Translate this page into:
Vacuum Phenomenon in Parameniscal Cyst Masquerading as Infection – An Unusually Rare Presentation of a Common Entity

*Corresponding author: Alagiri Karikalan Radiology, Ganga Medical Centre and Hospital, Coimbatore - 641 4043, Tamil Nadu, India. drazhagiri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhari P, Rajkumar N, Karikalan A. Vacuum Phenomenon in Parameniscal Cyst Masquerading Infection – An Unusually Rare Presentation of a Common Entity. Indian J Musculoskelet Radiol 2020;2(1):66-8.
Abstract
Parameniscal cysts are a common entity in daily practice and are found in association with a meniscal tear. Vacuum phenomenon within joints and discs can be seen secondary to degeneration or application of traction, which is believed to be released from adjacent soft tissues. Although the vacuum phenomenon is frequently present within the joints, it is rare within a parameniscal cyst which resulted in a diagnostic dilemma. In this article, we present an unusual case with a combination of two rare entities, vacuum phenomenon within a large parameniscal cyst, which has not been reported so far along with management considerations.
Keywords
Vacuum phenomenon
Knee joint
Parameniscal cyst
INTRODUCTION
Parameniscal cysts are the most common subtype of meniscal cysts. They are a relatively common entity in daily practice and are usually found in association with a meniscal tear. However, the vacuum phenomenon within a parameniscal cyst has not been reported so far in the literature. In this article, we report a rare case of a large parameniscal cyst showing a vacuum phenomenon mimicking an infection.
CASE REPORT
A 75-year-old man presented to our outpatient clinic with complaints of bilateral knee pain more on the left side for 2 years, the pain was insidious in onset, progressive in nature, aggravated by activities, relieved by rest, and analgesics. The patient noticed a painless swelling on the medial aspect of his left knee which was gradually increasing in size followed by pain for 1 week. It was not associated with fever or loss of appetite.
On inspection, the swelling was firm, tender, and fluctuant with mild redness of the overlying skin. There was no joint instability, his stance and gait were normal.
Plain radiograph of the left knee joint [Figure 1] showed a well-defined radio-opacity along the medial border of the joint and proximal tibia with few air foci within it. In addition, there were degenerative changes in the joint. Since the lesion was of gradual onset with recent onset of pain and with radiographic features of soft-tissue lesion, magnetic resonance imaging (MRI) was performed for further evaluation.
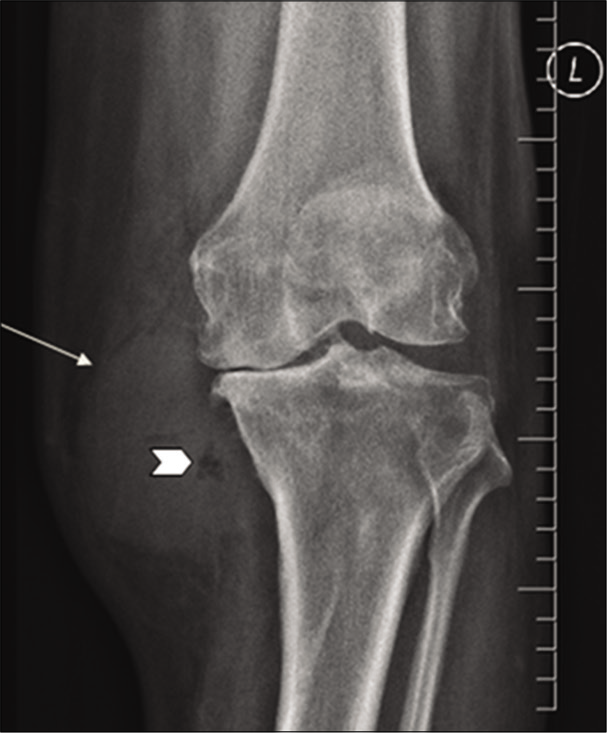
- Plain radiograph of the left knee joint showing a well- defined radio-opacity (arrow) along the medial border of the joint and proximal tibia with few air foci within it (arrowhead). Note the degenerative changes in the joint, predominantly in the medial compartment.
MRI [Figure 2a and b] showed a large well-defined fluid intensity lesion adjacent to the medial meniscus extending caudally along the medial border of the proximal tibia. The lesion was thick walled with multiple internal septa along with hypointense foci at the center which showed subtle susceptibility artifacts suggesting air pockets. Minimal perilesional soft-tissue edema was seen. The tibial attachment of medial collateral ligament was not visualized separately from the lesion. The medial border of the proximal tibia also showed areas of erosions with edema. Other findings were maceration of the posterior horn of the medial meniscus with degenerated and extruded body, significant medial patellofemoral joint space reduction with cartilage loss, and subchondral edema. Anterior cruciate ligament showed mild mucoid degeneration.
