Translate this page into:
A rare case report of fibrous dysplasia with aneurysmal bone cyst-like changes of femur and innominate bone

*Corresponding author: Jyoti Gupta, Department of Radiodiagnosis and Interventional Radiology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. jyotigupta99@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta J, Jamwal R. A rare case report of fibrous dysplasia with aneurysmal bone cyst-like changes of the femur and innominate bone. Indian J Musculoskelet Radiol. 2024;6:57-60. doi: 10.25259/IJMSR_58_2023
Abstract
Fibrous dysplasia (FD) is a common disorder of the skeletal system in which normal bone deposition and remodelling are disturbed and are replaced by anomalous fibrous tissue of varying stages. The age of presentation may vary depending on the genetic penetration and severity of the disease. Aneurysmal bone cyst (ABC) is a non-aggressive neoplastic pathology wherein there is the presence of blood-filled intramedullary cystic lesions and resultant aneurysm-like dilatation of the involved bone that may be a standalone true neoplasm or ABC-like changes associated with other lesions. Concurrence of FD with ABC-like changes is an uncommon entity with most of such cases involving the craniofacial location. To the best of our knowledge, only two cases of appendicular skeleton FD with ABC could be found in the literature, and neither of them is from the Indian subcontinent. Herein, we report one such case of appendicular FD with concomitant ABC-like changes presenting in the adolescent age group. Prompt and accurate diagnosis guides further surgical management and helps in avoiding inadvertent complications.
Keywords
Fibrous dysplasia with aneurysmal bone cyst
Fibrous dysplasia of bone
Bone cysts
aneurysmal
Secondary aneurysmal bone cyst
INTRODUCTION
Fibrous dysplasia (FD) is a common sporadic musculoskeletal disorder characterized by the replacement of the osseous matrix of the bones by fibrous tissue in varying stages. It is the result of genetic mutation affecting the GNAS1 gene with resultant dysfunctional osteoblasts and accelerated bony resorption.[1]
An aneurysmal bone cyst (ABC) is a benign neoplasm occurring due to the deregulation of the USP6 gene, affecting the bone characterized by classical imaging findings and is neither an aneurysm nor a cyst. ABC-like changes, previously known as secondary ABC, are non-neoplastic changes associated with multiple benign and malignant tumors such as chondroblastoma, osteoblastoma, non-ossifying fibroma, and giant cell tumors, and do not show the deregulation of the USP6 gene.[2]
The concurrence of FD with ABC-like change is uncommon and seldom reported, with only a few published case reports in the literature primarily depicting craniofacial FD with ABC-like changes. Herein, we report one such exceptional case of FD with ABC-like changes in the lower extremity, which represents an addition to the paucity of existing literature and discuss the role of magnetic resonance imaging (MRI) in accurate diagnosis and management.
CASE REPORT
A 17-year-old male patient was referred from a primary care center to a tertiary care center with complaints of the right lower limb and hip pain with acute exacerbation for the past 1 week. The patient underwent an X-ray pelvis with both hip joints in the primary center, which was lost by the patient. On clinical examination, there was mild restriction of hip movements, for which the patient was referred for an MRI hip examination. MRI Figures 1 and 2a revealed the presence of mild expansile T2 Non FatSat (NFS) and Fat Sat (FS) hyperintense lesion in the right innominate bone with the presence of thin-walled circumscribed fluid-fluid levels within. Few thin internal septations were seen. Mild hyperintensity was seen in the surrounding muscles, along with mild periosteal location. The head of the femur and acetabulofemoral joint per se was normal except for mild reduced superior joint space. A similar signal intensity lesion was also seen involving the proximal femoral metaphysis and entire diaphysis with cortical thinning, coxa magna, and vara deformities representing classical shepherd’s crook deformity. There was a curvilinear T2 hypointense line in the neck of the femur, suspicious of fracture. The non-contrast computed tomography (CT) scan was done to confirm the same Figure 2b, which revealed a minimally displaced pathological fracture in the sub-trochanteric region of the neck of the femur. Ground glass matrix was seen in the right innominate bone and right femur, along with the presence of eccentric mildly expansile lytic lesions corresponding to the cystic spaces on MRI examination. Skeletal survey and endocrinological examination were unremarkable. The patient was referred for surgical management and underwent surgical fixation for the fracture along with bone cementing of the neck cystic lesion. A final diagnosis of polyostotic FD with ABC-like changes and a pathological sub-trochanteric fracture was made, which was confirmed in histopathology [Figure 3]. The patient was discharged without any complications.

