Translate this page into:
Calcific tendinitis of the flexor digitorum profundus in a pediatric patient: A common condition in an uncommon location

*Corresponding author: Harmeet Kaur, Department of Radiodiagnosis, All India Institute of Medical Sciences, Bathinda, Punjab, India. kaurh28@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur H, Bajaj M, Garg A, Tiwari P. Calcific tendinitis of the flexor digitorum profundus in a pediatric patient: A common condition in an uncommon location. Indian J Musculoskelet Radiol. doi: 10.25259/IJMSR_75_2024
Abstract
In this report, we present the case of a 12-year-old boy with calcific tendinitis of the flexor digitorum profundus (FDP) tendon, presenting with pain and restricted movement in the left index finger. The patient had no history of trauma or illness, and laboratory tests showed mildly elevated inflammatory markers. Multimodality imaging, including X-ray, sonography, and magnetic resonance imaging, confirmed calcific deposits within the FDP tendon, with no signs of infection or bone involvement. Conservative treatment with non-steroidal anti-inflammatory drugs and splinting resulted in significant improvement, with complete symptom resolution and near-total disappearance of the calcification on follow-up radiographs. This case highlights the importance of imaging in diagnosing calcific tendinitis in pediatric patients, a rare condition in this age group. Imaging plays a pivotal role in confirming the diagnosis and ruling out differential diagnoses, such as infection or trauma. Early recognition and non-invasive management ensure excellent outcomes, avoiding unnecessary interventions.
Keywords
Calcific tendinitis
Flexor digitorum profundus tendon
Intratendinous calcific deposit
Pediatric
INTRODUCTION
Calcific tendinitis, while well-documented in adults, is an uncommon entity in pediatric patients, particularly in the tendons of the hand. It is most commonly observed in the rotator cuff tendons of the shoulder.[1] However, it can occur in other body parts, with the hip and knee joints being the second and third most frequent sites.[2]
The condition arises due to the deposition of calcium hydroxyapatite crystals within or around the tendons, leading to an acute inflammatory reaction.[1] The incidence in hand and wrist is estimated to be around only 2%,[3] but the incidence in children is even rarer, making it an underdiagnosed condition in this age group. The rarity of calcific tendinitis in pediatric patients may be attributed to increased tendon vascularity, reduced cumulative mechanical stress, efficient metabolic regulation, and the absence of pre-existing tendon degeneration.[4,5] In hand involvement, calcific tendinitis of the flexor tendons, especially the flexor digitorum profundus (FDP), is exceedingly rare. The clinical presentation often overlaps with conditions such as infectious tenosynovitis, traumatic tendon injury, gout, or inflammatory arthritis, which may lead to misdiagnosis.[6] This case report highlights a rare instance of calcific tendinitis of FDP in a pediatric patient, emphasizing the role of imaging in differentiating it from other conditions and guiding appropriate treatment.
CASE REPORT
A 12-year-old boy presented with pain and difficulty in flexing the proximal interphalangeal (PIP) joint of his left index finger. The symptoms had an insidious onset and progressively worsened over the past 4 days. There was no history of trauma, repetitive strain, or recent illness. His past medical history was unremarkable.
On examination, the child was afebrile and showed no signs of systemic illness. The left index finger appeared swollen, erythematous, and tender to palpation along the volar aspect, particularly around the PIP joint. The range of motion was notably restricted, and both passive and active finger extension elicited pain.
Laboratory investigations, including a white blood cell count of 7200/μL and an erythrocyte sedimentation rate of 8 mm/h, were within normal limits, effectively ruling out systemic infection or inflammation. The C-reactive protein level, measured at 6.0 mg/dL, was slightly elevated, suggesting mild inflammation. His serum calcium, phosphorous, alkaline phosphatase, and uric acid levels are within normal limits.
X-ray imaging of the left hand, performed in the posteroanterior oblique and lateral views, revealed a cluster of few small, well-defined, lobulated radiopaque calcific foci on the flexor aspect of the index finger at the level of the PIP joint. The phalanges of the index finger and the hand appeared grossly normal [Figure 1a and b]. High-resolution sonography was done on a BPL Alpinion scanner (Model: X -CUBE 70) using a linear probe of frequency 10–25 Megahertz, which showed hyperechoic foci with faint posterior acoustic shadowing along the course of the FDP tendon near the PIP joint, proximal to its insertion, suggesting intratendinous calcification. Mildly hypoechoic surrounding soft tissue suggested localized inflammation [Figure 2a and b].
