Translate this page into:
Ultrasound-Guided Percutaneous Needle Tenotomy for Tendinosis

*Corresponding author: Dharmendra Singh, Department of Radiodiagnosis, VM Medical College and Safdarjung Hospital, New Delhi - 110 029, Delhi, India. dksinghrad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh D, Nayak B, Kumar M, Tomar S, Katyan A, Suman S, et al. Ultrasound-guided percutaneous needle tenotomy for tendinosis. Indian J Musculoskelet Radiol 2020;2(1):52-7.
Abstract
Tendinosis is an important cause of musculoskeletal pain and disability. Tendinosis is principally a degenerative process, rather than inflammatory as was traditionally believed. Consequently, traditional tendinosis treatments focused solely on decreasing inflammation, i.e. intratendinous corticosteroid injection has often been ineffective. The advancement of ultrasonography as for the guidance of musculoskeletal intervention has facilitated the development of percutaneous procedures focused on the regenerative healing process for the treatment of tendinosis. In this article, our aim is to illustrate the technical aspects of ultrasound-guided percutaneous needle tenotomy for the treatment of tendinosis.
Keywords
Ultrasound-guided intervention
Musculoskeletal intervention
Tendinosis
Percutaneous needle tenotomy
INTRODUCTION
Tendinosis constitutes one of the most common etiologies of musculoskeletal pain and disability. In contradiction to the prior considerations, tendinosis is not an inflammatory process, rather a degenerative one. Tendinosis represents a failed healing response leading to the decreased mechanical integrity of the affected tendon. Histopathologic examination characteristically reveals disorganized proliferation of tenocytes, disrupted organization of collagen fibers, an increase in the noncollagenous matrix, and neovascularization; described as angiofibroblastic hyperplasia. The nerve fibers that develop in the area of tendinosis along the neovascularization are responsible for the pain associated with tendinosis.[1-3] Various conservative treatment options for tendinosis such as rest, analgesics, topical vasodilators, and extracorporeal shock wave therapy have shown variable success rates.[4,5] Corticosteroid injection, once a mainstay of treatment for tendinosis, is rather contraindicated inside the tendon.[6] With the emergence of high-resolution diagnostic musculoskeletal ultrasound (US), tendinosis is better evaluated at point of care. US features of tendinosis include tendon thickening with regions of fibrillary disorganization, ill- defined hypoechogenicity, and possible neovascularization represented by intratendinous and peritendinous blood flow observed by color or power Doppler US [Figure 1a and b]. The adjacent cortical bone at the tendon attachment or footprint frequently exhibits irregularity, pitting, and enthesophyte formation. Tendon tears are often associated with tendinosis, which structurally weakens the tendon.[7] Increased understandings of imaging and histological features of tendinosis have also led to the development of US-guided percutaneous procedures focused on the regenerative healing process for the treatment of tendinosis. These procedures include US-guided percutaneous orthobiologic interventions such as percutaneous needle tenotomy (PNT).[8] The article aims to illustrate the technical aspects of US-guided PNT for the treatment of tendinosis.

- Longitudinal grey scale ultrasound (US) (a) and Doppler US (b) of the lateral elbow demonstrate hypoechoic area in common extensor tendon near attachment (Yellow arrow) and increased color flow/neovascularization (Red arrow) consistent with tendinosis. Red asterisk: Common extensor tendon.
US-GUIDED PNT
US-guided PNT involves repeatedly passing a needle under US guidance through the targeted area of tendinosis to disrupt the degenerative process, including scar tissue, and encouraging localized bleeding, and fibroblast proliferation, which can lead to growth factor release, collagen formation, and ultimately healing. The brief mechanism of action is illustrated in “[Figure 2].”

- Illustration demonstrating mechanism of action of tenotomy.
