Translate this page into:
Idiopathic chondrolysis of hip: A case report with literature review

*Corresponding author: Rushabh Bhikhabhai Suthar, Department of Radiology, Zydus Hospitals, Ahmedabad, Gujarat, India. rushabhb84@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Suthar RB, Thakkar T, Goswami G, Shukla Y. Idiopathic chondrolysis of hip: A case report with literature review.Indian J Musculoskelet Radiol. 2023;5:158-61. doi: 10.25259/IJMSR_32_2023
Abstract
Idiopathic chondrolysis of the hip (ICH) is a rare debilitating disease that results in articular cartilage loss in proximal femoral epiphysis and acetabulum; in the absence of a history of trauma, slipped capital femoral epiphysis, Perthe’s disease, prolonged immobilization, and infective/inflammatory joint diseases or malignancies. The diagnosis of chondrolysis of the hip is usually delayed due to the gradual onset of symptoms, initial normal radiographs, and the absence of specific diagnostic laboratory tests. Magnetic resonance imaging is the gold standard for the early diagnosis and grading of disease. ICH is often reversible with non-surgical management such as rest, alleviation of pain, and avoidance of weight-bearing. The clinical details and imaging appearance of this uncommon disease are discussed here.
Keywords
Chondrolysis
Proximal femoral epiphysis
Magnetic resonance imaging
Articular cartilage
INTRODUCTION
Idiopathic chondrolysis of the hip (ICH) is a rare debilitating illness that results in gradual loss of articular cartilage in the proximal femoral epiphysis and acetabulum; in the absence of a history of trauma, slipped capital femoral epiphysis, Perthe’s disease, prolonged immobilization, and infective/inflammatory joint diseases or malignancies. Undiagnosed or neglected cases can advance to severe joint space narrowing, osteoarthritis, protrusio acetabuli, and spontaneous ankylosis. ICH is frequently seen in adolescents (9–12-year-old children) and shows relative female predominance. It is generally monoarticular (60%) with less common (5%) bilateral joint involvement.[1] The patient presents with a painful hip with restriction of movements without an identifiable cause. The typical magnetic resonance imaging (MRI) features of our case enabled us to confirm the diagnosis.
CASE REPORT
A 12-year-old female child presented to the orthopedic outpatient department with complaints of pain and stiffness in her left hip, resulting in abnormal gait for the past two months. There was no history of injury, fever, malaise, or reduced appetite. The dull, aching pain in the left hip used to intensify with physical activity. The patient also complained of significant restriction of movement. Blood investigations, including complete hemogram, erythrocyte sedimentation rate, C reactive protein, rheumatoid arthritis factor, and human leukocyte antigenB27, were normal.
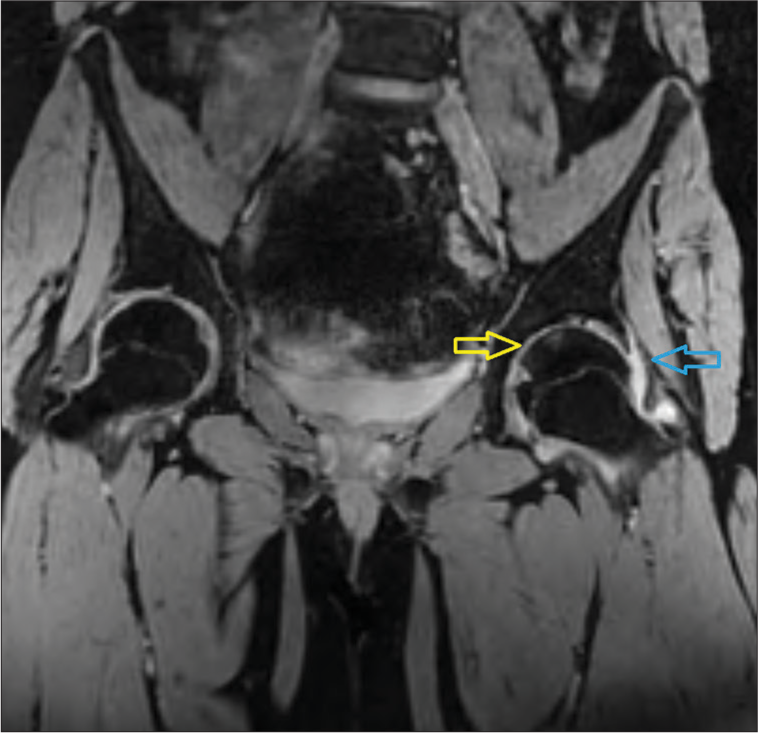
Her initial radiograph showed subtle contour irregularity of femoral epiphysis with <3 mm, concentric reduction in the left hip joint space [Figure 1]. MRI done at the same time revealed about 10 × 6 mm focal wedge-shaped T2, proton density fat suppression (PDFS), and short-tau inversion recovery (STIR) hyperintense and T1 hypointense bone marrow edema in the central third of the femoral epiphysis [Figures 2 and 3]. STIR coronal images showed focal areas of hyperintensity involving the femoral head and opposing acetabulum [Figure 4]. MERGE images showed mild cartilage loss overlying the central femoral head and acetabulum with moderately reduced joint space and mild left hip joint effusion [Figure 5]. There was no depression of the subchondral growth plate or erosions. MERGE or MEDIC is a T2* weighted spoiled gradient echo sequence used to look for fluid-filled spaces in the body (normal as well as pathological) and edema. A contrast study was not performed in this case due to the absence of any alarming non-contrast MRI features favoring aggressive infective or neoplastic etiology. The diagnosis of idiopathic chondrolysis of the hip was given after excluding clinical features, blood investigation reports, and radiological imaging features of all other common causes of cartilage loss.