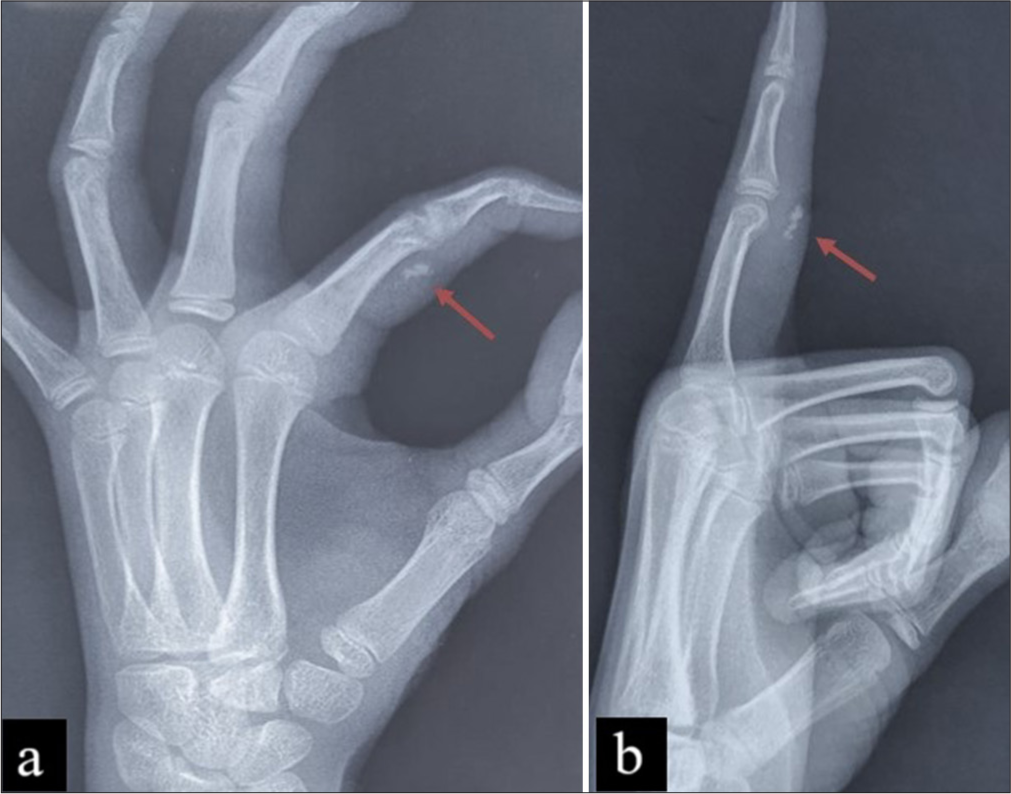
- (a) X-ray PA oblique view left hand and (b) lateral view index finger showing a cluster of few small, well-defined, lobulated radiopaque calcific foci on the flexor aspect of the index finger at the level of the PIP joint highlighted by red arrows, with normal-appearing phalanges and hand structures. PA: Posteroanterior, PIP: Proximal interphalangeal.
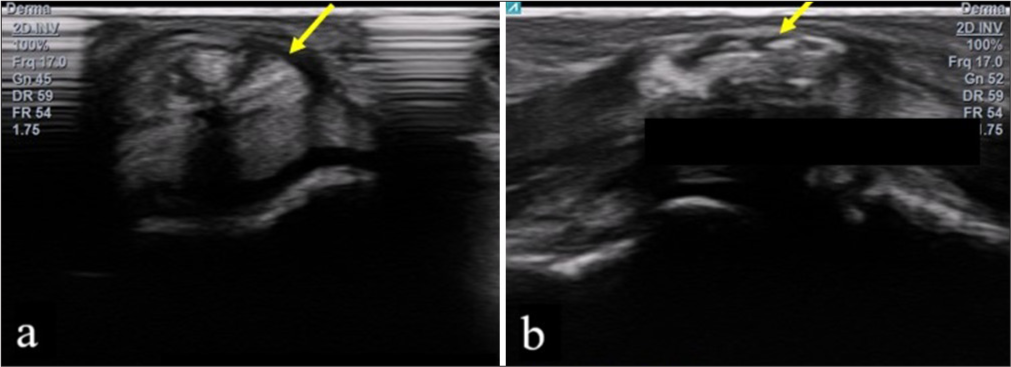
- (a) Ultrasound transverse view index finger of the left hand and (b) sagittal view showing thickening and irregularity of FDP tendon at the level of PIP joint with intratendinous heterogeneity and lobulated echogenic foci giving faint posterior acoustic shadowing suggesting calcific tendinitis (yellow arrows in a and b). FDP: Flexor Digitorum Profundus, PIP: Proximal interphalangeal.