The US-guided PNT is an accepted technique for the treatment of tendinosis within the limitations of current literature. Several other percutaneous treatments for tendinosis that includes prolotherapy, autologous whole- blood injection, and autologous platelet-rich plasma injection are often performed in conjunction with PNT.[9-13]
Our experience of US-guided PNT followed by rehabilitation, over the period of 1 year from October 2018 to October 2019, in 74 patients having variable degrees of tendinosis in different tendon groups without a coexistent tear (common extensor tendon n = 33; Achilles tendon n = 13, patellar tendon n = 11, adductor tendon n = 9, and gluteus medius tendon n = 8) had shown statistically significant results. The mean value of visual analog score (VAS) at presentation was 8.02 ± 0.72 with median (interquartile range) of 8 (7.75–9) which was significantly decreased to 3.16 ± 1.63 with median (interquartile range) of 3 (2–3) after 6 weeks of PNT and rehabilitation.
The patient selection for US-guided PNT depends on the clinico-radiological qualitative and quantitative assessments. The qualitative clinical assessment is the presence of pain and disability attributable to the affected tendon. The quantitative clinical assessments are done by VAS and various disability scores for each region such as disabilities of the arm, shoulder, and hand score.[14] The radiological assessment is done by the US which includes the presence of intratendinous hypoechogenecity with or without a discrete tear, intratendinous and/peritendinous color flow on Doppler, and the presence or absence of underlying bony changes. The quantitative radiological assessments are the dimension of the hypoechoic area of tendinosis and measurement of tear, if present. The quantitative clinico-radiological assessments serve as baseline values for comparative analysis on follow- up. The criteria of patient selection for US-guided PNT are summarized in “Table 1.”
| Clinical score (VAS) | More than 5 |
|---|---|
| US imaging appearance of tendon | The hypoechoic area on the US with intratendinous and/peritendinous color flow on Doppler. Absence of tendon tear. |
VAS: Visual analog score, US: Ultrasound, PNT: Percutaneous needle tenotomy
The pre-requisite biochemical reports before the intervention are prothrombin time, INR, total and differential leucocyte count, ans viral markers (HBsAg, HCVAg, and human immunodeficiency viruses-1 and II). Clinical signs of infection such as cellulitis/abscess on the overlying skin and partial thickness/full thickness tendon tear are the contraindications for US-guided PNT. Patient is instructed to stop any anti-inflammatory medication at least 3 weeks before the procedure.
An informed written consent is obtained and the possibility of complications such as post-procedural pain, vasovagal syncope, burning sensation, swelling, and infection is explained to the patient. The patient is counseled about the variable outcome of the procedure, which may be adversely affected due to chronicity of tendinosis, associated calcification, disuse of muscle due to chronic tendinosis, overuse of antagonist’s muscle, and strenuous exercise during 1st week after PNT and poor compliance of post-procedural rehabilitation. The patient is also instructed that he/she might need reintervention after 6 weeks if the results are not significant in terms of clinical outcome.
The intervention is preferably performed in the patient in a lying down position to minimize the chances of vasovagal syncope. The position of the patient should be in such a manner that the US monitor is always in front of the radiologist. The positioning of patient for US-guided PNT is summarized in “Table 2.”
