Translate this page into:
Imaging in a case of classic Trevor’s disease

*Corresponding author: Aruna R. Patil, Department of Radiology, Apollo Hospitals, Bengaluru, Karnataka, India. dr.arunarpatil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil AR, Javalgi A, Babu M, Shivakumar S. Imaging in a case of classic Trevor’s disease. Indian J Musculoskelet Radiol 2021;3:133-6.
Abstract
Trevor’s disease, also known as dysplasia epiphysealis hemimelica, is a rare developmental bone dysplasia, characterized by benign osteocartilaginous overgrowth pathologically indistinguishable from osteochondroma. The lesion arises from epiphysis more so on the medial aspect of long bones resulting in painless or painful deformities and limb length discrepancies. Imaging plays an important role in diagnosis as the features are characteristic in an appropriate demographic background. We report a case of Trevor’s disease in a 2-year male with multifocal involvement and characteristic imaging findings.
Keywords
Trevor’s
Dysplasia
Epiphyses
Hemimelica
Imaging
INTRODUCTION
Trevor’s disease, also known as dysplasia epiphysealis hemimelica (DEH), is a rare, non-hereditary epiphyseal disease of unknown etiology and sporadic origin that simulates osteochondromatosis in the synovial joints. The most commonly involved sites are the lower limb, ankle followed by the knee. Most cases are painless, presenting with gradual deformity and limitation of motion of the affected joint. Radiographs are useful for the initial diagnosis with magnetic resonance imaging (MRI) adding to a better understanding of the pathophysiology.
CASE REPORT
A 2½-year-old male child presented with unilateral right knee and ankle swelling, occasional pain, and limitation of movements around the knee joint. Radiographs of both knee and right ankle showed lobulated bony growth on the medial aspect of the right knee inferior to the distal femoral condyle epiphyses. No obvious continuity with the native bone was seen. Genu valgum deformity of the right knee was noted. Similar findings were seen in the right ankle with bony outgrowths related to medial distal tibial epiphyses and talus [Figure 1a and b]. Genu valgum correction was attempted and follow-up radiographs after 10 months showed an interval increase in the size of the medial knee bony mass [Figure 2]. MRI of the right knee demonstrated multiple conglomerate bony fragments related to the lower femoral epiphyses medially with cartilage continuity around the fragments. The bony fragments showed normal marrow signals like the native bone [Figures 3 and 4]. Cartilage cap had typical chondral characteristics appearing hyperintense on T2 and intermediate signal on T1. A final diagnosis of DEH, classic type was made as there was involvement of two epiphyses (knee and ankle) in a single limb. The patient underwent resection of the lesion. The histology of resected part showed features of osteochondroma with orderly arrangement of chondrocytes within the cartilage cap along with mature marrow adipocytes. Mitoses were not seen. The histopathological diagnosis was a benign osteochondroma [Figure 5]. The patient is on regular follow-up.
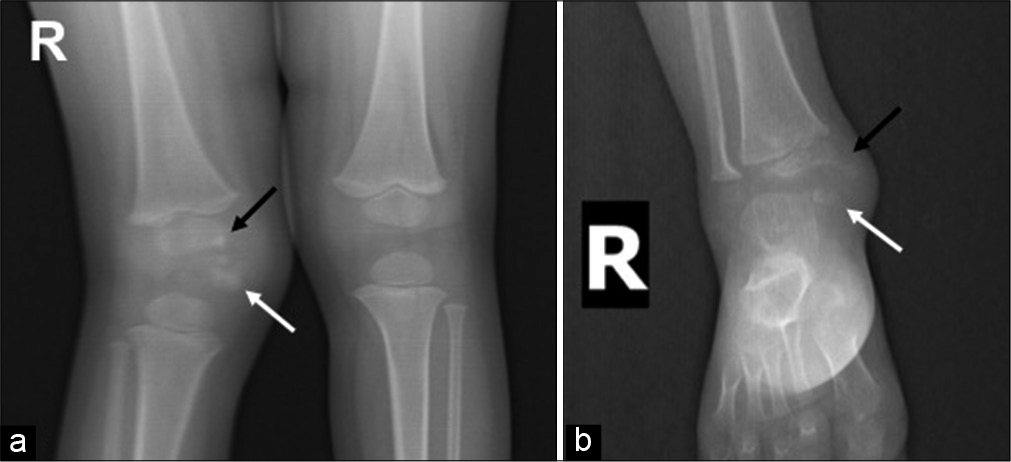
- (a) Anteroposterior radiograph of both knee joints shows a lobulated irregular bony lesion in the medial knee (white arrow) with irregularity of medial aspect of femoral epiphyses (black arrow) along with genu valgum deformity. (b) Similar findings were seen in the ankle region with the bony lesion (white arrow) and irregular lower tibial epiphyses medially (black arrow).