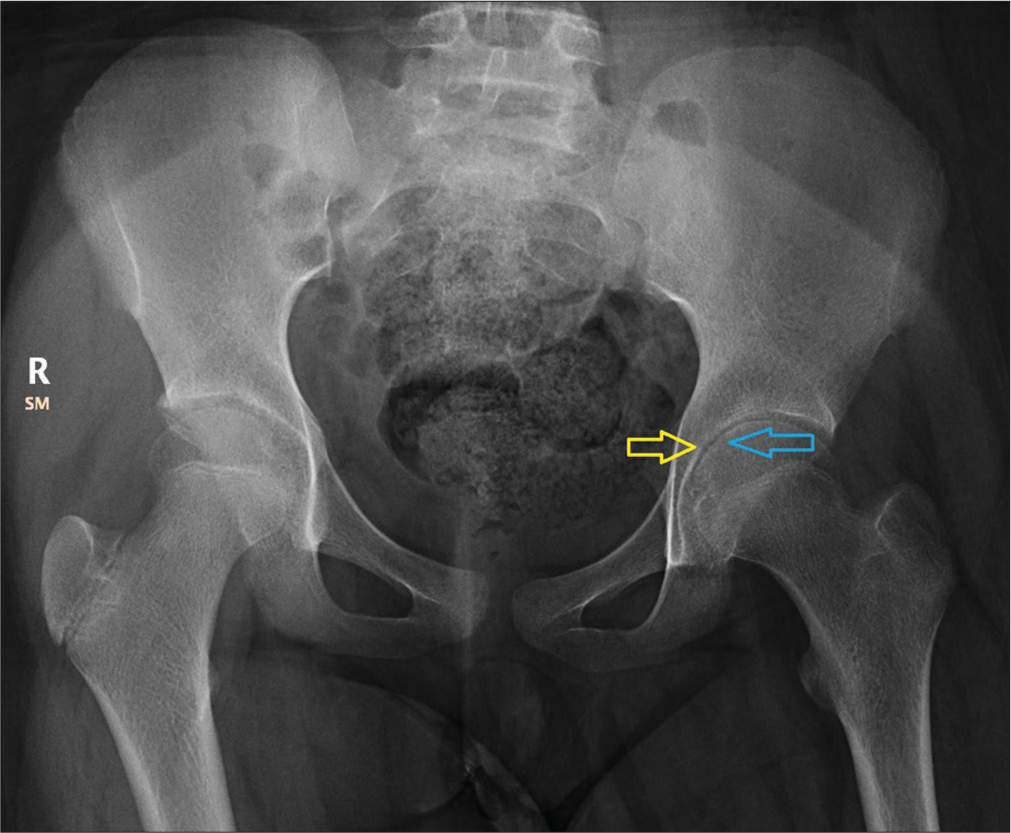
- Radiograph of the pelvis with both hips. The blue arrow shows subtle contour irregularity of femoral epiphysis. The yellow arrow shows <3 mm concentric reduction in the left hip joint space. The note is made of mild pelvic tilt to the left side.

- Sagittal proton density fat suppression image shows a focal wedge-shaped— area of hyperintensity involving the middle one-third of the femoral head.

- Sagittal short-tau inversion recovery image shows a focal wedge-shaped—area of hyperintensity involving the middle one-third of the femoral head with subtle hyperintensity in the opposing acetabulum.

