Translate this page into:
Traumatic prepatellar quadriceps continuation injury in an elite cyclist

*Corresponding author: Patrick Baker, Department of Radiology, Queen Elizabeth University Hospital, Glasgow, Scotland, United Kingdom. patrick.baker@nhs.scot
-
Received: ,
Accepted: ,
How to cite this article: Baker P, Lam L, Jacob J, McKenzie G. Traumatic prepatellar quadriceps continuation injury in an elite cyclist. Indian J Musculoskelet Radiol. 2024;6:145-8. doi: 10.25259/IJMSR_29_2024
Abstract
Injury to the prepatellar quadriceps continuation is a lesser recognized extensor mechanism injury when compared to the more commonly encountered quadriceps and patellar tendon injuries. We present a case of a traumatic injury to the prepatellar quadriceps continuation in an elite cyclist without injury to the adjacent patellar or quadriceps tendons. The magnetic resonance imaging findings depict the anatomy of the prepatellar structures in detail, as well as the sequelae of trauma. These include, but are not limited to partial or complete tearing, stripping and elevation of the anterior surface of the patella, and traumatic reactive prepatellar bursitis. Cyclists may be predisposed to injury to the prepatellar quadriceps continuation due to background overuse prepatellar friction syndrome, but as in our case, injury can also be the result of an acute traumatic insult. These injuries can be managed conservatively with physiotherapy and result in a good outcome.
Keywords
Prepatellar quadriceps continuation
Extensor mechanism
Knee injury
INTRODUCTION
We report a case of a traumatic injury to the prepatellar quadriceps continuation in an elite cyclist. While injury to the quadriceps and patellar tendons are well-documented common extensor mechanism injuries,[1,2] injury to the prepatellar quadriceps continuation has much less recognition in the literature and indeed clinically. The prepatellar quadriceps continuation can be injured concurrently with quadriceps tendon tears, but an isolated injury to the prepatellar quadriceps continuation is rare.[3] To date, there is only a single case report outlining an injury to the prepatellar quadriceps continuation.[4]
The prepatellar soft-tissue structures have been described in several cadaveric studies and generally conform to a trilaminar configuration with a degree of anatomical variation in the number and arrangement of the layers.[5-9] In theory, any one of these layers can be involved in a traumatic injury.
This anatomical distinction regarding an injury to the prepatellar quadriceps continuation could have management implications, particularly if surgical management is undertaken, although the clinical presentation and mechanism of injury may be similar. A suggestive examination finding with a complete rupture of the patellar or quadriceps tendon can be a palpable gap at its expected location and either superior or inferior migration of the patella, respectively.[1,2] This may not be readily apparent with a prepatellar quadriceps continuation injury, given the anatomy, despite the presence of a potentially significant extensor mechanism injury. The case we describe will elucidate further some other important features regarding prepatellar quadriceps continuation injury, particularly salient imaging findings and potential management implications.
CASE REPORT
A 22-year-old elite cyclist sustained a fall at high speed while competing. Due to the high speed at which the injury was sustained, it was difficult to discern the exact mechanism, but a significant traumatic injury was suspected. The patient was transferred to the local trauma center and initially underwent computed tomography imaging according to the local trauma protocol. This did not include imaging of the left knee but revealed no other significant injury. This was followed by a left knee radiograph and magnetic resonance imaging (MRI) of the left knee the following day.
On clinical examination, there was restricted motion due to pain, but the ability to raise a straight leg was preserved, and full active extension was possible. The pain was exacerbated during knee flexion, and it was not possible to elucidate the full range of motion due to the degree of discomfort.
A radiograph of the left knee showed prepatellar soft-tissue swelling but no bony injury [Figure 1].