- Anteroposterior and lateral views of the right knee after 10 months show interval increase in the size of the bony lesion (white arrow). Genu valgum correction screws noted.
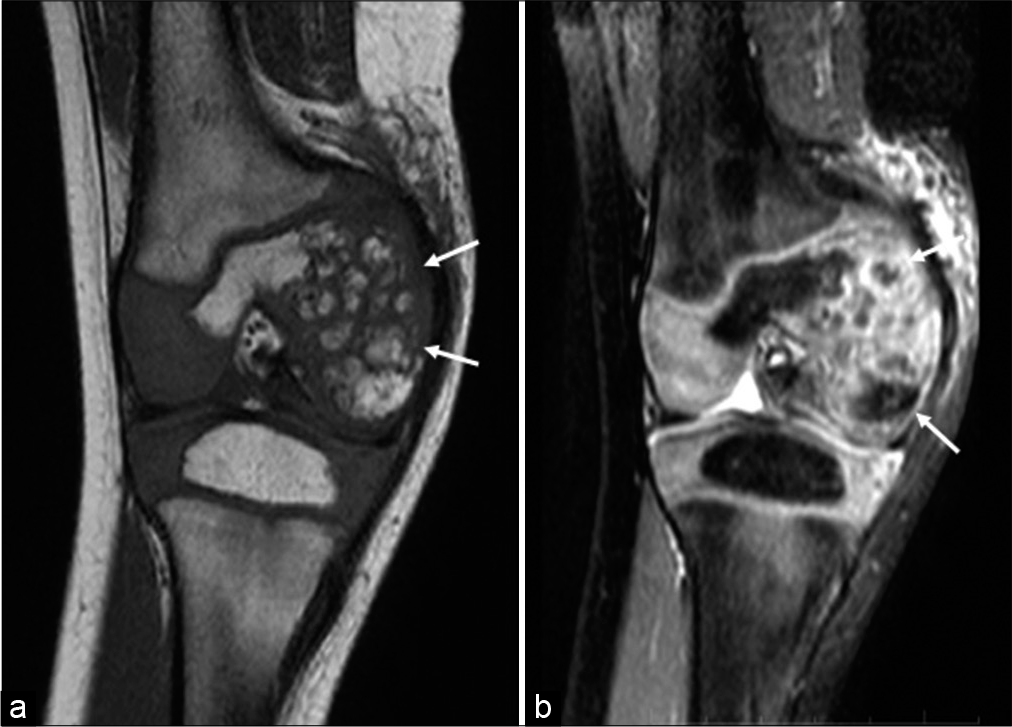
- Coronal T1 (a) and PD fat-saturated sequences (b) show multiple conglomerate bony fragments related to the lower femoral epiphyses medially (white arrows) with cartilage continuity around the fragments.
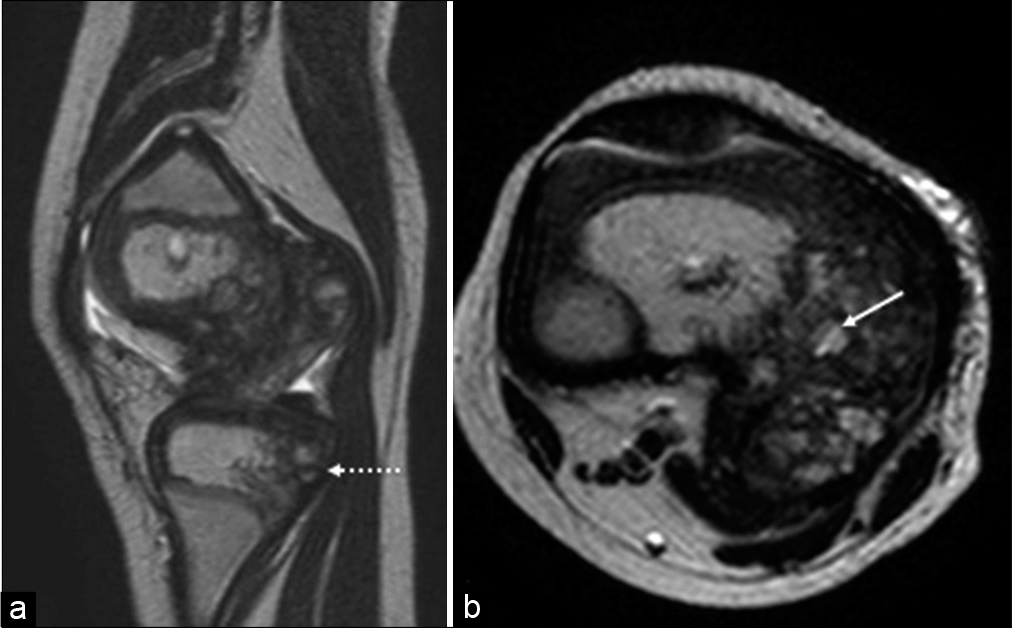
- Sagittal (a) and axial (b) T2-weighted image shows similar changes in upper tibial epiphyses (dotted arrow). The fragments show normal marrow signal (white arrow).
