Translate this page into:
Cloaked bones in Mucolipidosis II - A periosteal reaction in newborns

*Corresponding author: Sana Ashraf Khan, Department of Radiology, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, Maharashtra, India. sana18597@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khan SA, Kale S, Thakkar HU, Alam Z. Cloaked bones in Mucolipidosis II - A periosteal reaction in newborns. Indian J Musculoskelet Radiol. 2024;6:24-7. doi: 10.25259/IJMSR_46_2023
Abstract
On routine, antenatal ultrasound evaluation of a women at 35 weeks gestation showed a fetus (Case 1) with shortening of all the long bones (<5th percentile) with bowing and fuzzy margins. The baby was delivered full term. On physical examination, the baby had a fragile skull, narrow thorax, and short angulated limbs. Postnatal infantogram showed short long bones, periosteal cloaking, fractures, and bell shaped thorax. Another fetus (Case 2) with antenatal ultrasound done elsewhere was suggestive of short and bowed femur. At birth, the baby had angulated limbs. The infantogram shows the periosteal cloaking (thick periosteal reaction) and short long bones similar to the above-mentioned case. Both babies were positive for the I-cell screening test for Mucolipidosis II. Case 1 was confirmed for the same with whole exome sequencing.
Keywords
Periosteal cloaking
Bowing
Angulated limbs
Bell-shaped thorax
INTRODUCTION
Mucolipidosis II (also known as I-cell disease) is a genetically inherited autosomal recessive lysosomal storage disorder occurring due to a deficiency of lysosomal enzyme N-acetylglucoaminyl-phospho-transferase.[1] The empty lysosomes accumulate in the fibroblasts of the bones; hence, skeletal changes are seen. The classic radiographic feature of “periosteal cloaking” is seen in Mucolipidosis-II.
CASE SERIES
Case 1
On routine, antenatal ultrasound evaluation of a women at 35 weeks gestation showed a fetus with shortening of all the long bones (<5th percentile) with bowing and fuzzy margins.
Femur length: Abdominal circumference – 0.13 (i.e., <0.16) [Figure 1a]
