Translate this page into:
MRI as an aid to diagnosis of scurvy in absence of classic clinical and radiographic signs

*Corresponding author: Hirva Manek, Department of Radiology, Bai Jerbai Wadia Hospital for Children, Mumbai, Maharashtra, India. hirvamanek@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Manek H, Gala F. MRI as an aid to diagnosis of scurvy in absence of classic clinical and radiographic signs. Indian J Musculoskelet Radiol. 2023;5:135-9. doi: 10.25259/IJMSR_28_2023
Abstract
Scurvy, a Vitamin C deficiency disorder leads to impaired synthesis of collagen, osteoid, and dentine, causing cutaneous, dental, and skeletal manifestations, respectively. The radiographic features of scurvy are very well established but the increasing use of magnetic resonance imaging (MRI) in limb pathologies warrants radiologists to be aware of its common as well as atypical magnetic resonance findings. Two children who presented with pain and swelling of the thigh and were proven to have scurvy were included in the study. The first child had cerebral palsy and MRI was performed as radiographs were suspicious for physeal subluxation. MRI confirmed physeal separation of the distal femur with subperiosteal collection. The second patient was developmentally normal and had non-traumatic painful thigh swelling. Radiographs showed a fracture at the distal metaphyseal–diaphyseal junction of the femur. Subperiosteal collection and surrounding muscle edema with heterogenous marrow signal were seen in both the patients on MRI. Inflammatory markers were normal. Follow-up with radiographs after treatment with vitamin C supplementation showed ossification of the subperiosteal hematomas and resolution of the symptoms. These two cases highlight the significance of MRI in reaching a diagnosis in atypical cases of scurvy which has excellent response to Vitamin C supplementation.
Keywords
Scurvy
Magnetic resonance imaging
Fracture
Physis
Hemorrhage
INTRODUCTION
Scurvy, a nutritional deficiency disorder is caused by inadequate intake of the essential micronutrient, Vitamin C. It is rare in the current times but is still encountered in children with risk factors such as cerebral palsy, picky eating behaviors, developmental delay, and in uncommon situations in developmentally normal children as well.[1-3] Vitamin C is essential in collagen synthesis in skin, blood vessels, and connective tissue and its deficiency leads to bleeding diathesis and musculoskeletal complaints. Radiographic features of scurvy are very well-known and extensively described in the literature for many years. However, with the increasing use of advanced imaging modalities such as magnetic resonance imaging (MRI), it is inevitable to know the imaging features of this new old nutritional deficiency disorder.
CASE SERIES
Case 1
A 10-year-old male child was presented with chief complaints of swelling of the left thigh and knee with a paucity of limb movements. On examination, the swelling was warm, tender, and showed redness of the overlying skin. The child was developmentally delayed secondary to a complication of the pediatric inflammatory multisystem syndrome (PIMS) in early childhood. Clinically, there were no signs of petechial rashes, gum or mucosal bleeding, or joint swelling. His inflammatory markers were mildly elevated whereas the total white blood cell (WBC) count was normal. Despite these lab findings, a clinical suspicion of septic knee or underlying left femur osteomyelitis was raised. A radiograph of the knee was obtained in orthogonal projections. The radiographs showed mild osteopenia with suspicious physeal subluxation on the lateral radiograph [Figure 1]. Further evaluation with multiplanar MRI was done [Figure 2a and b]. The findings were grotesque on MRI which confirmed distal femoral physeal separation with impingement of the metaphysis on the epiphysis. The marrow of the femur appeared homogenous except for some edema at the site of metaphyseal impingement on the epiphysis. There was an associated large subperiosteal heterogenous collection along the entire shaft of the femur. The collection showed T1 and T2 hyperintensity. A limited computed tomography scan was also performed which showed a thin discontinuous peripheral rim of calcification [Figure 2c]. A suspicion of scurvy was raised based on these findings and the referring pediatric orthopedic surgeon was notified. Serum Vitamin C levels confirmed scurvy and the child was managed with Vitamin C supplementation and limb splint for pain relief and healing. A follow-up radiograph after 2 months showed calcification of the subperiosteal hematoma Figure 3 and the child improved symptomatically on 6 months follow-up.

- A 10-year-old male child with developmental delay presented with left thigh swelling (a) Frontal radiograph of the left knee shows mild osteopenia. (b) The lateral radiograph shows mild subluxation of the distal femur epiphysis with a step in the level between the epiphysis and the metaphysis (white arrow).

- A 10-year-old male child with developmental delay presented with the left thigh swelling (a) short T1 inversion recovery (STIR) sagittal image shows physeal separation with a large circumferential heterogenous hyperintense subperiosteal hematoma (star) around the femur shaft. (b) The hematoma is hyperintense on the sagittal T1-weighted image (star). (c) Computed tomography sagittal image shows anterior subluxation of the shaft of the femur over the physis with metaphysis impinging on the epiphysis. A thin peripheral rim of calcification along the surrounding soft tissue (black arrows).