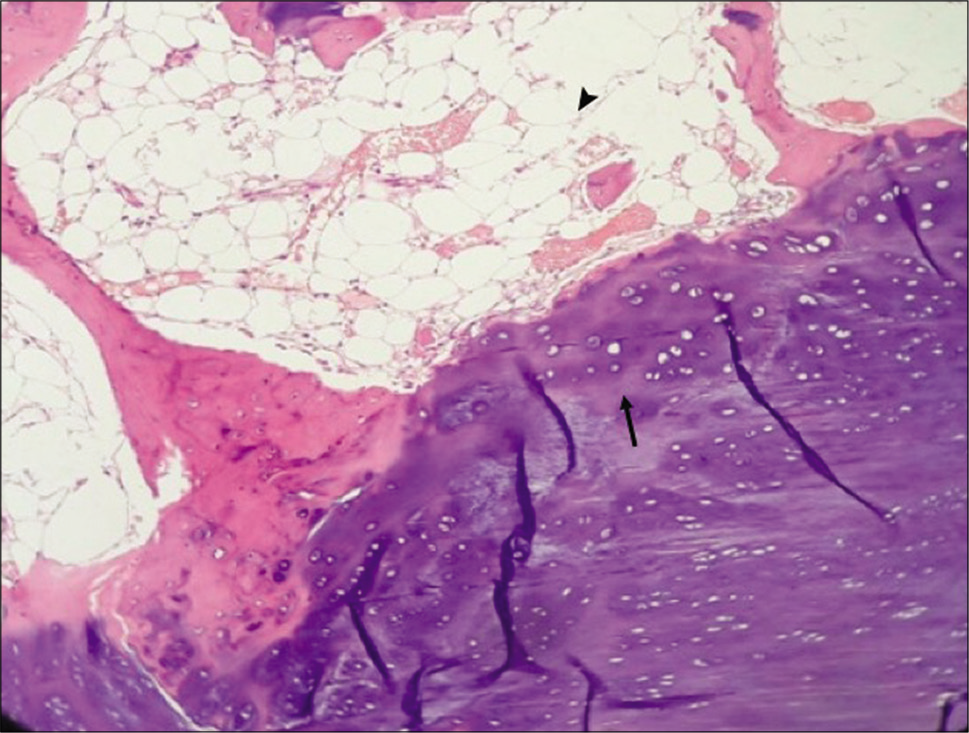
- Histopathology shows features of osteochondroma with cartilage capping (arrow) and mature marrow adipocytes (arrowhead).