Magnetic resonance imaging (MRI) was performed using a Siemens Healthineers 3T scanner (Model: Magnetom Skyra) and showed a slightly thickened and swollen FDP tendon with increased signal intensity on T2-weighted and short-tau inversion recovery (STIR) images, indicating intratendinous and peritendinous fluid signal or edema or inflammation. Several small hypointense foci representing calcific deposits were observed within the FDP tendon along its course over PIP. In addition, reactive changes were noted as STIR and proton density fat-saturated hyperintensity in the underlying volar plate and joint capsule. There was no evidence of synovial proliferation in this case. In addition, no abnormal marrow signal was seen in the phalanges, carpals, or other hand bones, and no signs of bone erosion or destruction [Figure 3a-c].
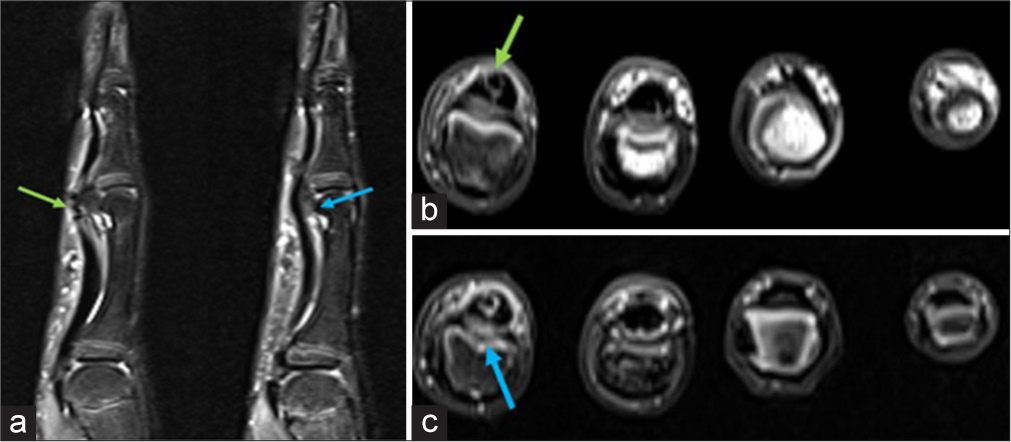
- (a) STIR sagittal view of the index finger in the midline and along the radial aspect, (b) Axial T1, and (c) Axial PDFS magnetic resonance images demonstrating intratendinous hypointense foci (green arrows in a and b) within the FDP tendon, indicative of calcific deposits. In addition, hyperintensity on STIR and PDFS sequences is observed in the underlying volar plate, joint capsule, and overlying subcutaneous fat, consistent with reactive changes (blue arrows in a and c). No evidence of marrow edema in the phalanges of the finger. STIR: Short-tau inversion recovery, PDFS: Proton density fat-saturated, FDP: Flexor digitorum profundus.
Based on the clinical presentation, laboratory investigations, and imaging findings, the patient was diagnosed with FDP calcific tendinitis.
The patient was managed conservatively with splinting exercises, along with a course of anti-inflammatory drugs/non-steroidal anti-inflammatory drugs. A volar splint was advised for the first 2 weeks, with gradual discontinuation planned over the following 6 weeks.
Upon review after 2 weeks, significant improvement was noted, with a marked reduction in swelling and pain. Tenderness persisted only over the flexor aspect of the PIP joint. The child was then instructed to perform passive and active range-of-motion exercises to prevent stiffness in the affected finger. At the second follow-up, 2 months later, the patient was completely pain-free, with no swelling in the finger and a full range of motion in the interphalangeal joints with complete restoration of finger function and no recurrence of pain or swelling. Follow-up radiographs taken 2 months later showed a marked resolution of the calcification [Figure 4].

- Follow-up X-ray done after 2 months showing marked resolution of tendinous calcification.