- Follow-up at 2 months after Vitamin C supplementation (a) Frontal and (b) Lateral radiographs of the left femur show ossification of the subperiosteal hematoma (white arrowheads) with persistent anterior subluxation.
Case 2
A 14-year-old female child presented with acute painful swelling of the left thigh. She had ipsilateral skin melanosis and vascular malformation due to phacomatosis pigmentosa vascularis. Her development was normal. She did not show any signs of petechial rashes, joint swelling, or gum or mucosal bleeding. There was no history of trauma or other signs of abuse. A possibility of infection was thought of initially. The inflammatory markers were mildly raised whereas the total WBC count was normal. A radiograph of the left thigh in orthogonal planes showed an oblique displaced fracture of the distal metaphysis of the left femur. To rule out underlying pathological lesion, a multiparametric MRI was performed [Figure 4]. It revealed circumferential T1 isointense and T2 heterogenous subperiosteal collection around the fracture site with mild knee joint effusion. No underlying pathological mass lesion was evident. The presence of non-traumatic fracture with subperiosteal collection raised a possibility of scurvy over osteomyelitis. Serum Vitamin C levels confirmed scurvy and the patient was treated with surgical fixation of the fracture and Vitamin C supplementation. Follow-up radiographs after 2 months showed calcification of the subperiosteal hematoma Figure 5, suggesting a response to treatment.