Thoracic circumference: Abdominal circumference – 0.75 (should be <0.6 for lethality)
Thoracic circumference – <5th percentile [Figure 1b].
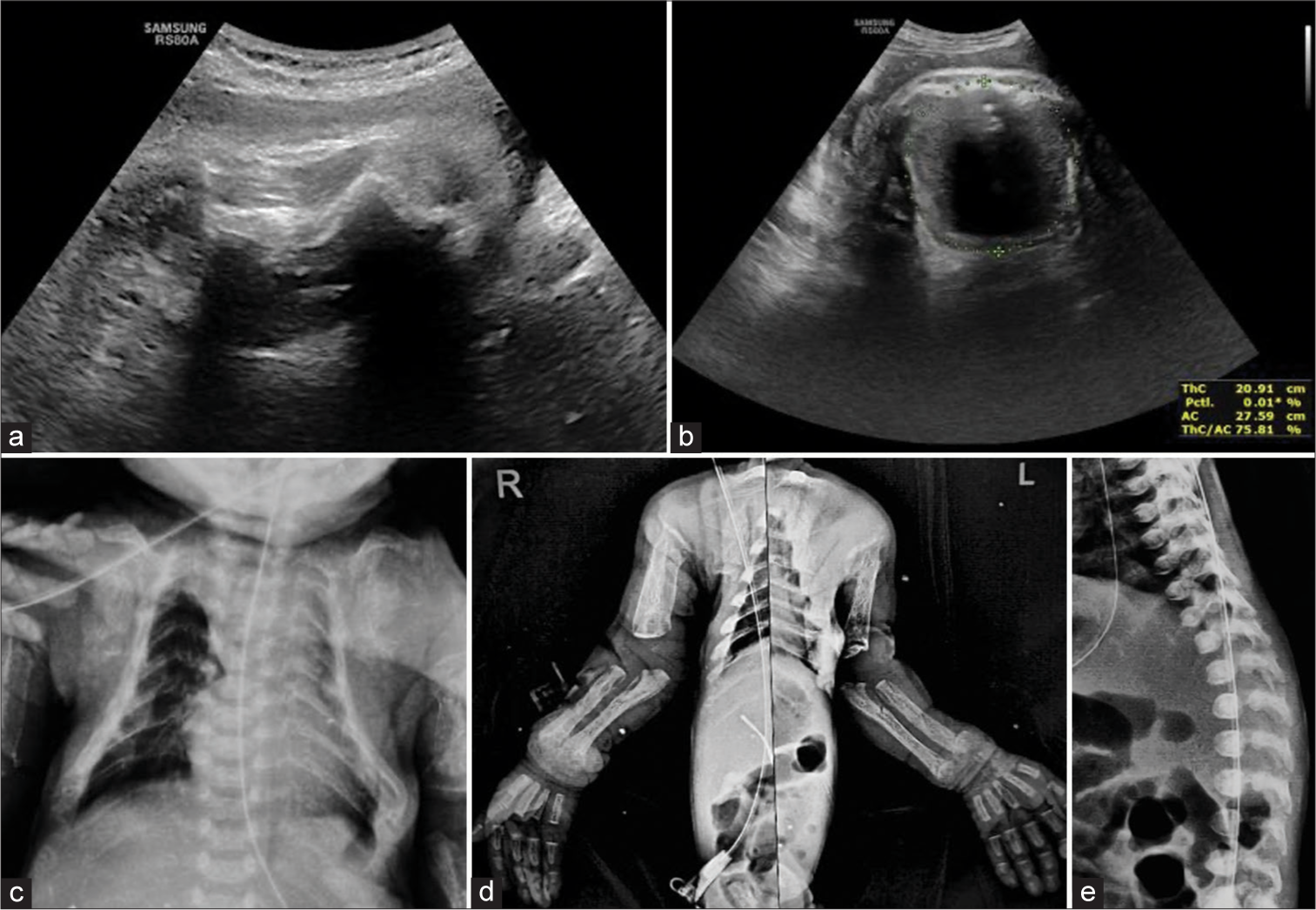
- Images of Case 1. (a) Antenatal ultrasonogram of fetal femur shows a short, angulated femur with fuzzy margins. However, there is a good posterior acoustic shadowing suggesting normal bone density (in contrast to decreased bone density in Osteogenesis imperfecta). Femur length was <5th percentile for the gestational age. (b) Antenatal ultrasonogram at the level of thorax shows the thoracic circumference <5th percentile. (c) Postnatal radiograph of chest shows narrow (Bell-shaped) thorax with thin osteopenic ribs and hypoplastic scapulae. (d) Anteroposterior radiograph of both upper limbs shows short humeri, periosteal cloaking – severe periosteal reaction along all the long bones, fractures in the left ulna and left humerus, distal metaphyseal cupping, and splaying in both the radius and ulna. (e) Lateral radiograph of spine shows convex anterior margin of vertebrae (ovoid vertebrae).
The above two values (1 and 3) indicate lethality.
The baby was delivered full term. On physical examination, the baby had a fragile skull, narrow thorax, and short angulated limbs.
Postnatal radiographs show
Narrow (Bell-shaped) thorax, thin osteopenic ribs, and hypoplastic scapulae [Figure 1c]
Short humeri, periosteal cloaking – severe periosteal reaction along all the long bones, fractures in the left ulna and left humerus, and distal metaphyseal cupping and playing in both the radius and ulna [Figure 1d]
Convex anterior margin of vertebrae (Ovoid vertebrae) [Figure 1e].
The baby was positive for I-cell screening test which showed decreased activity of the lysosomal enzyme. The absence of this enzyme was, further, confirmed with whole exome sequencing. Due to narrow chest circumference, the baby developed respiratory infection and succumbed after 2 weeks due to its complications. History of death in elder sibling was due to respiratory distress at 7th day of life, which is suggestive of genetic etiology [Figure 2].
