head were the most obvious deformities among the shoulder joints examined. The humeral head and proximal end of the humerus were smaller compared to the normal side in all of the children with deformation of the humeral head.
As shown by the previous studies,[3] most patients with OBPI who begin to recover in the first 3 months of life can be expected to have improved to nearly normal function. Patients who have nerve injuries have to undergo nerve repair surgeries within the first 6 months. The patients who show delayed recovery fail to regain normal muscle power, resulting in deformity.
In our study, a CT scan was used instead of MRI as it can be more accurate in the assessment of bony deformities, takes lesser time for imaging with fewer patients needing sedation than MRI which consumes more time, needs sedation, and both sides cannot be assessed adequately in the same field of view. However, several glenohumeral morphologic features can be evaluated on axial MR images. First, the shape of the glenoid can be characterized in the Birch classification as concave-flat, convex, or biconcave. Evaluation for a pseudo glenoid, whereby the humeral head articulates with a retroverted posterior articular surface, is also possible. Finally, the GSA can also be calculated using MRI images.[17]
The treatment strategies[14,18] for these children were discussed with the treating surgeons. The concern in these children is the choice of procedure that is to be carried out. The choices that are currently available include microsurgical nerve reconstruction in infants and secondary reconstruction with tendon transfers or osteotomy. The children with Type I and II, with GSA < 20° were managed by tendon transfer. Most of the cases of Type III were managed by contracture release and latissimus dorsi and teres major muscle transfer to the insertion of the rotator cuff, as it may correct the muscle imbalance. Type IV patients would not benefit from muscle transfer alone, the role of osteotomy was also unclear in these cases. Type V–VII cases underwent deformity correction osteotomy and arthrodesis in a functional position as required.
Limitations
The study group was small due to the rarity of the condition. Earlier imaging and follow-up were not taken into account. Acute OBPI patients were not included in this study. A mild injury like neuropraxia could not be seen, as only children presenting to the hospital with subluxation were included in this study.
CONCLUSION
CT scan identifies glenohumeral bony deformities such as increased glenoid retroversion, posterior subluxation or dislocation of the humeral head, smaller humeral head size, and smaller size of the scapula as the deviations from normal status and aids in grading.
Declaration of patient consent
Institutional review board (IRB) permission was obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Perinatal brachial plexus palsy. Paediatr Child Health. 2006;11:93-100.
- [CrossRef] [PubMed] [Google Scholar]
- Obstetric brachial plexus injury. Indian J Plast Surg. 2011;44:380-9.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital brachial palsy: Incidence, causes, and outcome in the United Kingdom and Republic of Ireland. Arch Dis Child Fetal Neonatal Ed. 2003;88:F185-9.
- [CrossRef] [PubMed] [Google Scholar]
- Severe obstetric brachial plexus palsies can be identified at one month of age. PLoS One. 2011;6:e26193.
- [CrossRef] [PubMed] [Google Scholar]
- Brachial plexus birth injuries. An experimental study (author's transl) Chir Pediatr. 1979;20:159-63.
- [Google Scholar]
- Glenohumeral deformity in children with brachial plexus birth injuries. Bull NYU Hosp Jt Dis. 2011;69:36-43.
- [Google Scholar]
- Scapular deformity in obstetric brachial plexus palsy: A new finding. Surg Radiol Anat. 2007;29:133-40.
- [CrossRef] [PubMed] [Google Scholar]
- Upright MRI of glenohumeral dysplasia following obstetric brachial plexus injury. Magn Reson Imaging. 2007;25:1277-82.
- [CrossRef] [PubMed] [Google Scholar]
- Upper limb function in children with obstetric brachial plexus palsy. Chir Narzadow Ruchu Ortop Pol. 2010;75:5-9.
- [Google Scholar]
- Secondary gleno-humeral joint dysplasia in children with persistent obstetric brachial plexus palsy. Int Orthop. 2010;34:863-7.
- [CrossRef] [PubMed] [Google Scholar]
- Role of early shoulder tomography on the obstetric brachial plexus palsy. Acta Ortop Bras. 2015;23:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder reconstruction in patients with chronic brachial plexus birth palsy. A case control study. Clin Orthop Relat Res. 1999;364:144-52.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior dislocation of the shoulder associated with obstetric brachial plexus palsy. J Bone Joint Surg Br. 1989;71:764-6.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder contracture and osseous deformity in obstetrical brachial plexus injuries. J Bone Joint Surg Am. 2003;85:316-22.
- [CrossRef] [PubMed] [Google Scholar]
- Brachial plexus birth palsy: Multimodality imaging of spine and shoulder abnormalities in children. Am J Roentgenol. 2015;204:W199-206.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical Management of Obstetric Brachial Plexus Palsy Secondary Deformities. London: Intech Open; 2014:114.
- [CrossRef] [Google Scholar]






