Translate this page into:
A resident’s sharp learning curve: Post-needle stick injury arteriovenous fistula of the finger

*Corresponding author: Ajith Ramakumar Varrior, Department of Radiodiagnosis, Seth GS Medical College and KEMH, Mumbai, Maharashtra, India. ajithvarrior@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varrior AR, Driver ZV, Waghela M, Gala F. A resident’s sharp learning curve: Post-needle stick injury arteriovenous fistula of the finger. Indian J Musculoskelet Radiol. 2024;6:136-9. doi: 10.25259/IJMSR_32_2024
Abstract
Iatrogenic vascular injuries can be encountered during diagnostic or therapeutic interventions. Traumatic arteriovenous fistulas (AVFs) occur due to penetrating injury involving contiguous arteries and veins. We report a case of a 27-year-old postgraduate trainee who presented with swelling over her left middle finger for 5 months following a needle prick injury at the same site 1 year back, which was diagnosed with ultrasound and dynamic magnetic resonance imaging angiography. Endovascular embolization is avoided in AVFs of the hand due to the risk of distal ischemia, and surgical excision with reconstruction is the preferred treatment.
Keywords
Needle prick
Arteriovenous fistula
Traumatic arteriovenous fistula of finger
Arteriovenous fistula of the digital arteries
Magnetic resonance angiography
INTRODUCTION
Vascular anomalies have undergone multiple changes in classification, the recent one being updated in the year 2018 by the International Society for the study of vascular anomalies on the basis of cellularity, flow pattern, and clinical features.[1,2] However, this classification has not taken into consideration post-traumatic causes, which are rather more common than congenital types.[1]
Various vascular anomalies in the hand include arteriovenous fistula (AVF), arteriovenous malformation, and venous aneurysm.[1] AVF refers to the direct communication between an artery and a vein bypassing the capillary network. An example of a therapeutic AVF is that of hemodialysis access. We report a case of a 27-year-old woman who presented with an AVF of the finger following a needle stick injury, which, to the best of our knowledge, has not been reported previously.
CASE REPORT
A 27-year-old postgraduate trainee in the obstetrics and gynecology department presented with a history of swelling over the radial aspect of her left middle finger in the region of the middle phalanx for the past 5 months. One year back, she had a history of needle prick injury at the same site while performing a procedure. The swelling was reddish and not associated with pain. The overlying skin was smooth. The lesion was soft and non-tender, with a subtle thrill on palpation. It measured approximately 1 cm × 0.8 cm [Figure 1].

- A 27 year old woman presented with a swelling over her left middle finger. The swelling is reddish with a smooth overlying skin.
Ultrasound of the lesion showed a well-defined heterogeneously hypoechoic lesion in the subcutaneous plane with vascularity on color Doppler [Figure 2]. On spectral Doppler, the lesion had both arterial and venous waveforms with a maximum velocity of 30 cm/s [Figure 3]. The tendons were seen separate from the lesion. The underlying bone was normal.
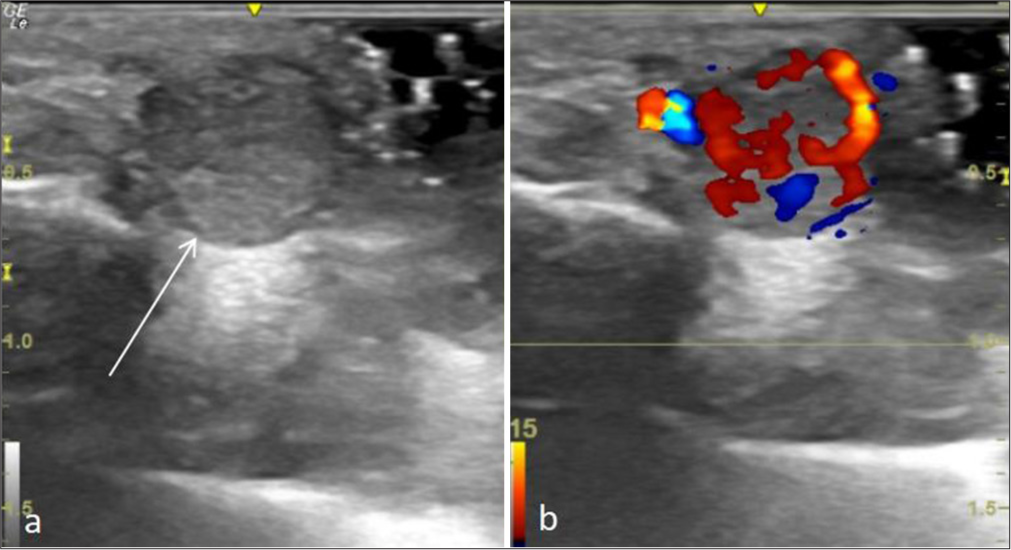
- A 27 year-old woman with an arteriovenous fistula of the digit presented with swelling over her left middle finger. (a) Ultrasound of the lesion with the probe perpendicular to the long axis of the finger shows a well defined heterogenously hypoechoic lesion in the subcutaneous plane (arrow). (b) Colour Doppler shows vascularity within the lesion.