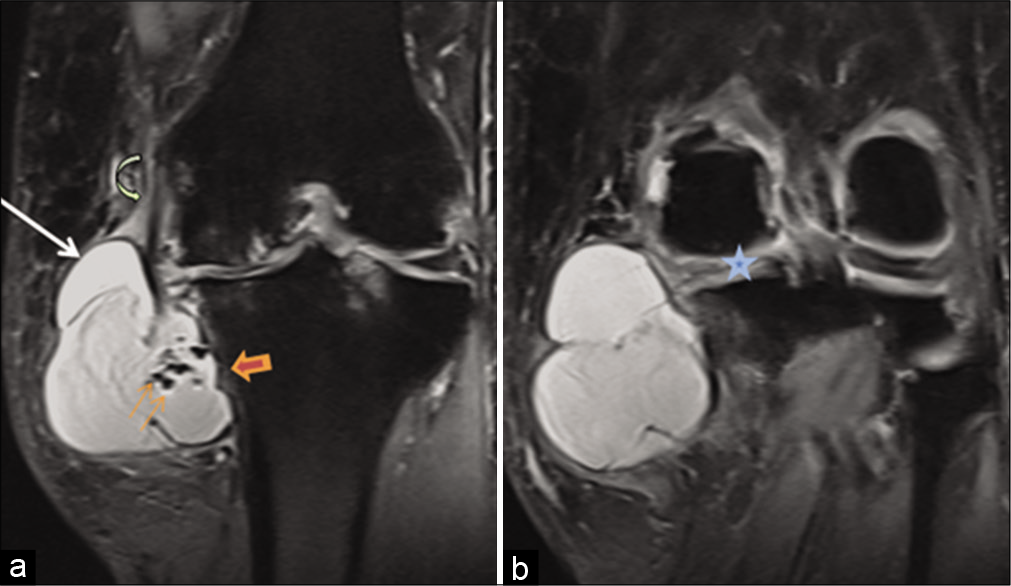
- Magnetic resonance imaging TRIM coronal images showing (a) a large complex cyst (arrow) with air pockets (thin arrows), tibial cortical erosion (arrowhead), and edema, femoral attachment of medial collateral ligament was seen (curved arrow); however, the tibial attachment was indistinct (not shown). (b) Macerated medial meniscus with articular cartilage loss and subchondral edema is also seen (star).
Computed tomography (CT) [Figure 3] was performed to look for bone involvement which revealed tiny erosions, suspicious periosteal reaction, air within the lesion and medial joint space. Air within the medial compartment of the joint could not be appreciated in MRI.
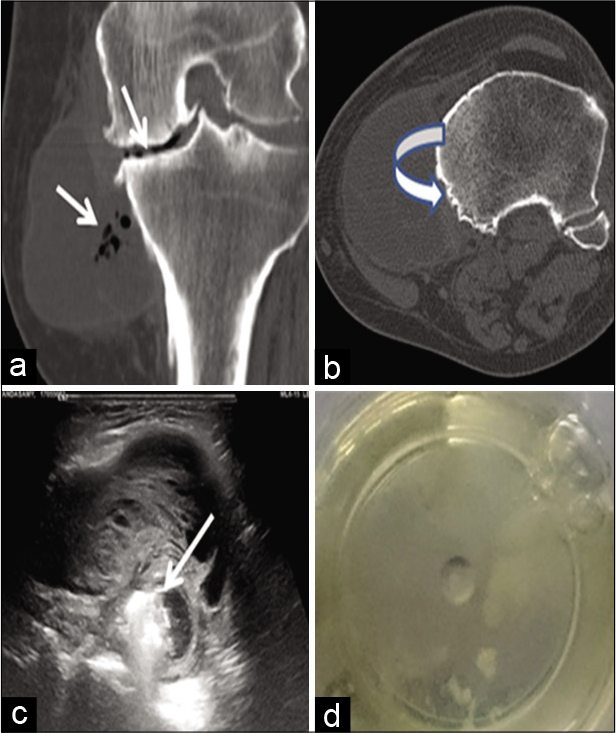
- (a,b) Coronal and axial computed tomography images showing tibial cortical erosion (curved arrow), air foci within the lesion, and medial joint space. (c) Ultrasound showing the complex nature of the cyst as thick septations and air pockets (arrow) within it. (d) Ultrasound-guided aspirate from the lesion showing clear yellowish gelatinous material.