- Fourteen years old developmentally normal female child with pain and swelling of left thigh (a) Frontal and (b) lateral radiographs of the left knee show an oblique displaced fracture through the distal diaphysis of the femur with osteopenia of the bones. No obvious underlying lytic expansile lesion. (c) T1-weighted sagittal and (d) short T1 inversion recovery sagittal images confirm distal femur metaphyseal fracture without any underlying lesion. Circumferential subperiosteal hematoma and intramedullary hemorrhage are seen at the site of fracture (white arrow). Mild knee joint effusion.
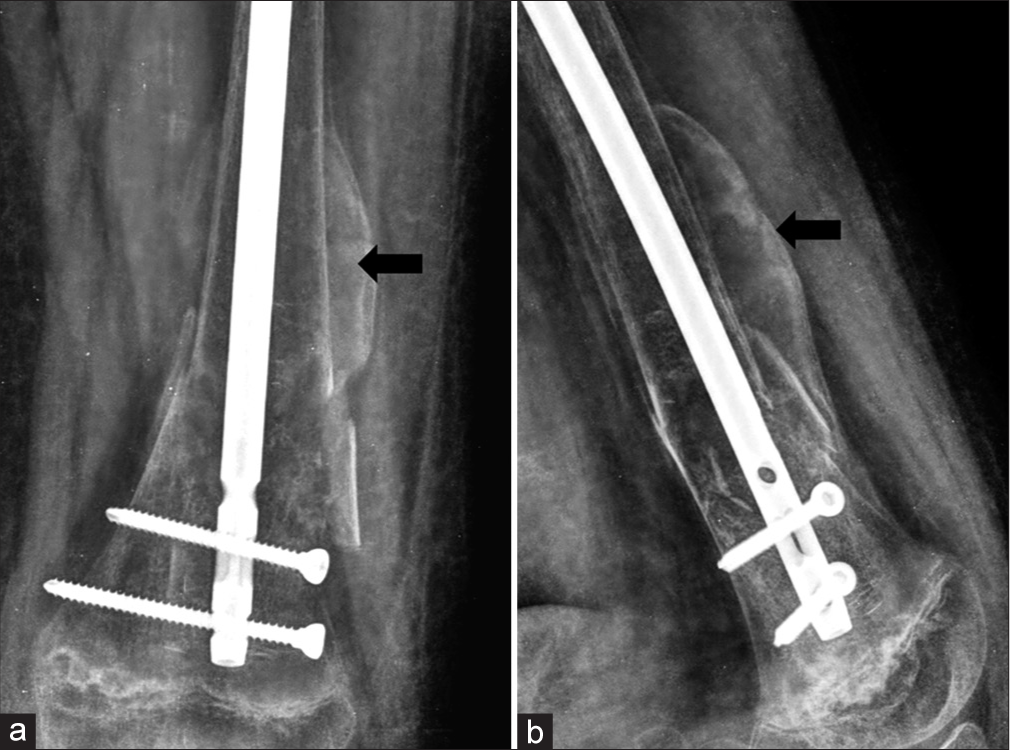
- Follow-up 2 months after surgery and Vitamin C supplementation (a) Frontal and (b) lateral radiographs of the left femur show ossification of the subperiosteal hematoma (black arrow). Metallic implant in situ.
DISCUSSION
Vitamin C is an essential vitamin in humans and its deficiency can lead to scurvy. Vitamin C is passively absorbed from the small intestine and the excess is excreted through the renal route. Hence, excessive intake of Vitamin C does not lead to overdose. Deficiency of this essential micronutrient leads to defective synthesis of type II collagen resulting in gingival inflammation, hypertrophy and bleeding, cutaneous purpura, defective osteoid synthesis, osteopenia, subperiosteal, and intraosseous hemorrhages.[2]
Typical radiographic findings of scurvy are well established for many years. These include metaphyseal lucent bands (trummerfeld zone), white line of Frankel above the lucent line, Wimberger sign of dense epiphyseal ring, and metaphyseal irregularity or metaphyseal fractures (pelkan spur).[2] These findings are characteristic of scurvy but are not always seen. The presence of normal to near normal radiographs is not unlikely even in cases of severe Vitamin C deficiency.[1-3]
The first child in our case report was an at-risk child with developmental delay. However, both patients did not have the typical signs and symptoms of Vitamin C deficiency like cutaneous purpura, gum hypertrophy, or bleeding. Physeal separation is a known complication of severe Vitamin C deficiency and similar reports have been published in literature but in all these cases the physeal subluxation was well evident on the radiographs and MRI was not performed.[4,5]
The magnetic resonance (MR) findings in scurvy have been described in multiple case reports where the radiographs were normal.[1,2,6,7] These early MR findings usually include multifocal marrow edema involving the metaphyses of the long bones which could be symmetric or asymmetric. This is associated with circumferential periosteal elevation, subperiosteal edema, and adjacent soft tissue inflammation. This metaphyseal signal correlates with the lucency due to osteopenia seen on radiographs. These MRI changes when multifocal can raise a suspicion of chronic recurrent osteomyelitis when associated findings such as hematoma or physeal separation are not present.[8] Correlation with the laboratory markers and Vitamin C levels can be of further value in such presentations.
The second case in our case report had normal neurodevelopment and phacomatoses pigmentosa vascularis affecting the left lower limb. This child was presented with painful tender unilateral thigh swelling mimicking underlying infection, but the radiograph of the thigh showed a metaphyseal fracture in the absence of any history of trauma. MRI findings of intraosseous and subperiosteal hemorrhages raised a possibility of scurvy in this case.
Although physeal separation is known in severe cases of hypovitaminosis C, metaphyseal fracture due to scurvy is not reported in recent times. The only similar case we found was in the Lancet article of 1897 which discusses shaft fractures in children with scurvy.[9] In another article by Sutherland, it was postulated that subperiosteal hemorrhage due to bleeding diathesis in scurvy causes periosteal stripping and deprives the underlying bone of nutrition, making it brittle. The other hypothesis was that fracture causes perifocal hemorrhagic extravasation.[10] He also suggested that in such fractures of scurvy, there was usually an absence of concomitant marked rachitic changes of Vitamin D deficiency in bones. Classical radiograph signs of rickets were absent in both of our patients.
MRI as a cross-section imaging tool is of value in atypical scurvy cases as the heterogenous signal of hematomas in the medullary cavity and beneath the periosteum helps it to differentiate it from the subperiosteal abscess of osteomyelitis. Furthermore, a higher T1 signal of blood than abscess and the absence of cortical thickening or erosions are other diagnostic clues. Adjacent soft-tissue inflammation is a non-specific finding and can be seen in both the differentials. Thus, we conclude that MRI in atypical settings can hint at an underlying diagnosis. We do not recommend MRI in typical cases of scurvy as radiographs remain the choice of investigation for diagnosis and for evaluating the treatment response.
CONCLUSION
Radiograph is the mainstay investigation in children presenting with skeletal pathologies and it gives away the diagnoses in the majority of cases. Scurvy is one such pathology for which the radiograph findings are extensively described. However, normal radiographs can be seen in scurvy, and it is in such atypical cases that MRI helps in reaching a diagnosis. With the increasing use of MR in children presenting with limp, limb swelling, and pain, it is also imperative to be aware of the findings of this uncommon nutritional deficiency disorder. Once properly diagnosed, this clinically grave looking disorder can be managed by vitamin supplementation and limb management with excellent prognosis and minimal to absent residual deformity.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Modern day scurvy in pediatric orthopaedics: A forgotten illness. J Pediatr Orthop. 2021;41:e279-84.
- [CrossRef] [PubMed] [Google Scholar]
- Scurvy: A new old cause of skeletal pain in young children. Front Pediatr. 2020;8:8.
- [CrossRef] [PubMed] [Google Scholar]
- Scurvy: A neglected cause of muscle pain and weakness in a child with picky eating behavior. Cureus. 2021;13:e16289.
- [CrossRef] [Google Scholar]
- Epiphyseal separations in spastic cerebral palsy. J Pediatr Orthop B. 2007;16:170-4.
- [CrossRef] [PubMed] [Google Scholar]
- Scurvy: An unusual presentation of cerebral palsy. World J Orthop. 2012;3:58.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric scurvy MRI appearance. Radiol Case Rep. 2021;16:1148-52.
- [CrossRef] [PubMed] [Google Scholar]
- Scurvy in a pediatric patient with autism and limp: A case report. J Emerg Med. 2021;60:e53-6.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging mimics of chronic recurrent multifocal osteomyelitis: Avoiding pitfalls in a diagnosis of exclusion. Pediatr Radiol. 2020;50:124-36.
- [CrossRef] [PubMed] [Google Scholar]