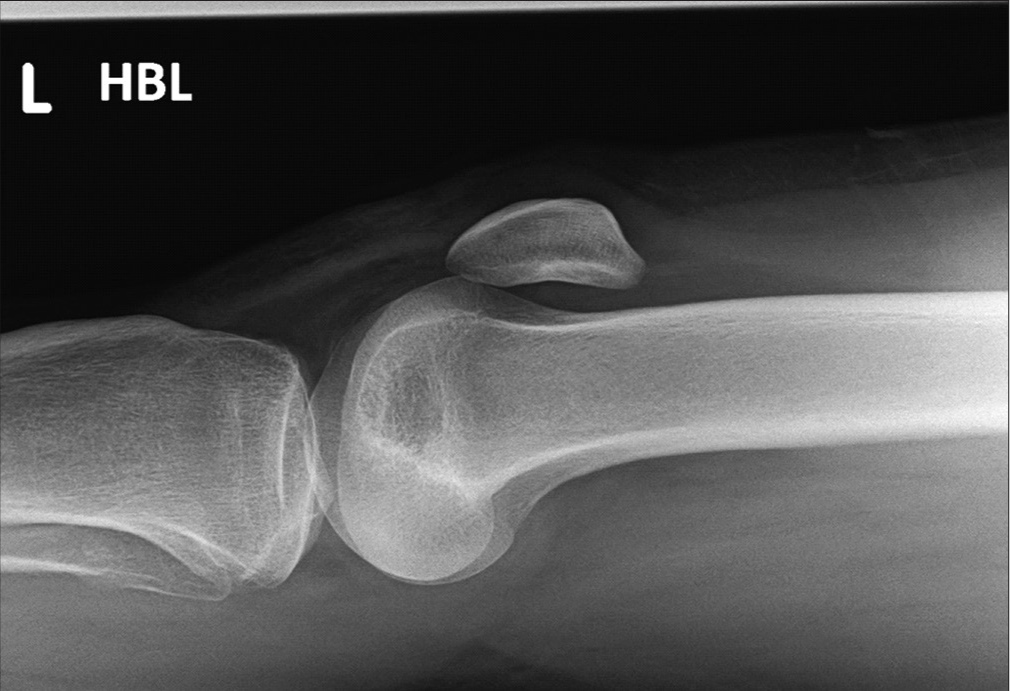
- Lateral radiograph of the left knee demonstrating prepatellar soft-tissue swelling but no bony injury, effusion, or lipohaemarthrosis. HBL: Horizontal beam lateral.
MRI revealed an injury to the prepatellar quadriceps continuation, causing the structure to elevate off the anterior patellar cortex, with stripping and partial tearing of the superior fibers [Figures 2 and 3]. Fluid was present in the prepatellar subcutaneous fat as well as between the prepatellar fascial layers, signifying traumatic bursitis [Figures 2 and 3]. Of note, there was no bone marrow edema or discrete fracture of the patella. There was no retraction of either the quadriceps or patellar tendon fibers. There was also no other bony or soft tissue injury identified elsewhere. Following orthopedic review, the patient was managed with an adjustable range of motion knee brace, initially allowing 30° of flexion. The patient was discharged the same day and returned to the elite training base for further rehabilitation. After 1 week, it was possible to begin progressive mobilization and start light pedaling. Over the subsequent 4 weeks, cycling volume and gym-based rehabilitation were progressively increased. By 2 months, full training, gym, road, and velodrome riding were possible, and a complete recovery was achieved.

- (a) Sagittal T1-weighted and (b and c) sagittal and (d) axial proton-density fat-saturated sequences of the left knee demonstrating prepatellar soft-tissue swelling of T1-weighted intermediate-tohypointense signal (a – solid arrow). Disruption of the superior prepatellar quadriceps continuation fibers (b – solid arrow) and overlying fascial layers (b – open arrow) with associated surrounding high signal on proton-density fat-saturated sequences consistent with partial tearing and edema. There is stripping of the superior prepatellar quadriceps continuation from the anterior patellar surface (c and d – solid arrow) with associated tear (c – open arrow).
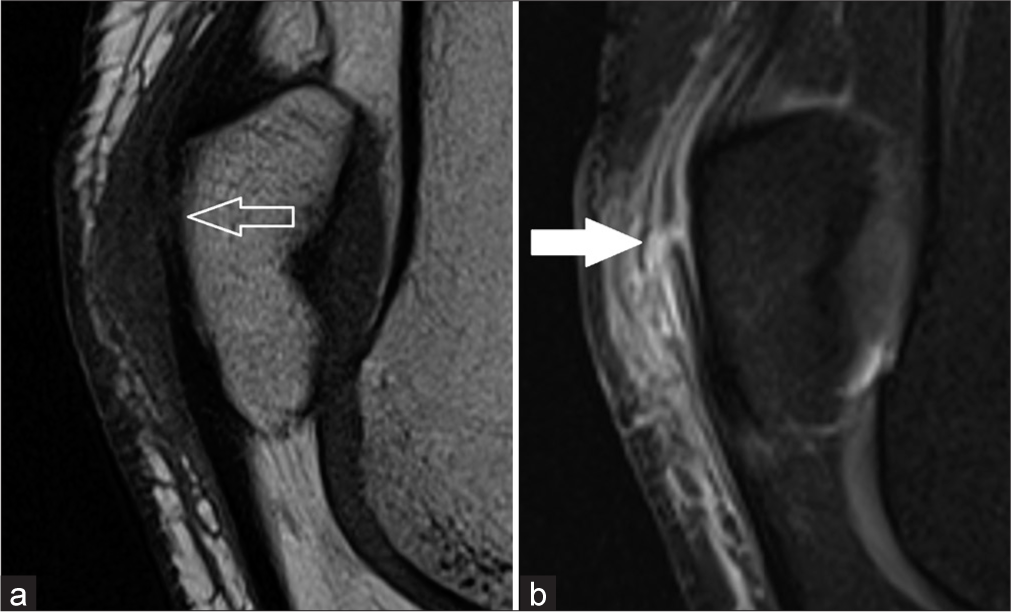
- (a) Zoomed sagittal T1-weighted and (b) proton-density fat-saturated sequences further demonstrating the disrupted prepatellar quadriceps continuation fibers (b - solid arrow) but an intact anterior patellar cortex with no fracture (a - open arrow).
