Translate this page into:
Mueller Weiss syndrome, a less elucidated and unusual cause of midfoot pain: A case report

*Corresponding author: Veena Mariam Joseph, Department of Radiology and Imaging, North Eastern Indira Gandhi Institute for Health and Medical Sciences, Shillong, Meghalaya, India. josveena@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Joseph VM, Lynser D, Khan AY, Daniala C. Mueller Weiss syndrome, a less elucidated and unusual cause of midfoot pain: A case report. Indian J Musculoskelet Radiol 2021;3:94-7.
Abstract
Mueller Weiss Syndrome is a rare, under-diagnosed cause of chronic mid foot pain despite having well-described imaging features. It is historically described as spontaneous adult-onset osteonecrosis of the navicular bone. The disease commonly affects bilateral navicular bones in women in the fifth decade of life. Nearly a century after its first description as a disease entity, the exact etiopathogenesis is still not well understood. From a radiographic point of view weight-bearing radiographs of the foot remains the mainstay in diagnosis. Characteristic imaging findings include the lateral collapse of navicular, dorsomedial subluxation of the remnant navicular, and lateral deviation of the talus (hind-foot varus). Progressive disease leads to pes planus and secondary osteoarthritis of the talonavicular joint with or without the involvement of other midfoot joints. Severe disease may show “listhesis navicularis” and talo-cuneiform neo-articulation. Computed tomography and magnetic resonance imaging can be used as adjuncts, especially to detect changes in the initial stage of the disease and early osteoarthritic features.
Keywords
Mueller Weiss syndrome
Talo-navicular joint
Meary Tomeno angle
Navicular osteonecrosis
Comma shaped deformity
INTRODUCTION
MuellerWeiss Syndrome is the eponym for adult-onset spontaneous osteonecrosis of navicular bone causing mid and hindfoot pain and deformity.[1] Early recognition and management can control symptoms and delay progression of the disease and secondary osteoarthritis. We present a case report of a patient diagnosed with Mueller Weiss Syndrome, having typical imaging features but presenting at a relatively younger age of onset.
CASE REPORT
A 34-year-old woman presented with insidious onset, progressively increasing bilateral asymmetric dorsomedial midfoot pain for 4 months. There was no history of recent trauma or systemic diseases. On examination, there was swelling and tenderness over the talonavicular joint (Right > Left). Routine blood investigations like complete blood count were unremarkable. The patient underwent weight-bearing radiographs followed by computed tomography and magnetic resonance imaging of both feet [Figures 1-3].

- Anteroposterior Radiograph of the right foot (a) and left foot (b) showed-(1) Collapse of the lateral portion of navicular bone with resultant comma-shaped deformity. (2) Loss of cyma line (‘S’ shaped line along the talonavicular and calcaneocuboid articular surface which indicates normal alignment. (3) Peri-talar (i.e., medial) subluxation of the remaining navicular fragment with respect to the head of the talus. (4) Subchondral sclerosis of the articular surface of the tarsal navicular. Lateral radiograph of the right foot (d) and left foot (e) showed- (1) Reduction in the navicular height in AP dimension (2) Subchondral sclerosis of the talo-navicular articular surface of navicular bone (3) Asymmetry of the talonavicular joint space with apparent widening of the dorsal aspect (4) Anterior marginal osteophytes at the talonavicular joint. Anteroposterior (c) and lateral (f) radiographs of normal foot is provided for comparison.
![Sagittal unenhanced computed tomography images of the ankle with foot [Right (a) and left (b)] showed findings similar findings as radiography, including bilateral reduction in size of the tarsal navicular with asymmetric reduction of the talonavicular joint space and anterior marginal osteophytes. The angle between the long axis of the first metatarsal and talus (Meary Tomeno angle) was calculated and measured on unenhanced computed tomographic images of bilateral feet in sagittal view (bone window). It measured 4 degrees on the right (c) and 2 degrees on the left (d).](/content/107/2021/3/2/img/IJMSR-3-094-g002.png)
- Sagittal unenhanced computed tomography images of the ankle with foot [Right (a) and left (b)] showed findings similar findings as radiography, including bilateral reduction in size of the tarsal navicular with asymmetric reduction of the talonavicular joint space and anterior marginal osteophytes. The angle between the long axis of the first metatarsal and talus (Meary Tomeno angle) was calculated and measured on unenhanced computed tomographic images of bilateral feet in sagittal view (bone window). It measured 4 degrees on the right (c) and 2 degrees on the left (d).