| Anatomical location | Position |
|---|---|
| Supraspinatus tendon | Lateral decubitus position with the affected shoulder up and hand in Jeffrey crass position. |
| Subscapularis tendon | Supine position with the arm adducted and externally rotated. |
| Infraspinatus tendon | Lateral decubitus position with the affected shoulder up and arm adducted, internally rotated (hand holding contralateral shoulder). |
| Common extensor tendon | Supine position with the arm adducted and internally rotated; elbow flexed to 90 degrees and hand pronated resting on the abdomen. |
| Common flexor tendon | Supine position with arm abducted and externally rotated. |
| Distal biceps tendon | Supine position; elbow hyperextended, and hand supinated. |
| Adductor tendon | Hip abducted and externally rotated, knee flexed to 90 degree. |
| Gluteus medius and minimus | Lateral decubitus position with affected greater trochanter up and knee semiflexed. |
| Quadriceps tendon | Supine position with knee semiflexed (Pillow below the knee) |
| Patellar tendon | Supine position with knee semiflexed (Pillow below the knee) |
| Tibialis posterior | Supine position, knee semiflexed, ankle everted (lateral border of foot touching couch). |
| Tibialis anterior | Supine position, knee semiflexed, ankle plantar flexed (foot resting on the couch) |
| Peroneus tendon | Lateral decubitus position with affected foot up, hindfoot inverted. |
| Proximal and distal hamstring tendon | Prone position, hip and knee extended. |
| Achilles tendon | Prone position, foot dorsiflexed, and at the side of couch. |
US: Ultrasound, PNT: Percutaneous needle tenotomy
The patient’s body part for intervention is thoroughly cleaned with an alcohol-based disinfectant and chlorhexidine; subsequently, it is air-dried and covered with sterile drapes. The musculoskeletal radiologist performing the intervention should put on a sterile gown as well as sterile gloves.
A linear transducer of 9–12 MHz or 12–18 MHz is used to localize the lesion depending on the depth of the lesion. The transducer must be covered with a sterile probe cover before the intervention. Care should be taken to use sterile US jelly on the aseptic intervention area. The probe should be kept stable on the area of interest using the ring and little finger resting on the area of interest; while rest of three fingers are holding the probe [Figure 3].
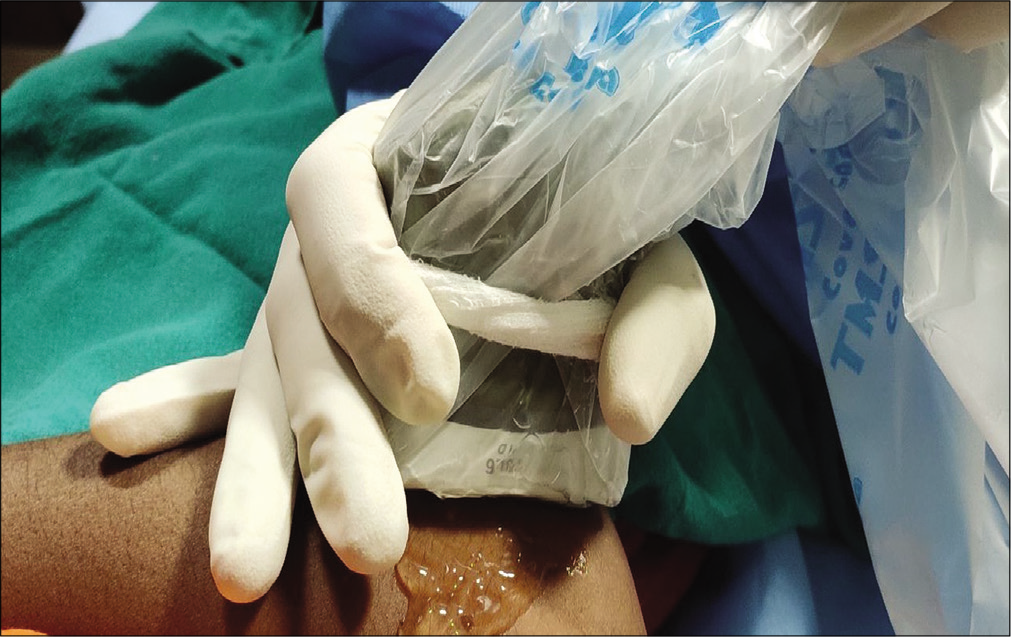
- Image demonstrating probe holding position during ultrasound-guided percutaneous needle tenotomy.