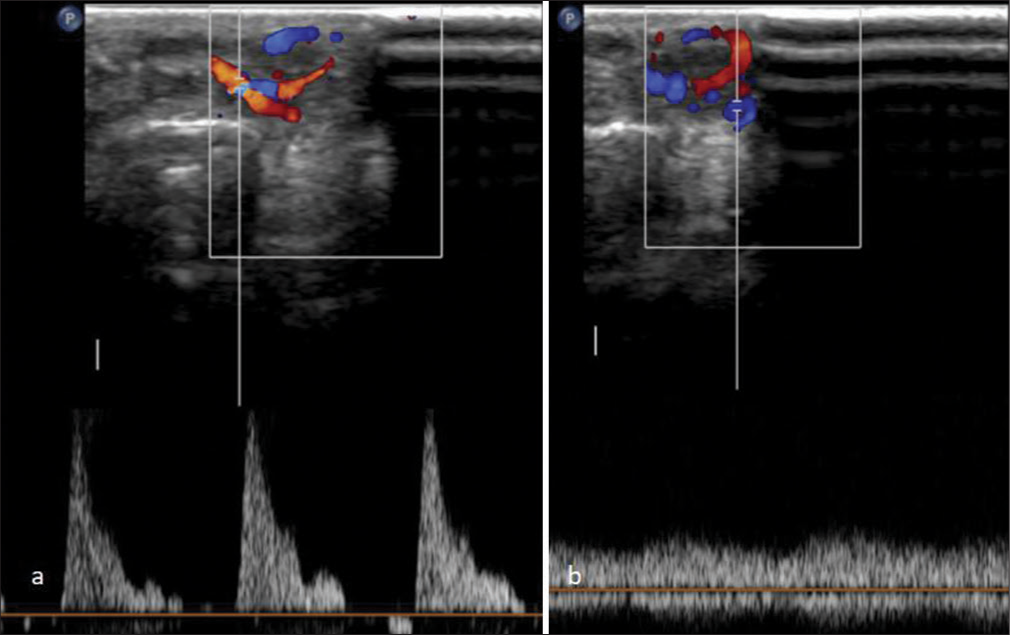
- A 27 year old woman with an arteriovenous fistula of the digit presented with swelling over her left middle finger. (a) Arterial waveform on Doppler spectrum, (b) venous waveform on Doppler spectrum.
A magnetic resonance imaging (MRI) of the finger showed a well-defined 7 × 10 × 20 mm round lobulated lesion in the subcutaneous plane along the radial aspect of the middle finger at the region of the middle phalanx. There was a serpiginous extension proximally up to the proximal interphalangeal joint. It was hyperintense on short-tau inversion recovery, hypointense on T1 sequences. Fat planes were maintained with the flexor tendon and the collateral ligaments [Figure 4]. On dynamic imaging, there was early arterial phase enhancement with supply from the branch of the proper digital artery along the radial aspect of the middle finger with an early draining vein [Figure 5]. The lesion was excised surgically.