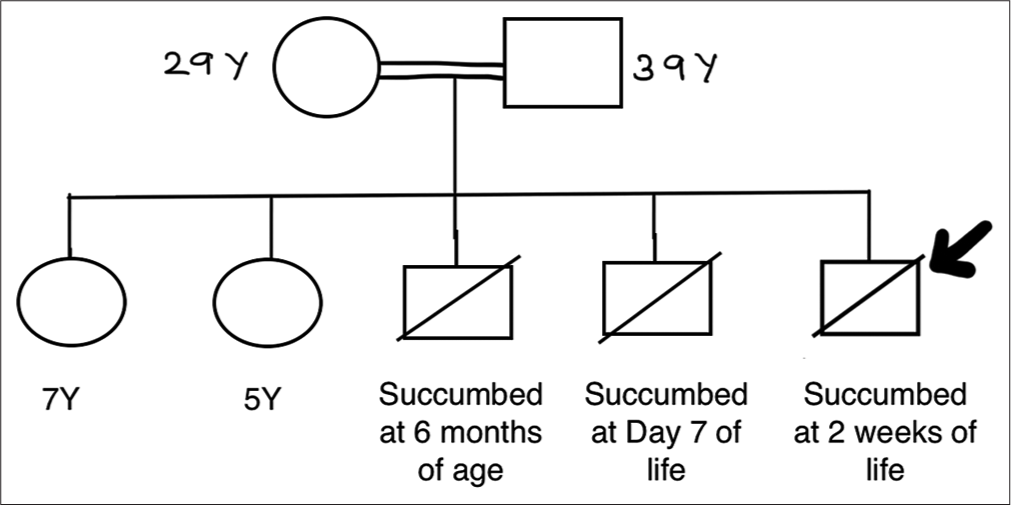
- Pedigree chart for Case 1, Bold arrow indicates the child in Case 1.
Case 2
Another infant presented with short angulated limbs with antenatal ultrasound done elsewhere which was suggestive of short and bowed femur. The infantogram [Figure 3] shows the periosteal cloaking (thick periosteal reaction) and short long bones similar to above-mentioned case. This baby as well was positive for I-cell screening test for Mucolipidosis II. Later, the baby developed respiratory infection and was under intensive care unit. Clinical images of both the cases have been shown in Figure 4.

- Image of Case 2. Postnatal infantogram shows periosteal cloaking (thick periosteal reaction) and short long bones in all limbs.

- Clinical image of Case 1 and Case 2. (a) Case 1: Angulated left forearm and hyper-flexed left leg. (b) Case 2: Angulated left leg.
DISCUSSION
Mucolipidosis II (also known as I-cell disease) is a genetically inherited autosomal recessive lysosomal storage disorder occurring due to a deficiency of lysosomal enzyme N-acetylglucoaminyl-phospho-transferase.[1] The empty lysosomes accumulate in the fibroblasts of the bones; hence, skeletal changes are seen.
These patients can present at birth or within 6–10 months after birth. Clinical features include coarse facies, thick skin, joint contractures, or limb deformity. The most common cause of death is usually due to cardiorespiratory compromise.[2]
Antenatal detection of this condition plays an important role in prognosis of the child. The assessment done with fetal ultrasound includes length of limbs (reduced femur length), abnormal shape (bowing, fractures, etc.), and reduced echogenicity.[3] Chest circumference might be reduced. The section of head circumference shows reduced ossification of skull bones with hyper-visualization of intracranial structures. Definite diagnosis, however, depends on genetic workup in fetuses of skeletal dysplasia; however, one of the most important roles played by ultrasound is the determination of neonatal or infantile lethality.[4] The cause of lethality in most skeletal dysplasias is small chest circumference and resultant pulmonary hypoplasia. However, not all skeletal dysplasias associated with small thoracic circumferences are associated with immediate lethality. When associated abnormalities in other organ systems are detected, it increases morbidity and mortality.
The ultrasound criteria for lethality is:
Chest-to-abdominal circumference ratio of <0.6
Femur length-to-abdominal circumference ratios of <0.16.[5]
The early radiographic features seen in Mucolipidosis II[6] are increased vertebral body height (80%, nonspecific), talocalcaneal stippling (86%), periosteal cloaking (74%), and vertebral body rounding (50%). Other findings included sacrococcygeal sclerosis (54%) and vertebral body sclerosis (13%). Rickets and hyperparathyroidism-like (pseudohyperparathyroidism) changes were also found in 33% of cases. These changes started in the newborn period. There is conversion from these early infantile radiographic features to dysostosis multiplex changes in 41% of cases.
The differential diagnosis for cases with shortened fetal long bones on antenatal ultrasound is a large number of skeletal dysplasias; hence, definitive diagnosis on antenatal ultrasound could not be given; however, the lethality of the dysplasia can be predicted.
