Translate this page into:
Sarcomatous Transformation of Unicentric Calcaneal Epithelioid Hemangioendothelioma: A Case Report with Review of Literature

*Corresponding author: Garima Sharma, Department of Radiodiagnosis, All India Institute of Medical Sciences, Rishikesh - 249 203, Uttarakhand, India. garimasharmavns@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma G, Saxena S, Subbaih AV. Sarcomatous Transformation of Unicentric Calcaneal Epithelioid Hemangioendothelioma: A Case Report with Review of Literature. Indian J Musculoskelet Radiol 2020;2(1):77-81.
Abstract
Vascular origin tumors of bone are rare entities. Epithelioid hemangioendothelioma (EHE) is a rare tumor representing <1% of primary bone tumors and is considered a low to intermediate grade malignancy. Literature describes cases which were either a part of multicentric disease or were metastatic. In this study, we reported a case of a 23-year-old female with biopsy-proven EHE with prior history of resection, presenting with recurrence of disease. Radiographs showed a lytic lesion involving the left calceneum and other tarsal bones with extensive soft-tissue component. Magnetic resonance imaging revealed an ill-defined, enhancing, lobular, and lytic lesion with adjacent soft-tissues component. Computed tomography confirmed extensive destruction of the involved tarsal bones. EHE is treated with wide surgical excision and recurrence is rare; however, our case presented with recurrence as well as thoracic metastasis which posed a great clinical challenge. The patient was treated with below knee amputation and was given subsequent radiotherapy. The main aim of this study is to revisit the clinicopathological aspects as well as the spectral behavior of vascular bone tumors.
Keywords
Vascular tumors of bones
Calcaneal lesions
Hemangioendothelioma
Sarcomatous transformation
INTRODUCTION
Primary vascular tumors of bone are rare. These originate from endothelial cells of the vessels and include both benign and malignant entities. First described by Wells in 1921,[1,2] classification of these lesions has undergone several changes.[3] Hemangioma, epithelioid hemangioendothelioma (EHE), and angiosarcoma are few to quote. Wenger and Wold[1,2] in 2000 proposed a new classification system by considering these tumors as a part of spectrum and classified them into benign and malignant entities.
EHE is considered as tumors of low to intermediate malignant potential. The entity was named by Weiss and Enzinger in 1982.[4] All bones can be affected, however, 50% occur in long tubular bones of extremities. Multifocality is a frequent feature of this malignancy[5-7] and is observed in approximately 50–75% of cases. Although cases of unicentric EHE are reported out of which very few had distal extremity involvement,[8,9] recurrence and presence of thoracic metastasis are exceptional features. Histological features as well as immunohistochemical markers suggest spindling morphology which strongly supports the spectral nature of these entities.
CASE REPORT
Clinical Presentation
A 23-year-old female presented to the orthopedics department with ulceroproliferative growth over the left foot. The patient was a known case of EHE (proven through biopsy at an outside tertiary facility) left foot with a history of multiple resections and incomplete radiotherapy over the period of 2 years. The growth measured approximately 25 cm×10 cm over the plantar aspect extending up to dorsolateral aspect of the involved foot. Swelling of about 6 cm×3 cm was present over medial aspect of the left dorsal third leg, soft to firm in consistency, skin over swelling was not pinchable, fixed to underlying structures. No sensory loss was seen. Range of motion was reduced significantly.
Imaging features
Radiograph of the left ankle and foot (anteroposterior [Figure 1] and lateral [Figure 2]) showed a lytic expansile lesion involving the calcaneum, talus, cuboid, and lateral cuneiform reaching up to talocalcaneal and calcaneocuboid joints along with an large soft-tissue component.

- Radiograph of the left foot with ankle showing a large soft-tissue lesion with lytic expansile destruction of calceneum, talus, cuboid, and cuneiforms.

- Lateral radiograph of the left foot with ankle showing a large soft-tissue lesion epicentered at calcaneum with its lytic expansile destruction and associated soft-tissue component.
The patient also underwent non-enhanced computed tomography (CT) of the left foot with ankle which showed near-complete destruction of calcaneum with lytic destruction of talus, cuboid, and lateral cuneiform by a soft-tissue density mass lesion [Figure 3].