The preferred approach used for the intervention is the in- plane approach [Figure 4a and b]. Under US-guidance 1% lidocaine is infiltrated into the skin, subcutaneous plane and up to the surface of tendon concerned. The needle (usually 21–23 G) is then advanced into the area of tendinosis. Lidocaine is usually not injected into the area of tendinosis while doing PNT. The beveled edge of the needle should preferably be kept up to reach the relatively deep fibers; whereas the beveled edge of the needle should be kept down to reach the superficial fibers [Figure 5a and b]. Once within the target, the needle is repeatedly moved-in and -out in a conical manner to cover all segments of the tendinosis, but care should be taken not to go outside the tendon boundary. It is preferred to abrade the bony margin with needle tip while doing PNT, if tendinosis is near the bony attachment. The PNT is done until there is a lack of resistance; or when the hypoechoic area of tendinosis becomes isoechoic to the normal-appearing tendon [Figure 6a and b]. Usually, 15–20 strokes of tenotomy in one sitting are sufficient to achieve the desired result. One of the major advantages of doing PNT under US-guidance is this precise endpoint; whereas when performing blind PNT, we do not confidently know when to end the procedure. Slender tendons such as distal biceps brachii and semitendinosus require only 5–10 strokes of PNT. However, there is a paucity of studies on the outcome analysis of US-guided PNT for tendinosis of slender tendons.

- Image (a) and corresponding longitudinal ultrasound (US) of the lateral elbow (b) demonstrating relative position of needle and US probe during in plane technique of intervention in (a). The corresponding US image in (b) demonstrates whole length of needle trajectory and needle tip (small yellow arrows) in one plane.

- Longitudinal ultrasound demonstrate needle in the area of tendinosis with needle in hub up position (yellow arrow) for tenotomy of deep fibers in (a) and needle in hub down position (Red arrow) for tenotomy of superficial fibers in (b).

- Longitudinal ultrasound of the lateral elbow demonstrates area of tendinosis as hypoechoic area before percutaneous needle tenotomy (PNT) (area inside yellow circle) in (a) and after PNT (area inside yellow circle) in (b).
Once PNT is done, the needle is withdrawn; the puncture site is secured with sterile gauze and sterile adhesive bandage.
Some prefer to inject steroid superficial to the tendon after PNT, in the same sitting, particularly in the tendinosis of common extensor tendon. However, this is counterproductive and against the concept of creating an inflammatory response. The steroids hinder neovascularity in the area of tenotomy and should, therefore, be avoided.[6,10]
The patient is instructed to avoid strenuous exercise for 1 week post-procedure. The anti-inflammatory medicines are contraindicated for 4 weeks; however, limited use of opioid- based analgesics is encouraged to limit post-procedure pain. After 1 week, the patient is instructed to commence rehabilitation of the tendon under the supervision of a sports clinician. The specific rehabilitation program is for 5 weeks; which includes 2 weeks of isometric strengthening, 2 weeks of concentric strengthening, and 1 week of eccentric strengthening of the tendon. The patient is instructed to come for follow-up imaging after 6 weeks.
On follow-up, the clinical parameter of favorable response is the reduction of VAS score with an increased range of movement; while a reduction in the size of hypoechogenecity of tendinosis with the presence of Doppler flow in the area of tenotomy is the sonographic parameter for a favorable outcome of PNT. If clinico-radiological parameters are not favorable after 6 weeks follow-up, then the PNT followed by rehabilitation may be repeated, or the PNT may be combined with platelet-rich plasma injection. The proposed working template for US guided PNT is summarized in “Table 3.”