- (a-c) Sequential axial T2-weighted (T2W) Non Fat Sat images of the pelvis and acetabulofemoral joint and (d) axial T2-weighted image (T2WI) FS at the level of the iliac blade showed mild expansion of the right iliac bone with thin-walled septated cystic lesion showing internal fluid-fluid levels with dependent T2 hypointensity (white arrows). Mild adjacent soft tissue (black arrow) and periosteal (curved white arrow) thickening were seen. Axial T2WI at the level of the acetabulofemoral joint (c) showed mild uniform marrow altered signal intensity (star) involving the neck and meta-diaphysis. The femoral epiphysis (dashed white arrow) showed normal signal intensity. (e and f) Coronal Proton Density Fat Sat (PDFS) images of both hip joint and proximal femur showed the mild expansion of the right innominate bone (solid white arrow), mild coxa vara deformity (curved white arrow) with resultant shepherd-crook deformity, and mixed marrow lesions involving the right femoral shaft (rectangular arrow). The left femur shows normal marrow signal intensity (red arrow).

- (a) Coronal PDFS magnetic resonance imaging of hip joints, femur, and proximal knee joints showed the extent of involvement of the right innominate bone and right femur. A hypointense line was seen in the neck of the femur (solid white arrow), suspicious of fracture. (b) Corresponding coronal maximum intensity projection (MIP) computed tomography scan image (b) showed the classical ground glass matrix of fibrous dysplasia (star) and interspersed lytic lesions. A hypodense minimally displaced fracture line was seen in the neck of the femur (White arrow).
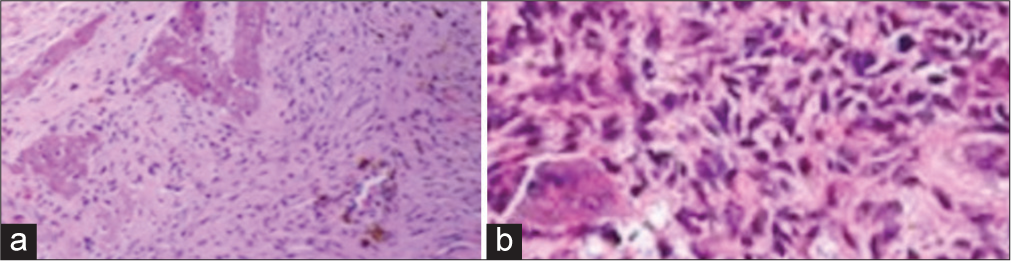
- (a and b) Histopathology images show (a) the presence of osseous trabeculae in the background of fibrous changes and (b) vascular endothelial channels.
DISCUSSION
FD is a sporadic bone proliferation disorder with two clinic- radiological subtypes. Monostotic FD is mostly an asymptomatic bone proliferation disorder and is commonly diagnosed as an incidental finding on radiographs acquired for other causes. Polyostotic FD may be symptomatic or asymptomatic depending on the presence or absence of associated endocrinal abnormalities. The classical radiographic features of FD are the ground glass appearance of the matrix associated with cortical thinning and bony expansion. ABC is commonly seen true neoplasm in children and adolescent age group, with a classical radiograph depicting the presence of an eccentric expansile lytic metaphyseal lesion with a thin sclerotic rim with a blowout appearance in cases with a large size. ABC-like changes are commonly associated with chondroblastoma, giant cell tumor, osteoblastoma, and sometimes with malignant osteosarcoma. The concurrence of ABC-like changes is very rare and is mostly seen in the craniofacial FD. Only a handful of cases reported in the concurrence of FD in the appendicular skeleton with ABC-like changes. Our case showed the presence of polyostotic FD with ABC-like changes involving the innominate bone and femur with a pathological fracture best diagnosed on combined computed tomography (CT) and MRI evaluation. Concomitant ABC-like changes can predispose the bone to pathological fractures. They can be easily missed on the radiograph and present as a diagnostic dilemma with MRI as the problem-solving tool. Wahab et al. reported a case of FD of femur and tibia where the pre-operative diagnosis of FD alone was made, and post-surgical histopathological examination revealed concomitant ABC-like changes.[3] The lack of pre-operative MRI of the patient may have been the reason for missing the diagnosis. Lee et al. reported concomitant FD with ABC formation in the skull, humerus, and rib.[4] In our case, the rest of the skeletal survey was unremarkable, thus representing a monomelic polyostotic FD with ABC-like changes.
CONCLUSION
Concurrent FD with ABC-like changes is relatively uncommon with most of such cases reported involving the craniofacial bones. Radiograph or CT scan evaluation can miss the concomitant ABC-like changes that are best depicted on MRI with classical fluid-fluid levels. Knowledge of this entity can help in accurate diagnoses and tailoring the treatment protocol of patients to avoid inadvertent intraoperative complications.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Update on aneurysmal bone cyst: pathophysiology, histology, imaging and treatment. Pediatr Radiol. 2022;52:1601-14.
- [CrossRef] [PubMed] [Google Scholar]
- Case report of a young girl with fibrous dysplasia (FD) concomitant with secondary aneurysmal bone cyst (ABC) J Pak Orthop Assoc (JPOA). 2023;35:23-7.
- [Google Scholar]
- Secondary aneurysmal bone cyst in a craniofacial fibrous dysplasia: Case report. Brain Tumor Res Treat. 2018;6:86-91.
- [CrossRef] [PubMed] [Google Scholar]