DISCUSSION
Previous cadaveric studies have investigated the anatomy of the prepatellar structures in detail.[5-7] These have elucidated a trilaminar arrangement to the prepatellar structures for most individuals, with a minority of subjects having a bilaminar arrangement. For those with the more commonly encountered trilaminar arrangement, this includes a superficial transversely orientated fascial layer, intermediate obliquely-orientated aponeurotic layer comprising the distal vastus lateralis, vastus medialis and superficial rectus femoris tendons, and a deep longitudinal orientated layer comprising the distal deep rectus femoris tendon fibers.[5] The deepest of these layers was found to be intimately associated with the anterior patella through a chondroapophyseal type of attachment to a layer of fibrocartilage lining the anterior patella with no space or bursa present between the continuation and patella. The remainder of these layers have potential spaces between them, which can fill with fluid in the context of insult, in this case, trauma. These have been described as separate bursal layers as the subcutaneous, subfascial, and subaponeurotic bursae going from superficial to deep.[6,7] A schematic representation of the normal configuration and appearance of the prepatellar soft-tissue layers is depicted in Figure 4. This case delineates fluid accumulating in the subfascial and sub aponeurotic bursae well, with partial tearing of all the prepatellar fascial layers, and illustrates the presence of these additional prepatellar potential spaces.
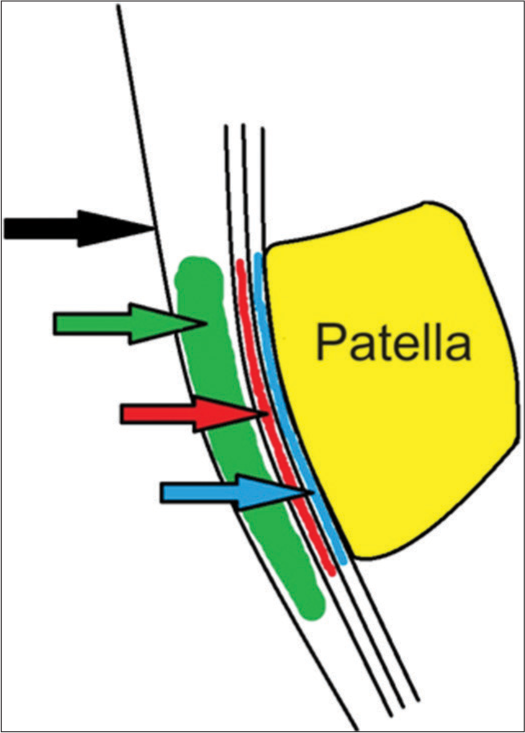
- Schematic illustration depicting the prepatellar structures and the intervening potential spaces in the sagittal plane. Black arrow – skin. Green arrow – subcutaneous prepatellar bursa. Red arrow – potential space between most superficial and intermediate layers of the prepatellar quadriceps continuation, i.e., subfascial component of prepatellar bursa. Blue arrow – potential space between the intermediate and deep layers of the prepatellar quadriceps continuation, i.e., subaponeurotic component of prepatellar bursa.
In the only other case report in the literature detailing injury to the prepatellar quadriceps continuation, the imaging was performed 4 weeks following the initial injury in an older patient with a less significant mechanism of injury.[4] The absence of the edema in the subacute setting can make identification of the injury difficult and preclude differentiation of the different layers of the prepatellar soft tissues, which was well demonstrated in our patient. The imaging appearances and, indeed, the management of an elite athlete are also likely to be different from that of an older patient with background degenerative changes in the knee.
Although the imaging findings were related to acute trauma in our case, the clinical entity of prepatellar friction syndrome related to overuse in elite cyclists has been described.[10] This is postulated to be secondary to the repetitive microtrauma of the prepatellar quadriceps continuation sliding over the anterior surface of the patella, as is encountered during long periods of cycling. It is difficult in the context of an acute injury to be certain of the absence of any predisposing tendinosis or “prepatellar quadriceps continuationosis” on imaging, but there was no suggestion of preceding pain or other clinical features of this to suggest the imaging findings were related to this entity as opposed to the acute event. The possibility of this specific anatomical region being prone to injury in elite cyclists should be borne in mind during clinical review.