Although the possibility of a large parameniscal cyst with vacuum phenomenon in joint and cyst was considered, superadded infection could not be ruled out; hence, USG- guided aspiration was performed. Histopathology revealed clear mucinous material [Figure 3] with no evidence to suggest infection.
The patient was then treated on a later date by cyst excision and total knee replacement.
DISCUSSION
The vacuum phenomenon is an accumulation of gas (commonly nitrogen) within a closed joint released from the surrounding tissues secondary to negative pressure. This is commonly observed in the degenerated disc or within the joints of the patients under traction, especially in children. The term “vacuum phenomenon” was first coined by Fick in 1910 who studied joints under traction and concluded that low pressure within the joint following traction leads to the release of gases from the adjacent soft tissues with variable quantities of oxygen, carbon dioxide, and nitrogen.[1]
Miller, who evaluated seven cases of spontaneous vacuum phenomenon, found that this could be a positive indicator of degenerative meniscal tear and chondrosis.[2]
Although uncommon, the vacuum can be seen on plain radiograph of knee if significant in quantity. MRI of the knee can show a minimal amount of gas in gradient recalled echo sequences which can be missed in a routine spin- echo sequence.[3] There are reports of vacuum phenomenon mimicking cartilage and meniscal pathology.[3,4]
Parameniscal cysts are a frequent finding in MRI knee having an incidence of 4–8%.[5,6] In the literature, the average size of parameniscal cyst is about 1.9 cm with only few reports of size as large as 10–11 cm.[6-8] The medial location of the parameniscal cyst is more common as compared to the lateral side with 96% of them having an underlying degenerative or traumatic meniscal tear.[6] The etiopathogenesis of meniscal cysts remains controversial. Nevertheless, the most accepted theory is that a lesion of the meniscus leads to extrusion of synovial fluid forming a collection in the adjacent parameniscal soft tissue.[9] Parameniscal cysts can mimic soft-tissue lesions, bakers cyst, and other cystic and other cystic lesions lesions, both clinically and radiologically.[10]
Our case is unique with all rare presentations of a parameniscal cyst, such as larger size, vacuum from the joint dissecting into the cyst, and pressure erosion of the adjacent tibial cortex. The most peculiar and interesting finding was vacuum phenomenon within the cyst which has never been reported so far. The air pockets within the cyst mimicked an infection, prompting us to do an usg guided aspiration. But, the aspirate turned out to be sterile synovial fluid. The patient was called back on a later date for cystectomy and total knee replacement which is a known definitive option.[8]
CONCLUSION
Large parameniscal cysts are uncommon, however when associated with rare findings such as air pockets within the cyst and erosion of adjacent bone adjacent bone, additional investigation, additional investigation, such as ultrasound- guided aspiration, is recommended to rule out infection and other aggressive mimickers. In our case, ultrasound-guided aspiration proved to be beneficial in making a confirming the diagnosis and guiding proper treatment.
Declaration of patient consent
Patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Vacuum pneumatography and the spontaneous occurrence of gas in the joint spaces. J Bone Joint Surg. 1950;32:933-8.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous vacuum pneumarthrography revisited: The significance of the vacuum phenomenon in the lateral compartment of the knee. Arthroscopy. 1998;14:576-9.
- [CrossRef] [Google Scholar]
- Minute amounts of intraarticular gas mimicking torn discoid lateral menisci. J Magn Reson Imaging. 2010;31:698-702.
- [CrossRef] [PubMed] [Google Scholar]
- Vacuum phenomenon simulating meniscal or cartilaginous injury of the knee at MR imaging. Radiology. 1991;180:513-5.
- [CrossRef] [PubMed] [Google Scholar]
- New observations on meniscal cysts. Skeletal Radiol. 2010;39:1187-91.
- [CrossRef] [PubMed] [Google Scholar]
- Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. AJR Am J Roentgenol. 2011;196:W180-6.
- [CrossRef] [PubMed] [Google Scholar]
- Giant medial parameniscal cyst in an osteoarthritic knee. Orthopedics. 2009;32:e978-84.
- [CrossRef] [PubMed] [Google Scholar]
- Knee arthroplasty in patient with a giant medial meniscal cyst: Case report. Ilizarov J Clin Exp Orthop Tom. 2017;23:359-63.
- [CrossRef] [Google Scholar]
- Relative incidence and morphology of lateral and medial meniscal cysts detected by magnetic resonance imaging. Clin Radiol. 1995;50:778-81.
- [CrossRef] [Google Scholar]
- MRI characteristics of cysts and “cyst-like” lesions in and around the knee: What the radiologist needs to know. Insights Imaging. 2013;4:257-72.
- [CrossRef] [PubMed] [Google Scholar]