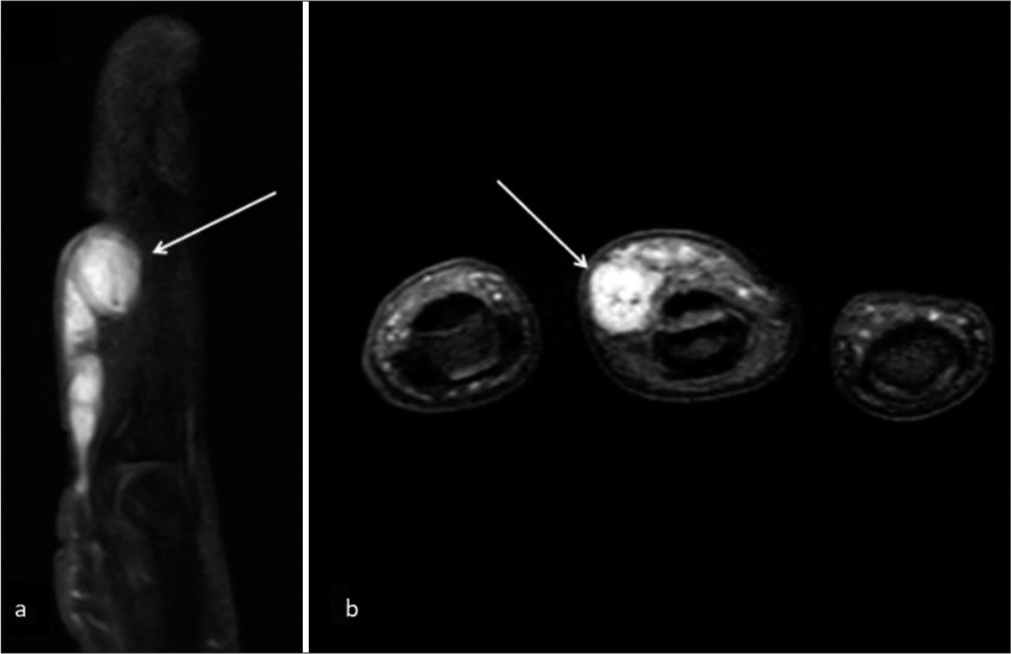
- A 27 year old woman with an arteriovenous fistula of the digit presented with swelling over her left middle finger. MRI of the finger in the short tau inversion recovery sequence shows: (a) A well defined hyperintense lobulated round lesion (arrow) with a serpiginous proximal extension, (b) the lesion (arrow) is separate from the flexor tendon, located eccentrically towards the radial aspect of the finger.
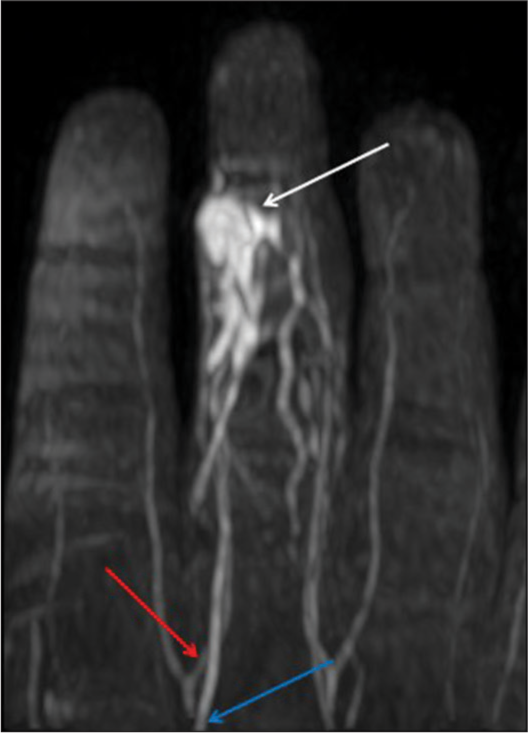
- A 27-year-old woman with an arteriovenous fistula of the digit presented with swelling over her left middle finger. Dynamic magnetic resonance angiography MIP image shows the lesion (white arrow) with an arterial feeder (red arrow) from the radial branch of the proper digital artery of the middle finger. There is an early draining vein (blue arrow). MIP: Maximum intensity projection.