- Non-contrast-enhanced computed tomography ankle and foot showing an ill-defined lytic lesion involving the calceneum causing its complete destruction with cortical breach and associated large soft-tissue component. Lytic destruction of talus, cuboid, and lateral cuneiform is also seen.
Magnetic resonance imaging (MRI) of the left foot was done which revealed an ill-defined lobulated area showing hypointense signal on T1-weighted images [Figure 4] and hyperintense signal on T2/short-tau inversion recovery [Figure 5] images involving left calcaneum causing its near-complete replacement. Lytic destruction of talus, cuboid, and lateral cuneiform was also seen. There was significant invasion into surrounding soft tissue, reaching up to the planter surface of foot which skin breach along with splaying of flexor tendons. On post-contrast images, intense heterogeneous enhancement was seen [Figure 6].

- Sagittal T1-weighted image showing an ill-defined lobulated hypointense lesion epicentered in calcaneus with complete destruction of calceneum, talus, cuboid, and lateral cuneiform. Inferiorly, the lesion is reaching up to skin surface with splaying of flexor tendons.
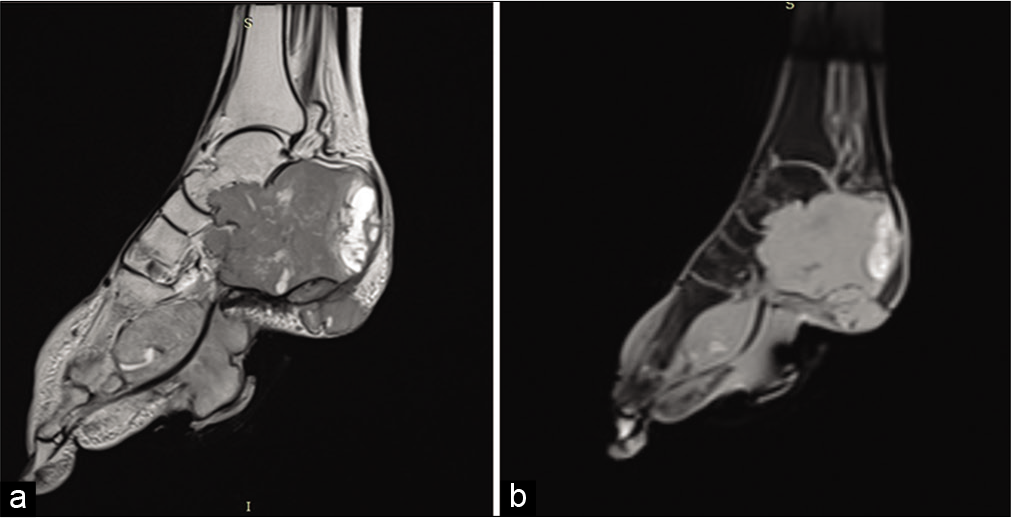
- Sagittal T2 (a) STIR (b) weighted images showing hyperintense signal in the lesion.
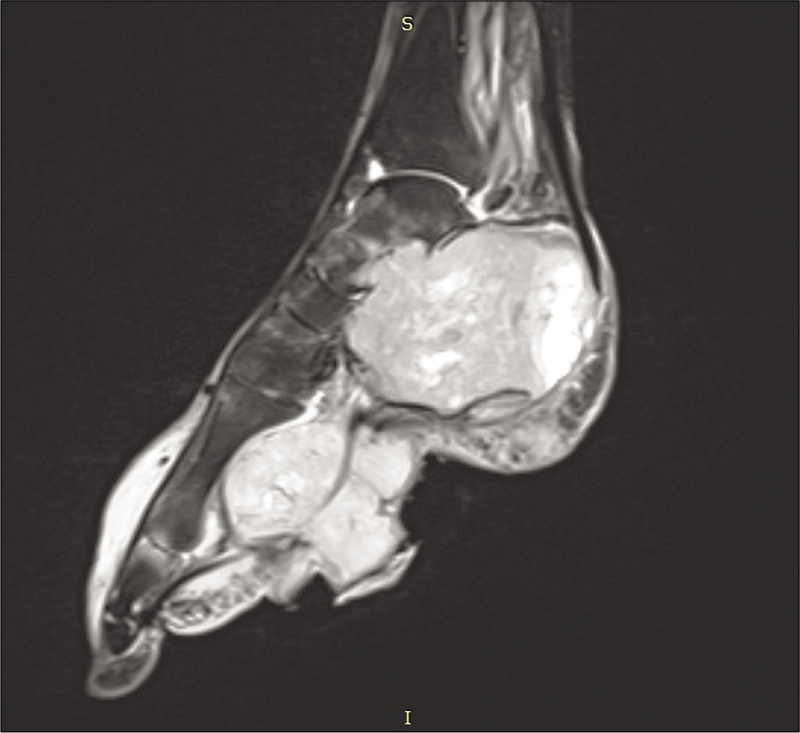
- Post-contrast T1-weighted sagittal image showing intense heterogeneous enhancement in the lesion.