DISCUSSION
DEH, also known as Trevor’s disease, is a non-hereditary disease that is characterized by osteochondromas arising from the epiphyses first described in 1926 by Mouchet and Belot as tarsomegaly.[1,2] It is also associated with extraskeletal osteochondromas, intracapsular chondromas, and sclerosing bone dysplasias.[1] The incidence is estimated at ~1:1,000,000. There is a recognized male predilection (M: F = 3:1) and usually presents in young children in the first decade of life.[1,2] Although DEH is thought of as epiphyseal osteochondromas, histologically it is comprised disorganized cartilage and unabsorbed cartilage fragments in contrast to more orderly process in osteochondromas. Furthermore, the EXT1 and EXT 2 gene pathways implicated in osteochondromas are not detected in DEH.[3]
The Azouz classification comprises three forms, localized, classic, and generalized. Localized type affects a single epiphysis whereas the classic form affects more than 1 epiphysis in the same limb and generalized type affects the entire lower limb. The classic type is the most common form. The medial side is affected twice as often as the lateral. Lower limbs are relatively favored with the distal femur, distal tibia, and talus being affected of frequency. Another recent classification by Arealis has six types and is based on joint involvement of upper, lower limbs and also takes into account any associated spine involvement.[4,5]
Radiographs are commonly the initial imaging investigation and usually are enough to make the diagnosis. The findings include asymmetrical enlargement of epiphyses with irregular or lobulated single or multiple masses with calcification or ossification arising from one side of the epiphyses. Irregular ossification centers are seen. They generally enlarge with skeletal growth and may be associated with the joint deformity. Eventually, they ossify and become confluent with the parent bone. Secondary involvement of metaphyses can result in undertubulation.[3,6] Skeletal surveys consisting of extremity radiographs can help in appreciating the asymmetry and asymptomatic lesions and also rule out sinister mimickers.[3]
CT is very sensitive to calcific and ossific components and to delineate the abnormal growth from normal secondary ossification centers and also to demonstrate the continuity of the growth with the medullary cavity. CT also helps in identifying the cleft between the DEH lesion and normal appearing ossification center aiding in surgical resection.[3,5-7]
MRI is preferred to evaluate the unossified cartilage mass in its entirety, to assess relation to neurovascular structures, tendons aiding in surgical planning. Cartilage appears T2 hyperintense and T1 iso-hypointense on MRI and hence can delineate clefts between normal ossification centers, physes, and the abnormal mass. Sometimes, the T2 signal is more hyperintense than normal cartilage reflecting disorganization histologically. The physeal integrity is additionally well assessed on MRI which can aid in surgical planning. It can also be used for post-surgical follow-up and early changes of secondary osteoarthrosis. The use of gadolinium is controversial and generally does not add to any additional advantage.[3,6] Some authors recommend whole-body MRI for detecting additional lesions.[8]
Imaging diagnosis is usually straightforward. Differentials include osteochondroma, metachondromatosis, synovial osteochondromatosis, and parosteal osteosarcoma. DEH normally originates from the epiphysis but the osteochondroma originates from the metaphysis of the bone and has a well-defined contour with a cartilage cap with medullary continuity. Dominant carpotarsal osteochondromatosis, a type of hereditary osteochondromatosis characterized by epiphyseal osteochondromas shares similar imaging features with DEH, is another close differential. The irregular calcific or ossific areas in DEH can mimic sinister lesions like parosteal osteosarcoma.[3,7,9,10]
Since the DEH lesions grow with skeletal growth, resultant joint deformities and limb length discrepancies require timely surgical intervention. Asymptomatic lesions can be treated non-operatively, as there is no known reported case of malignant transformation.[1,4] Resection is an accepted procedure with good outcomes.[3] Controversy exists for intra-articular lesions as resection may increase the risk of degenerative joint disease.[9,10]
CONCLUSION
DEH is a rare, sporadic non-hereditary dysplasia characterized by irregular osteochondral growths predominantly unilateral lower limb extremities. Imaging features are characteristic with MRI offering an additional advantage in surgical planning and understanding the disease process. Resection is generally favored to prevent deformities and limb length discrepancies.
Acknowledgments
Dr. Himaja Makineni, Dr. Shrivalli Nandikoor, Department of Radiology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Trevor disease (hemimelic epiphyseal displasia): 12 year follow-up case report and literature review. Ann Med Health Sci Res. 2014;4(Suppl 1):S9-13.
- [CrossRef] [PubMed] [Google Scholar]
- More than epiphyseal osteochondromas: Updated understanding of imaging findings in dysplasia epiphysealis hemimelica (Trevor disease) AJR Am J Roentgenol. 2018;211:910-9.
- [CrossRef] [PubMed] [Google Scholar]
- The variable manifestations of dysplasia epiphysealis hemimelica. Pediatr Radiol. 1985;15:44-9.
- [CrossRef] [PubMed] [Google Scholar]
- Trevor's disease: A literature review regarding classification, treatment, and prognosis apropos of a case. Case Rep Orthop. 2014;2014:940360.
- [CrossRef] [PubMed] [Google Scholar]
- Best cases from the AFIP: Dysplasia epiphysealis hemimelica of the patella. Radiographics. 2006;26:581-6.
- [CrossRef] [PubMed] [Google Scholar]
- Case report of imaging analyses of the dysplasia epiphysealis hemimelica (Trevor's disease) J Korean Soc Radiol. 2013;69:149-52.
- [CrossRef] [Google Scholar]
- Trevor's disease and whole-body MRI. Eur J Radiol. 2011;79:363-4.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and surgical treatment of dysplasia epiphysealis hemimelica. A report of nine cases. Orthop Traumatol Surg Res. 2014;100:941-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dysplasia epiphysealis hemimelica (Trevor's disease): 7 of our own cases and a review of the literature. Acta Orthop. 2007;78:856-61.
- [CrossRef] [PubMed] [Google Scholar]