DISCUSSION
Vascular injuries can be either due to penetrating or blunt injuries. The various forms of penetrating vascular injury include puncture, laceration, transection, dissection, aneurysm, or AVF formation. Non-penetrating injuries include intimal contusion, intimal flap, and intimal injury with thrombosis.[3] Iatrogenic vascular injuries can be encountered during diagnostic or therapeutic interventions, such as drawing intravenous/arterial blood, securing intravascular access, or occurring as an adverse event during procedures where there are chances of damage to the adjacent vessels. These injuries are also common in IV drug abusers. In the western countries, gunshot injuries are the common cause of penetrating vascular injuries. Needle injuries are mostly accidental and are seen commonly in healthcare workers.
Traumatic AVFs occur due to penetrating injury involving contiguous arteries and veins.[3,4] It is a chronic event where there is transmission of high pressure from the arteries into the low-pressure venous system. The presentation depends on the size of the fistula. Most commonly there is a pulsatile swelling with redness and warmth of the overlying skin. A thrill may be palpable due to the turbulent flow within the fistula. Distally, the region might be cold or ischemic due to the steal phenomenon. There might be varicosities along the venous drainage pathway with signs of chronic venous insufficiency. When the shunting is severe enough, there are signs of heart failure due to increased preload.
AVFs in the digits due to needle pricks are extremely rare and have not been described previously to the best of our knowledge. AVFs of the digits have been reported following blunt trauma (caught in the door, crush injury, and during sports).[5,6] Iatrogenic AVF following failed peripheral IV cannulation has been reported in the hand. Complications such as rupture and hemorrhage are not common in AVFs of the digital arteries. High-flow AVF can cause remodeling of the underlying bones in the form of pressure erosions and reduced density.[7] Ultrasound is the first-line modality of investigation in such cases. The supplying artery shows a high-velocity, low-resistance waveform, while the draining vein shows a pulsatile waveform.[8]
Computed tomography angiography is non-invasive, has multiplanar reconstruction, and also provides the adjacent anatomical details. MRI has better soft tissue and contrast resolution and lacks radiation. However, angiography is considered the gold standard investigation for AVFs. Both dynamic contrast MRI and conventional angiography demonstrate a communication between the artery and the early draining vein.
The management of the AVFs can be either surgical or endovascular. Surgical ligation of the feeding artery is performed with or without reconstruction, depending on the site involved. This has to be performed carefully to prevent distal ischemia. Embolization is avoided, whereas reconstruction has been advised when the hand is involved to restore physiologic conditions and to ensure adequate distal perfusion.[5] Very rarely, the AVF can undergo spontaneous closure on its own.[9] The incidence is higher in cases of AVF with pseudoaneurysm due to the diversion of blood to the aneurysm. This results in less flow to the fistula, which promotes coagulation and closure.
CONCLUSION
Although rare, an AVF should be considered under the differential diagnosis of a vascular lesion in the digits, especially in an appropriate clinical context. Although an ultrasound is the first line of investigation, an MR angiogram clinches the diagnosis, and the radiologist should make the call to perform an angiogram if findings are suspicious on a non-contrast MRI.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Posttraumatic vascular anomalies in hand surgery-a case-based approach. Plast Reconstr Surg Global Open. 2021;9:e3802.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral vascular malformations: Imaging, treatment approaches, and therapeutic issues. Radiographics. 2005;25(Suppl 1):S159-71.
- [CrossRef] [PubMed] [Google Scholar]
- Chapter 63: Vascular trauma In: Vascular medicine: A companion to Braunwald's heart disease. Sec 18: Miscellaneous. Netherland: Elsevier; 2006. p. :894-919.
- [CrossRef] [Google Scholar]
- Diagnosis of clinically unsuspected posttraumatic arteriovenous fistulas of the pelvis using CT angiography. Am J Roentgenol. 2007;188:W269-73.
- [CrossRef] [PubMed] [Google Scholar]
- Arteriovenous fistula secondary to recurrent metacarpophalangeal joint dislocation: A case report. Ochsner J. 2009;9:14-6.
- [Google Scholar]
- Acquired arteriovenous fistula of a finger. VASA. 2019;48:368-70.
- [CrossRef] [PubMed] [Google Scholar]
- Iatrogenic arteriovenous fistula in the hand: A case report. J Plast Reconstr Aesthet Surg. 2012;65:e351-3.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous closure of traumatic arteriovenous fistula. Radiology. 1976;118:291-2.
- [CrossRef] [PubMed] [Google Scholar]