High-resolution CT thorax was done as a part of metastatic workup which showed randomly distributed enhancing soft-tissue density nodules in bilateral lung parenchyma suggestive of metastasis [Figure 7a and b].
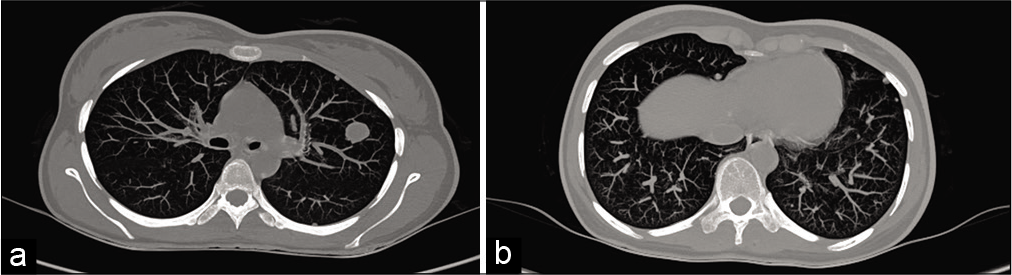
- (a and b) CT chest showing multiple randomly distributed soft-tissue nodules suggestive of metastasis.
Treatment
The patient underwent below knee amputation of the left leg. The resected limb was sent for histopathological assessment.
After proper physical rehabilitation, the patient was given radiotherapy. Histopathological examination of amputated limb show epithelioid cells in corded pattern within hyaline matrix. One region of the tumor distinctly showed spindle cell pattern. Immunohistochemistry was positive for CD34, CD31, CD99, TLE 1, and S 100 [Figure 8].
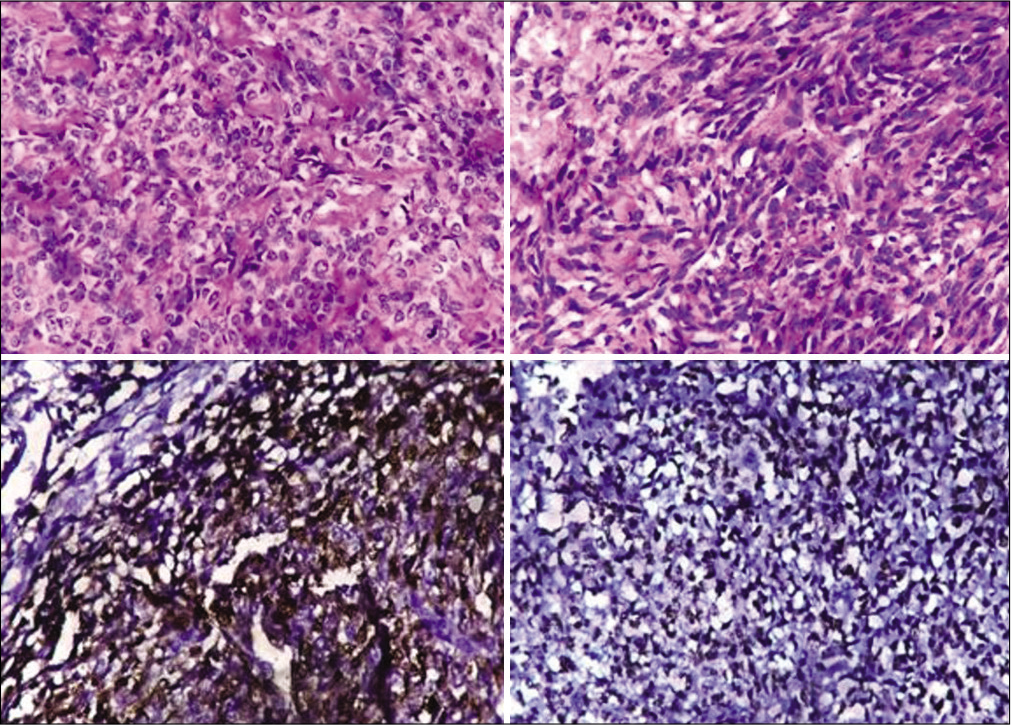
- Histological assessment (×200) showing large epithelioid and spindle cells arranged in cords, clusters, and as single cells within a myxoid to hyalinized stroma. Immunohistochemistry shows positivity to S-100 and CD99.