The imaging modalities performed in this case were a plain radiograph followed by MRI with the routine MRI knee sequences performed at our institution (sagittal T1-weighted and sagittal, coronal, and axial proton density fat-saturated sequences). Ultrasound is also an option described to evaluate the prepatellar quadriceps continuation [4,10] with the advantages of lower cost, ease of access, and ability to perform dynamic assessment of the extensor mechanism reported. Ultrasound is, however, highly operator-dependent, and given the lack of recognition of prepatellar quadriceps injury both clinically and radiologically, diagnosis may be difficult. Indeed, in the only other case report in the literature, an ultrasound was performed at first, which failed to diagnose the injury and the diagnosis was made 4 weeks later on MRI.[4] The other study that describes ultrasound as a modality for evaluating the prepatellar quadriceps continuation is in the context of prepatellar friction syndrome[10] rather than an acute injury as in our case. Some imaging findings may be similar, such as defects in the fibers of the fascial layers but the ultrasound findings for an acute injury to the prepatellar quadriceps continuation have yet to be described. Given the rarity of this injury and interobserver variability encountered with ultrasound, MRI may be a more comprehensive imaging modality in the assessment of a possible prepatellar quadriceps continuation injury. In our case, the clinical findings were not suggestive solely of extensor mechanism injury, and there was significant clinical suspicion of derangement to other internal structures within the knee. Thus, MRI was performed to enable more global assessment, further demonstrating an additional advantage of MRI over ultrasound.
There is a paucity of literature regarding the management of these injuries, as expected, given the relatively recently described imaging findings. Both in our case and the previous case reported,[4] a satisfactory recovery was achieved with conservative management and physiotherapy. In the series detailing prepatellar friction syndrome,[10] following a trial of failed conservative therapy for the elite cyclists involved, a prepatellar fasciectomy was performed with good post-operative results reported. It may be the case; however, that traumatic prepatellar quadriceps continuation injuries can heal without the need for operative intervention, unlike complete patellar or quadriceps tendon ruptures, which generally require surgical intervention to necessitate a reasonable functional recovery.[1-3] This may be due to the deep fibers of the prepatellar quadriceps continuation being densely adherent to the anterior patella and thus making a complete functional deficit less likely. At present, until further research has been undertaken, the management of these injuries may be best decided on a case-by-case basis.
CONCLUSION
In conclusion, injury to the prepatellar quadriceps continuation is a rare injury to the extensor mechanism, especially compared to the more common injuries affecting the quadriceps and patellar tendons. Our case highlights the anatomy of the prepatellar structures on MRI and the sequelae of acute traumatic injury to these. It may be difficult to clinically ascertain the extent of internal derangement to the soft-tissue structures of the knee following injury and MRI can give a comprehensive overview, including assessment of the prepatellar quadriceps continuation. The imaging features of injury to this structure are well demonstrated on MRI, and conservative management can be successful.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Quadriceps tendon rupture. J Family Med Prim Care. 2018;7:257-60.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and risk factors of acute patellar tendon rupture, repair failure, and return to activity in the active-duty military population. Am J Sports Med. 2021;49:2916-23.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of the quadriceps femoris tendon: Distal tear characterization and clinical significance of rupture types. Eur Radiol. 2021;31:7674-83.
- [CrossRef] [PubMed] [Google Scholar]
- Prepatellar continuation rupture: Report of an unusual case. Knee. 2014;21:979-81.
- [CrossRef] [PubMed] [Google Scholar]
- Prepatellar quadriceps continuation: MRI of cadavers with gross anatomic and histologic correlation. AJR Am J Roentgenol. 2009;192:W111-6.
- [CrossRef] [PubMed] [Google Scholar]
- Soft-tissue anatomy anterior to the human patella. J Bone Joint Surg Am. 2003;85:1012-7.
- [CrossRef] [PubMed] [Google Scholar]
- The prepatellar bursa: Cadaveric investigation of regional anatomy with MRI after sonographically guided bursography. AJR Am J Roentgenol. 2007;188:W355-8.
- [CrossRef] [PubMed] [Google Scholar]
- Layered approach to the anterior knee: Normal anatomy and disorders associated with anterior knee pain. Radiographics. 2018;38:2069-101.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467:3297-306.
- [CrossRef] [PubMed] [Google Scholar]
- Prepatellar friction syndrome: A common cause of knee pain in the elite cyclist. Acta Orthop Belg. 2015;81:614-9.
- [Google Scholar]