| S. No. | Check list | Remarks | |
|---|---|---|---|
| 1. | Pre-intervention Clinical assessment | Baseline VAS Baseline disability score |
|
| 2. | Pre-intervention Imaging assessment | US - Tendinosis present/absent If present dimension - With/without tear (If tear present, dimension-) - Bony changes – Present/absent (If present – specify) |
|
| 3. | Lab reports | PT/INR……………………………. TLC………………………………………………. DLC……………………………………………… Platelets……………………………………. Viral markers: HBsAg…... HCVAg………..HIV I and II……… |
|
| 4. | Any sign of infection in overlying skin such as cellulitis and abscess. | Yes/No | |
| 5. | The patient stopped taking an anti-inflammatory drug | Yes/No (If yes, date when stopped) |
|
| 6. | Date of procedure | ||
| 7. | Post-procedure instructions 1. To take opioid based analgesic if severe pain, 2. Anti-inflammatory medicines contraindicated for 4 weeks. 3. Rest for 1 week 4. Rehabilitation after 1 week for 5 weeks |
||
| 8. | Date of follow-up | ||
| 9. | Follow-up Clinical assessment | VAS- Disability score- |
|
| 10. | Follow-up imaging assessment | Tendinosis- Present/Absent (If present – dimension of tendinosis) (Reduced/No change/Increased) Color flow on Doppler – Present/Absent. |
|
| 11. | If need for re-intervention | ||
US: Ultrasound, PNT: Percutaneous needle tenotomy
CONCLUSION
Appropriate patient selection, thorough pre-intervention work up, strict aseptic precaution, meticulous intervention technique using the standard protocol, post-intervention rehabilitation and follow-up are the cornerstones for favorable clinical outcome of US-guided PNT. Based on the regenerative physiology, the US-guided PNT followed by rehabilitation has the potential to become the treatment of choice for tendinosis without a coexistent tear. However, studies with larger sample sizes are required to validate the outcome of US-guided PNT for tendinosis.
Key points
-
Tendinosis is a degenerative condition rather than an inflammatory one. Therefore, regenerative healing treatments such as US-guided percutaneous orthobiologic treatments are showing promising results as compared to anti-inflammatory treatments.
The US-guided PNT is done till the hypoechoic area of tendinosis becomes isoechoic to the normal-appearing tendon or a lack of resistance. This precise endpoint is one of the major advantages of doing US-guided PNT as compared to the blind PNT.
The outcome of US-guided PNT may be adversely affected due to the chronicity of tendinosis, associated calcification, disuse of muscle due to chronic tendinosis, and overuse of antagonist’s muscle and poor compliance with rehabilitation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Tendinopathy and inflammation: Some truths. Int J Immunopathol Pharmacol. 2011;24(Suppl 2):45-50.
- [CrossRef] [PubMed] [Google Scholar]
- Conservative management of tendinopathy: An evidence-based approach. Muscles Ligaments Tendons J. 2012;1:134-7.
- [Google Scholar]
- Tendinosis: Pathophysiology and nonoperative treatment. Sports Health. 2009;1:284-92.
- [CrossRef] [PubMed] [Google Scholar]
- Eccentric loading versus eccentric loading plus shock-wave treatment for midportion achilles tendinopathy: A randomized controlled trial. Am J Sports Med. 2009;37:463-70.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of tendinopathy what works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008;466:1539-54.
- [CrossRef] [PubMed] [Google Scholar]
- Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: A randomised controlled trial. Lancet. 2002;359:657-62.
- [CrossRef] [Google Scholar]
- Guided interventions in musculoskeletal ultrasound: What's the evidence? Clin Radiol. 2011;66:140-52.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound guided dry needling and autologous blood injection for patellar tendinosis. Br J Sports Med. 2007;41:518-21.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: Is a corticosteroid necessary? J Ultrasound Med. 2008;27:1137-44.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med. 2009;28:1187-92.
- [CrossRef] [PubMed] [Google Scholar]
- Tendon needling for treatment of tendinopathy: A systematic review. Phys Sportsmed. 2015;43:80-6.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided fenestration of tendons about the hip and pelvis: Clinical outcomes. J Ultrasound Med. 2015;34:2029-35.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: A prospective study. J Shoulder Elbow Surg. 2015;24:67-73.
- [CrossRef] [PubMed] [Google Scholar]