Several diagnostic challenges were present in this peculiar case. Unicentric lesion with recurrence on imaging as well as features such as spindle cell morphology and positivity of markers such as TLE-1 and S-100 on histopathology leads to a diagnostic dilemma. Initially, radiation-induced osteosarcoma as well as synovial cell sarcoma of talus was considered as a possibility, however, given the previous surgical history, sarcomatous transformation was dwelled upon.
DISCUSSION
Primary vascular tumors are rare entities with diverse clinical and radiological features. Wenger and Wold[2] suggested a nomenclature for these tumors and classified them as low- grade (hemangioendothelioma), high-grade (angiosarcoma and epithelioid angiosarcoma), and histologically distinct (EHE) endothelial malignancies.
EHE is low to intermediate grade malignant tumors. One of the characteristic features of these tumors is the tendency to develop multicentric disease.[5-7] Multiple lesions can develop in a single bone or involve multiple bones with lesions randomly distributed throughout the skeleton or clustered in an anatomic region, such as a single extremity. The majority of EHE cases of the bone occur in the lower extremities followed by the spine. The most common locations in the lower extremity for EHE to occur in descending order are the femur, tibia, fibula, and small bones of the feet. Multifocality is such an important feature of this tumor that, sometimes, it can be the only cue to diagnosis; however, such generalization limits the diagnostic possibilities.
Typical imaging features in EHE reveal a lytic lesion without matrix mineralization, and osseous expansile remodeling involving cortical or medullary bone on radiographs and CT. Calcification and periosteal reactions are generally not seen. Cortical disruption with resultant soft tissue involved may be present. On MRI, hypointense signal is seen on T1-weighted images and iso to hyperintense signal on T2-weighted images with variable enhancement on post-contrast images.[2] Again, multicentricity is observed in majority cases. However, wherein the features for the benign entity like hemangioma are quite diagnostic and preclude biopsy, as the grade of tumor increases, the imaging becomes more and more non- specific.[3] Certain radiological features such as extensive osseous destruction, joint involvement, and presence of extensive soft-tissue components along with clinical features can expand the limits of histopathological diagnosis.
The radiographic differential diagnosis for hemangioendotheliomas varies according to the age of the patient and number of lesions. In young patients with multiple lytic lesions, the differential includes diagnoses such as Langerhans’ cell histiocytosis, fibrous dysplasia, Brown tumors, and less likely metastases. In older patients with multifocal disease, metastases, myeloma, and lymphoma are the most likely diagnostic considerations. The differential diagnosis for solitary hemangioendothelioma varies according to the pattern of destruction, ranging from benign lesions such as fibrous dysplasia, fibrous cortical defect, or simple cyst to primary bone sarcomas such as osteosarcoma, fibrosarcoma, primary osseous lymphoma, or Ewing’s sarcoma for solitary lesions with malignant imaging features.[2] Moth eaten pattern of destruction with typical periosteal reaction such as “sunray” or “onion peeling” can narrow down the differential diagnosis.
While radiographs and CT scan help to differentiate these entities to certain extent, MRI features are often non-specific and used mainly for disease extent and pre-operative staging. Functional MRI techniques such as diffusion-weighted imaging and dynamic contrast enhancement studies help in prognosticating as well as response assessment of the disease. Baseline values can be used for the evaluation of residual or recurrent disease. MR spectroscopy is a method of molecular characterization of tumors, elucidating the metabolic footprint of the region of interest. The role of choline content has been studied by most authors since choline-containing compounds are constituents of the phospholipid metabolism of cell membranes that reflect cell membrane turnover, a feature of malignancy.