DISCUSSION
Calcific tendinitis results from the deposition of calcium crystals, typically calcium hydroxyapatite, in the tendon tissues.[1] This process is distinct from degenerative joint disease. While calcification may often be asymptomatic, calcific tendinitis can sometimes be a significant source of pain.[7]
The pathogenesis of calcific tendinitis remains incompletely understood but is believed to involve factors such as repetitive microtrauma, localized hypoxia, and resultant dystrophic calcification. In some cases, metabolic and endocrine disorders, including hyperparathyroidism and hypovitaminosis D, may play a role. However, the condition often occurs spontaneously in children without identifiable risk factors. In addition, inflammatory processes may contribute to tendon degeneration, ultimately leading to calcification.[8]
Histopathologically, this condition is characterized by hydroxyapatite deposition into psammoma-like bodies surrounded by inflammatory cells.[9] In addition, it has been associated with autoimmune diseases such as thyroid disorders, rheumatoid arthritis, and systemic sclerosis as well as metabolic conditions such as diabetes, gout, and pseudogout.[10]
In children presenting with finger pain and swelling, the common differential diagnoses include infectious tenosynovitis, traumatic injury, and juvenile idiopathic arthritis (JIA).[6] Infectious tenosynovitis is typically accompanied by systemic signs such as fever and elevated inflammatory markers, which were not observed in this case. In addition, there was no history of trauma. JIA often presents with chronic joint swelling and systemic features, both of which were absent in this patient. Thus, the absence of systemic symptoms and normal laboratory values, combined with imaging findings, ruled out these differentials, confirming acute calcific tendinitis.
Imaging plays a pivotal role in the diagnosis of calcific tendinitis. While X-rays can reveal calcifications, ultrasonography is highly sensitive in detecting small calcific deposits and associated inflammation. On MRI, calcific deposits are seen as signal voids (hypointense) on all sequences, with blooming artifacts on gradient-echo sequences. MRI offers valuable insights into the extent of tendon involvement, associated soft tissue changes, and surrounding edema, aiding in differentiating calcific tendinitis from other conditions.[11]
Treatment often begins with oral analgesic or anti-inflammatory medications to alleviate pain and reduce inflammation. In some cases, local anesthetic or steroid injections may be administered to provide targeted relief from pain and inflammation. For more extensive calcific deposits that do not respond to conservative treatments, surgical intervention such as barbotage may be considered, a minimally invasive procedure to aspirate the deposits. In addition, in refractory cases, extracorporeal shock wave therapy may be used to break down the calcific deposits and promote healing. Pediatric patients respond well to rest, analgesics, and immobilization.[12]
CONCLUSION
This case highlights the need to consider acute calcific tendinitis as a differential diagnosis in pediatric patients presenting with localized finger pain and swelling, even in the absence of trauma. Given the rarity of acute calcific tendinitis in children, the likelihood of misdiagnosis is considerably higher. We recommend considering calcific tendinitis as a potential diagnosis and adopting a multimodality approach when adults or children present with acute localized inflammation in the FDP. Early recognition and treatment can prevent unnecessary interventions and ensure favorable outcomes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Rotator cuff calcific tendonitis: Short-term and 10-year outcomes after two-needle us-guided percutaneous treatment--nonrandomized controlled trial. Radiology. 2009;252:157-64.
- [CrossRef] [PubMed] [Google Scholar]
- The acute and chronic presentation of gluteus medius calcific tendinitis-a case report of two. J Orthop Case Rep. 2014;4:48-50.
- [Google Scholar]
- Acute calcific tendonitis of dorsal interosseous muscles of the hand: Uncommon site of a frequent disease. Reumatismo. 2017;69:43-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acute calcific tendinitis of the flexor pollicis longus in an 8-year-old boy. Skeletal Radiol. 2014;43:1471-5.
- [CrossRef] [PubMed] [Google Scholar]
- Calcific tendinitis of the supraspinatus tendon in a 7-year-old boy: Diagnostic challenges. Hong Kong Med J. 2011;17:414-6.
- [Google Scholar]
- Enveloping calcification of flexor digitorum profundus tendon: A diagnosis easily missed. BMJ Case Rep. 2020;13:e233510.
- [CrossRef] [PubMed] [Google Scholar]
- Calcium deposits in the shoulder and subacromial bursitis: A survey of 12,122 shoulders. JAMA. 1941;116:2477-81.
- [CrossRef] [Google Scholar]
- Physiopathology of intratendinous calcific deposition. BMC Med. 2012;10:95.
- [CrossRef] [PubMed] [Google Scholar]
- Calcifying tendinitis: A new concept of its pathogenesis. Clin Orthop. 1976;118:164-8.
- [CrossRef] [Google Scholar]
- Acute calcific periarthritis of proximal interphalangeal joints in a professional golfer's hand. J Korean Med Sci. 2004;19:904-6.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of calcification of the lateral collateral ligament of the knee: A rare abnormality and a cause of lateral knee pain. Am J Roentgenol. 2003;181:199-202.
- [CrossRef] [PubMed] [Google Scholar]
- Acute calcific tendinitis of the index finger in a child. Hand (NY). 2017;12:84-7.
- [CrossRef] [PubMed] [Google Scholar]