- On the short-tau inversion recovery coronal image, the yellow arrow shows focal hyperintensity involving the middle one-third of the femoral head, and the blue arrow shows subtle focal hyperintensity in the apposing acetabulum.
- On the multiple echo recombined gradient echo coronal image, the yellow arrow shows mild thinning of articular cartilages over the left side femoral head and acetabulum, and the blue arrow shows mild synovial effusion involving the left hip joint.
The patient was managed nonsurgically with rest, alleviation of pain, and avoidance of weight-bearing. The patient responded exceptionally well to the conservative treatment. On the follow-up visit, the patient had no left hip pain and regained a normal range of left hip movement. A follow-up radiograph after three months showed a smooth contour of the femoral epiphysis with improved left hip joint space width. No obvious left pelvic tilt was noted – suggesting significant radiological improvement [Figure 6].
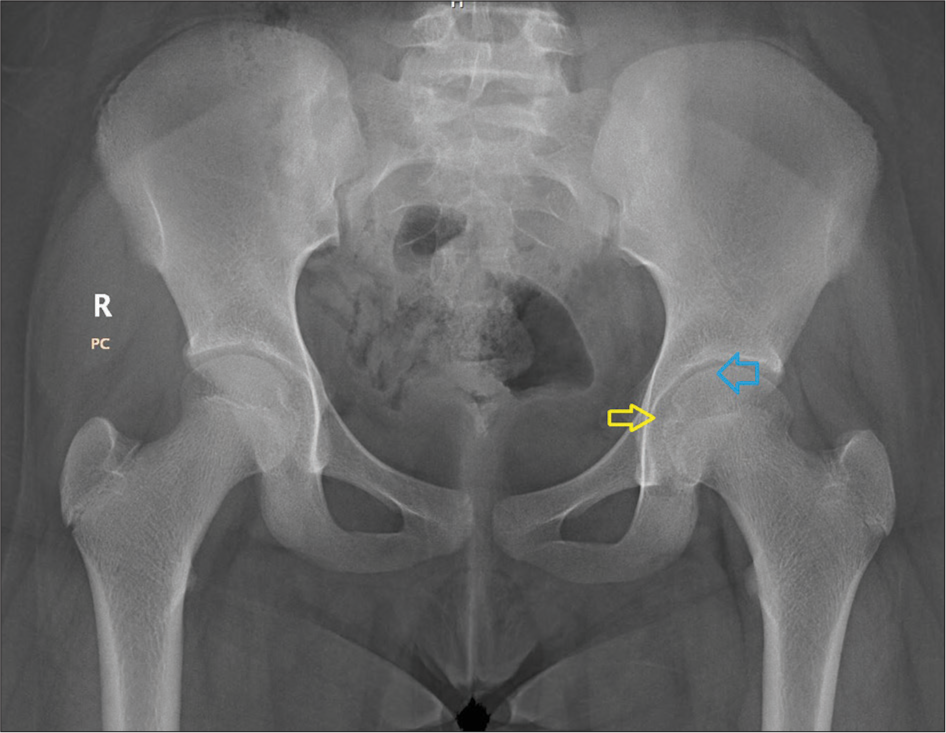
- Three-month follow-up radiograph of pelvis with both hips. The blue arrow shows a normal smooth contour of the femoral epiphysis. The yellow arrow shows improved left hip joint space width. No obvious left pelvic tilt was noted.
The response with conservative management confirmed the diagnosis of “Idiopathic chondrolysis of Hip.”
DISCUSSION
ICH results in the gradual loss of femoroacetabular articular cartilage in the absence of known and definable causes. In 1930, Waldenström[2] described chondrolysis of the hip in a patient suffering from slipped capital femoral epiphysis. Since then, this phenomenon has also been described in association with trauma, prolonged immobilization, Perthe’s disease, infective/inflammatory joint diseases, and malignancies.[3] Chondrolysis of the hip in the absence of a defined cause was first described by Jones[4], followed by Wenger DR[5] This entity is subsequently termed as “idiopathic chondrolysis of the hip.”
Initial radiographs of the hip are generally unremarkable. However, Bleck[6] described that some of the patients may show regional osteoporosis, blurred subchondral lines, and joint space reduction. Late radiographic changes include early closure of trochanteric and capital epiphyses, changes of osteoarthritis with secondary protrusio acetabuli, and fibrous or bony ankylosis.