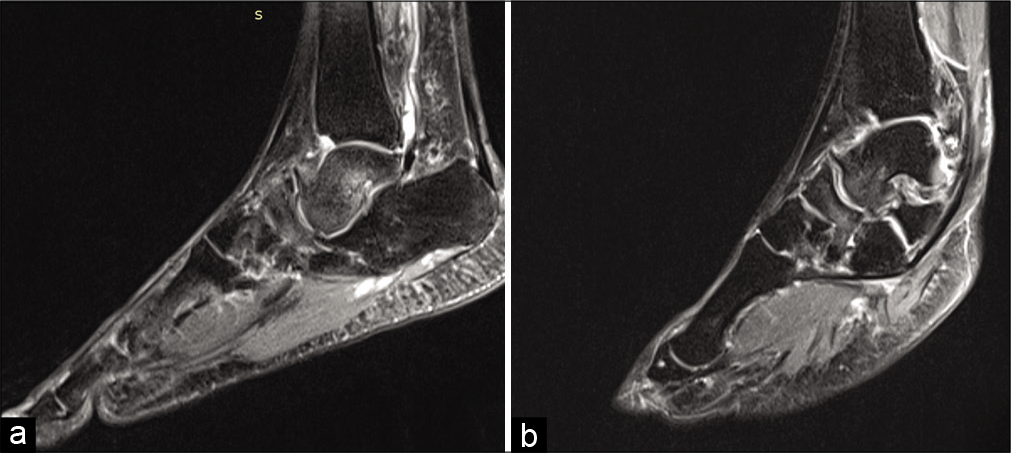
- Right (a) and Left (b) Sagittal short tau inversion recovery sequence Magnetic resonance images showed diffuse high signal intensity within the body of Navicular and head and neck of the talus suggestive of marrow edema which can be attributed to secondary talonavicular osteoarthritis.
Based on an isolated clinical background of bilateral chronic midfoot pain and typical imaging features, the diagnosis of Mueller Weiss Syndrome in this patient is well substantiated. However, being an infrequent cause of this symptom, on a case-to-case basis, there is a need for increased awareness of this entity both among treating clinicians as well as diagnosticians.
DISCUSSION
Historically, MuellerWeiss Syndrome has been described as spontaneous adult-onset osteonecrosis of the tarsal navicular. The exact etiopathogenesis is unknown, however, studies have proposed that factors leading to persistent lateral loading on a sub-optimally ossified navicular bone which is prone to ischemia is contributory.[1]
Most commonly the presentation is as chronic mid/ hindfoot pain in a middle-aged (40–60 years) female.[2] The presentation was atypical in the above-mentioned case both in terms of age of onset and chronicity, in that, the patient was younger and had a relatively subacute duration of onset of symptoms. Physical examination may reveal high, low, or normal arching of the feet. In this patient, there was maintained plantar arch as evident by physical examination and calculation of Meary Tomeno angle. Imaging features are multiple and hence clarity is achieved if classified based on the anatomic location [Table 1].
| Anatomic part | Involvement in this case |
|---|---|
| Ankle and hindfoot 1. Collapse of the lateral part of the navicular (Comma shaped deformity) 2. Peritalar (medial) subluxation of the navicular (loss of cyma line) 3. Reduction of Talocalcaneal angle (Kite’s angle) |
+ + – |
| MID Foot 1. Talocuneiform articulation 2. Osteoarthrosis of Talonavicular and Naviculocuneiform Joints 3. Medial subluxation of the cuboid (with respect to calcaneum) |
– +(Talonavicular) – |
| Forefoot 1. Parallel metatarsals 2. Hypertrophy of second metatarsal |
– – |
According to the Staging proposed by Maceira and Rochera[2] based on the morphology of the Navicular combined with the Meary Tomeno angle, the patient was staged as bilateral Stage II MuellerWeiss Syndrome [Table 2]. The Staging along with the severity of symptoms, helps the clinicians determine the appropriate line of management.