A bone scan or positron emission tomography scan is indicated for staging of disease. Staging studies serve a valuable role in the evaluation of patients with a diagnosis of hemangioendothelioma since the optimal treatment plan is determined by the presence or absence of multicentric disease.
Ultrasonography aids in visualization of tumors that are not confined to intraosseous compartment and assist in determination of consistency of the tumor or the soft-tissue component, hence assist in guided biopsy procedures. Color Doppler flow imaging allows visualization of blood flow within solid soft-tissue masses as well as has proved to be a useful tool to monitor regression of tumor neovascularity induced by therapy.
Microscopically, the lesions show vasoformative elements and involve the surrounding soft tissue. The most characteristic feature is the presence of intracytoplasmic vacuoles reminiscent of primitive lumen formation that may contain erythrocytes. Reactive bone formation may be visible in vicinity. Some EHE may less vasoformative. Immunohistochemistry is the key to diagnosis with C34, CD31, and FLI-1 in case of EHE. Appearance of atypical mitotic activity or spindle cell morphology can complicate the diagnosis. Histological features like spindling along with IHC markers of a spindle cell tumor are atypical. It may represent a transformation, a spectral jump to a higher grade of malignancy, such as epithelioid angiosarcoma. Etiopathogenesis of such transformation, as in our case, could be an incomplete or inadequate radiotherapy.
Metastasis has been shown to occur in up to 31% of cases and is more common in those with marked cellular atypia, increased mitotic activity, spindling, and necrosis.[10]
Complete resection is treatment of choice followed by radiation, chemotherapy, or combination therapy for unicentric disease. Multifocal diseases pose challenges to treatment and limited resection with chemo/ radiotherapy is generally resorted. Since angiogenesis is a hallmark of tumor growth, hence there is evidence that antiangiogenic drugs can lead to tumor regression. A variety of combinations of chemotherapeutic agents such as sorafenib, axitinib, doxorubicin, vincristine, and 5-FU has claimed to be effective; however, no consensus has been yet established.
As suggested by Wenger and Wold,[1,2] progression of EHE to sarcoma may reflect that these entities are part of a spectrum. This concept of spectral nature of vascular bone tumors has been less explored given the rarity of these tumors. Metastatic workup is recommended if imaging and history are suggestive of such changes, which can significantly alter patient management.
CONCLUSION
With clinical background of multiple recurrences post-radiotherapy, differential diagnosis of malignant (sarcomatous) transformation in cases of epithelial tumors of bone should be considered along with recurrent or residual disease.
This process could be either idiopathic or radiation induced. Incomplete radiation therapy, genetic factors along with inadequate tumor resection can be possible factors contributing.
Acknowledgment
We sincerely thank the department of pathology for the photomicrographs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Benign vascular lesions of bone: Radiologic and pathologic features. Skeletal Radiol. 2000;29:63-74.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant vascular lesions of bone: Radiologic and pathologic features. Skeletal Radiol. 2000;29:619-31.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular bone tumors: A proposal of a classification based on clinicopathological, radiographic and genetic features. Skeletal Radiol. 2012;41:1495-507.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelioid hemangioendothelioma: A vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970-81.
- [CrossRef] [Google Scholar]
- Multicentric epithelioid hemangioendothelioma involving the same lower extremity: A case report and review of literature. Int J Med Sci. 2011;8:558-63.
- [CrossRef] [PubMed] [Google Scholar]
- Multifocal epithelioid hemangioendothelioma of the foot and ankle: A case report. J Orthop Surg (Hong Kong). 2014;22:122-5.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant hemangioendothelioma of the left calcaneum associated with fever and hematological abnormalities. Skeletal Radiol. 1997;26:64-6.
- [CrossRef] [PubMed] [Google Scholar]
- Unicentric epithelioid hemangioendothelioma of the calcaneus: A case report and review of literature. Clin Sarcoma Res. 2018;8:5.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelioid hemangioendothelioma of the bone: A review and update. Adv Anat Pathol. 2014;21:254-9.
- [CrossRef] [PubMed] [Google Scholar]