However, the differentials for babies born with osteopenic fractures and shortened limbs include-
Congenital rickets/neonatal hyperparathyroidism
Hypophosphatasia
Osteogenesis imperfect
Metabolic disease of preterm
Mucolipidosis II/I cell disease.
The biochemical parameters for both the cases were within normal limits ([Table 1] for Case 1). Hence, the possibility of congenital rickets and neonatal hyperparathyroidism was ruled out. Both the babies were born at term; hence, the possibility of metabolic disease of newborn was ruled out. Based on the [Table 2], radiographic diagnosis of Mucolipidosis II was made which was later confirmed with genetic workup. Prognosis of most affected children is that they do not survive past early childhood.[7] There are currently no approved therapies to reverse the effects of Mucolipidosis II. Current approach is managing specific symptoms through targeted therapies.[8]
| Baby | Mother | |||
|---|---|---|---|---|
| Calcium | 8.4 | within normal limits | 9.1 | within normal limits |
| Phosphorus | 6 | within normal limits | 6.5 | within normal limits |
| Alkaline phosphatase | 1100 | Raised | 120 | within normal limits |
| Osteogenesis imperfecta | Hypophosphatasia | Mucolipidosis II | |
|---|---|---|---|
| Long bones | Osteopenia | Osteopenia | Osteopenia |
| Fractures | Fractures | Fractures | |
| Callus formation | - | - | |
| Metaphyseal widening | Metaphyseal lucencies or tongues | Metaphyseal fragmentation | |
| - | Diaphyseal spurs and hypoplastic fibulae | Periosteal cloaking and cortical erosions | |
| Chest | Short thin ribs | Beaded ribs | Almost invisible or hypoplastic scapulae |
| Skull | Wormian bones | Deficient ossification with wide sutures | Metopic and coronal synostosis |
| Spine | - | Absent pedicle | Ovoid vertebral bodies |
| Intervertebral disc calcifications | |||
| Pelvis | - | - | Flared iliac wings with horizontal acetabular roofs |
CONCLUSION
Lethal skeletal dysplasias usually present in the first/early second trimester. We tend to report non-lethal skeletal dysplasia in 3rd trimester; however, these cases teach us not to overlook the possibility of lethality even in 3rd trimester.
Mucolipidosis-II should be included as a rare differential for osteopenia with bone-within-bone appearance in newborns after ruling out other relatively common ones such as osteogenesis imperfecta, congenital rickets, and hypophosphatasia.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Mucolipidosis II (I-cell disease) and mucolipidosis IIIA (classical pseudo-hurler polydystrophy) are caused by mutations in the GlcNAcphosphotransferase α/β-subunits precursor gene. Am J Hum Genet. 2006;78:451.
- [CrossRef] [PubMed] [Google Scholar]
- Mucolipidosis 2 In: Atlas of genetic diagnosis and counseling. Germany: Springer; 2016. p. :1-10.
- [CrossRef] [Google Scholar]
- The fetal medicine foundation. Available from: https://fetalmedicine.org/education/fetal-abnormalities/skeleton/skeletal-dysplasia# [Last accessed on 2023 Aug 25]
- [Google Scholar]
- Ultrasonographic prediction of lethal pulmonary hypoplasia: Comparison of eight different ultrasonographic parameters. Am J Obstet Gynecol. 1996;175:477-83.
- [CrossRef] [PubMed] [Google Scholar]
- Suspected skeletal dysplasias: femur length to abdominal circumference ratio can be used in ultrasonographic prediction of fetal outcome. Am J Obstet Gynecol. 1997;177:864-9.
- [CrossRef] [PubMed] [Google Scholar]
- Early characteristic radiographic changes in mucolipidosis II. Pediatr Radiol. 2016;46:1713-20.
- [CrossRef] [PubMed] [Google Scholar]
- Phenotype and genotype in mucolipidoses II and III alpha/beta: A study of 61 probands. J Med Genet. 2010;47:38-48.
- [CrossRef] [PubMed] [Google Scholar]
- Mucolipidosis II (ML II) - Boston children’s hospital. Available from: https://www.childrenshospital.org/conditions/mucolipidosis-ii# [Last accessed on 2023 Aug 25]
- [Google Scholar]