| Stage of Disease (degree of severity) | Description |
|---|---|
| 1. Mild | Radiographs are normal |
| 2. Moderate | Dorsolateral subluxation of the talus resulting in cavus and hindfoot varus with rostral angulation of the Meary- Tomeno line |
| 3. | Condensation or splitting of the navicular leading to reduction of the longitudinal arch and neutral Meary- Tomeno line |
| 4. Severe | Compression of the navicular leading to rearfoot equinus deformity, further reduction of longitudinal arch and caudal angulation of the Meary Tomeno line |
| 5. | Talo-cuneiform neoarticulation and expulsion of a disintegrated navicular(“ listhesis navicularis”) |
| Based on the Staging proposed by Maceira and Rochera[2] |
Kohler’s disease is another cause of spontaneous osteonecrosis of navicular bone that is attributed to navicular ossification variant or osteonecrosis. However, Kohler’s disease usually has a childhood-onset (3–7 years), male predominance, unilateral presentation, and a more benign disease progression. Imaging of Kohler’s disease shows flattening of the navicular and a central area of sclerosis that evolves from irregular to progressive uniform redistribution.[5] Navicular stress injury, osteonecrosis secondary to systemic diseases, osteomyelitis, healing phase of traumatic fracture, and initial stages of the neuropathic joint are the other differentials to be considered.[2,6] Most important factor to differentiate Mueller Weiss from this apparently long list of diagnosis, is a detailed clinical history and weight-bearing radiographic findings.
Conservative measures like anti-inflammatory drugs, activity- restriction, and immobilization with orthoses or short leg casts, fail to achieve adequate symptomatic relief in moderate to severe disease and in patients who have developed secondary osteoarthritis.[7] There is a myriad of available surgical options including decompression with or without bone grafting and multiple midfoot arthrodesis[7] but the exact intervention must be tailored to the involvement in the individual patient. Studies have showed satisfactory results with both talonaviculocuneiform arthrodesis with bone grafting and triple fusion arthrodesis. The latter is preferred in patients with additional subtalar and calcaneocuboid joint involvement.[8] However, a standardised surgical option for the management of this disease is not available to date.[7,9]
CONCLUSION
In a young female patient who presented with a subacute history of bilateral midfoot pain, the diagnosis of MuellerWeiss Syndrome could be clinched owing to its characteristic imaging features of the lateral collapse of navicular with resultant comma-shaped deformity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
References
- Imaging of mueller-weiss syndrome: A review of clinical presentations and imaging spectrum. AJR Am J Roentgenol. 2016;207:W8-18.
- [CrossRef] [PubMed] [Google Scholar]
- Müller-Weiss disease: clinical and biomechanical features. Foot Ankle Clin. 2004;9:105-25.
- [CrossRef] [Google Scholar]
- Mueller-Weiss syndrome: Imaging and implications. Clin Imaging. 2014;38:895-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic imaging of the Mueller-Weiss syndrome: Findings of a rare condition of the foot. J Am Podiatr Med Assoc. 2014;104:110-4.
- [CrossRef] [PubMed] [Google Scholar]
- The ossification and vascularisation of the tarsal navicular and their relation to Köhler's disease. J Bone Joint Surg Br. 1958;40B:765-77.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous osteonecrosis of the tarsal navicular in adults: imaging findings. AJR Am J Roentgenol. 1988;151:355-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fusion of talonavicular and naviculocuneiform joints for the treatment of Müller-Weiss disease. J Foot Ankle Surg. 2012;51:415-9.
- [CrossRef] [PubMed] [Google Scholar]
- Open triple fusion versus TNC arthrodesis in the treatment of Mueller-Weiss disease. J Orthop Surg Res. 2017;12:13.
- [CrossRef] [PubMed] [Google Scholar]