MRI is the gold standard imaging modality for diagnosis and also to exclude certain other identifiable causes of hip pain. In the early stage, classical MRI findings show wedge-shaped/T2 hyperintense and T1 hypointense marrow edema involving the middle third of the proximal femoral head epiphysis.[7] This wedge-shaped focus indicates a watershed vascular territory between the area supplied by the medial circumflex femoral artery and the posterior branch of the obturator artery. Ill-defined marrow edema can also be seen in the iliac and ischial bones. In ICH, contrast MRI usually shows enhancement of the lesion as well as synovium. Johnson et al. found additional imaging findings, including central femoral head epiphysis cartilage loss, bone remodeling, and marrow edema involving the head and neck of the femur and acetabulum.[1] Progression of disease manifests as joint space reduction, acetabular changes, changes of osteoarthritis with secondary protrusio acetabuli, and fibrous or bony ankylosis.
Differential diagnosis in a child with hip pain includes slipped capital femoral epiphysis, Perthes disease, septic arthritis, pauciarticular juvenile rheumatoid arthritis (JRA), toxic synovitis, and post-traumatic arthritis. With careful assessment of the clinical features, imaging findings, and diagnostic laboratory results, most of these aforementioned differentials can be excluded.[7]
Reduced hip joint space is a very crucial finding which essentially excludes acute synovitis, septic arthritis, trauma, and initial stages of JRA, as the hip joint space is widened or normal in these cases. Monoarticular JRA predominantly affects the wrist, knee, or ankle joint with very rare involvement of the hip joint. Slipped capital femoral epiphysis is reliably diagnosed on plain X-rays. In ICH, patients classically show a restricted range of motion in all directions, which is more severe than seen in synovitis. Toxic synovitis shows joint effusion and enhancing synovial thickening with an absence of marrow signal changes.[8] MRI features differentiating septic arthritis from transient synovitis are signal changes and contrast enhancement in the bone marrow and periarticular soft tissues in septic arthritis, unlike only enhancing synovial thickening in transient synovitis. Perthes disease shows diffuse homogeneous or heterogeneous marrow abnormalities in the femoral epiphysis, unlike focal marrow changes seen in early ICH.[9]
Herman et al.[10] described the radiological stages of ICH.
Stage 0 – Normal imaging.
Stage 1 – Variable reduction in the hip joint space. On coronal images, a focal wedge-shaped area of STIR/T2 hyperintense marrow edema located in the middle one-third of the femoral head (earliest and characteristic finding in MRI) + mild synovial thickening and joint effusion.
Stage 2 – In addition to stage 1, marrow edema involves superomedial aspect of the acetabulum with protrusio acetabuli (in a few cases).
Stage 3 – Increased extent of marrow edema in the proximal femoral epiphysis, femoral head collapse, wide involvement of acetabulum, and osteoporotic and degenerative changes (fibrous ankylosis) ± overgrowing femoral head on the neck (“buttress” sign).
ICH is reversible with non-surgical management concentrating on rest, alleviation of pain, and avoidance of weight-bearing. Undiagnosed or neglected cases can progress to severe joint space narrowing, protrusio acetabuli, secondary osteoarthritis, and spontaneous ankylosis, which warrants surgical management.[10] To summarize, non-surgical conservative management opts for stage 1 and stage 2 ICH (without protrusio acetabuli). Stage 2 (with protrusio acetabuli) and stage 3 ICH are managed surgically.
CONCLUSION
ICH is a rare debilitating disease that results in articular cartilage loss in proximal femoral epiphysis and acetabulum; in the absence of a known identifiable cause.
MRI is the gold standard radiological modality for the early diagnosis and grading of disease.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Childhood idiopathic chondrolysis of the hip: MRI features. Pediatr Radiol. 2003;33:194-9.
- [CrossRef] [PubMed] [Google Scholar]
- On necrosis of the joint cartilage by epiphyseolysis capitis femoris. Acta Chir Scand. 1930;67:936-46.
- [Google Scholar]
- Idiopathic chondrolysis of the hip: Long-term evolution. J Pediatr Orthop. 1999;19:449-54.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic chondrolysis of the hip: Report of two cases. J Bone Joint Surg Am. 1975;57:268-71.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic chondrolysis of the hip. J Bone Joint Surg Am. 1983;65:1266-75.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic chondrolysis of the hip in children: Early MRI findings. AJR Am J Roentgenol. 2009;192:526-31.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of transient synovitis: Differentiation from septic arthritis. Pediatr Radiol. 2006;36:1154-8.
- [CrossRef] [PubMed] [Google Scholar]
- Legg-Calvé-Perthes disease: Detection of cartilaginous and synovial change with MR imaging. Radiology. 1988;167:473-6.
- [CrossRef] [PubMed] [Google Scholar]






