Translate this page into:
Ultrasound-guided aspiration and barbotage of acute calcific tendonitis in unusual locations

*Corresponding author: Amith Gaitonde, Department of Radiodiagnosis, Deenanath Mangeshkar Hospital, Pune, Maharashtra, India. amitgaitonde03@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Babhulkar JA, Gaitonde A. Ultrasound-guided aspiration and barbotage of acute calcific tendonitis in unusual locations. Indian J Musculoskelet Radiol. 2024;6:18-23. doi: 10.25259/IJMSR_6_2023
Abstract
Acute calcific tendonitis is an excruciatingly painful condition occurring due to the deposition of calcium, that is, calcium hydroxyapatite crystals within the tendons with subsequent rupture into the peritendinous tissues. The most common sites of calcific tendonitis are rotator cuff tendons, followed by the gluteal tendons in the hip. However, calcific tendonitis can occur in any tendons in the body. In this article, we present three unusual sites of acute calcific tendonitis with peritendinous rupture as diagnosed on high-resolution ultrasound (HRUS), along with its ultrasound-guided management. We should be familiar with these unusual sites and their management so that immediate relief and early recovery can be provided to the patient.
Keywords
Calcific tendonitis
Common extensor origin calcific tendinopathy
Pectoralis major calcific tendinopathy
Ultrasound-guided aspiration and barbotage
INTRODUCTION
Acute calcific tendonitis is an excruciatingly painful condition occurring due to the deposition of calcium hydroxyapatite crystals within the tendons with subsequent rupture into the peritendinous tissues or joint cavity.[1] The most common sites of calcific tendonitis are rotator cuff tendons in the shoulder and the gluteal tendons in the hip. However, calcific tendonitis can occur in any tendons in the body. The less common sites are within the tendons around the elbow joint, wrist joint, ankle joint, etc.
The most commonly affected age group is 30–60 years. The exact etiology is difficult to determine in most cases. It is associated with diabetes, hypothyroidism, deficiency of Vitamin D, etc.[2] The pathogenesis involves metaplasia of tenocytes into fibrocartilage, which then calcifies to form a calcium chunk within the tendon.[3]
Initially, the patients are asymptomatic; later, patients develop low-grade pain, and finally, when the inflammation sets in, there is severe pain.[4] Uhthoff and Loehr described four stages in the pathogenesis of calcific tendonitis as follows:[5]
The first stage is the pre-calcific stage, where there is metaplasia of the tenocyte into fibrocartilage, and the patient is asymptomatic in this stage.
The second is the stage of calcification or formative stage, where there is calcification of the fibrocartilage and the patient has low-grade pain.
The third is the stage of resorption, where there is an inflammatory response targeted against calcium, causing severe pain and sometimes associated with complications like rupture of the calcium chunk into the adjacent planes like bursa and, less commonly, into the joint cavity.
The last one is the post-calcific stage or recovery stage, where the inflammatory response subsides over months and is associated with chronic dull aching pain.
Bianchi and Martinoli classified calcifications into three types depending on the echogenicity, which reflects the calcium density.
Type 1 calcification is a well-defined hyperechoic focus with significant posterior acoustic shadowing. These are seen in the stage of calcification in pathogenesis.
Type 2 calcification is seen as hyperechoic focus with mild acoustic shadowing.
Type 3 calcification appears as an amorphous inhomogeneous iso-hyperechoic mass with no posterior acoustic shadowing. Both Type 2 and Type 3 calcifications are seen in the resorptive stage and post-calcific stages of the pathogenesis.
Ultrasound-guided aspiration and barbotage are a minimally invasive treatment reserved for cases of severe acute calcific tendonitis with rupture of the Type 3 calcium into the peritendinous tissues. We present three cases of severe acute calcific tendonitis with rupture into the peritendinous tissues in very unusual sites. These were diagnosed on HRUS and ultrasound (USG)-guided aspiration and barbotage were performed in all three patients in the same setting.
CASE SERIES
Case 1
A 49-year-old gentleman came with a history of pain in the anterior aspect of the arm for one week, aggravated significantly for 2–3 days. The patient is a regular gym goer, and there was no obvious history of trauma. On examination, he had restricted flexion and extension at the elbow with severe tenderness over the mid-anterior arm. HRUS [Figure 1a and b] revealed a large Type 3 focus of amorphous, ill-defined calcification along the floor of the bicipital groove in the region of the attachment sites of the pectoralis major and latissimus dorsi. There were associated edematous changes within the coracobrachialis muscle as well as the tendon of the pectoralis major. Two small Type 2 calcifications were also noted at the attachment of the pectoralis major tendon. The plain radiograph [Figure 1c and d] showed a well-defined radiopacity in the anterior aspect of the arm just anterior to the upper humeral shaft.
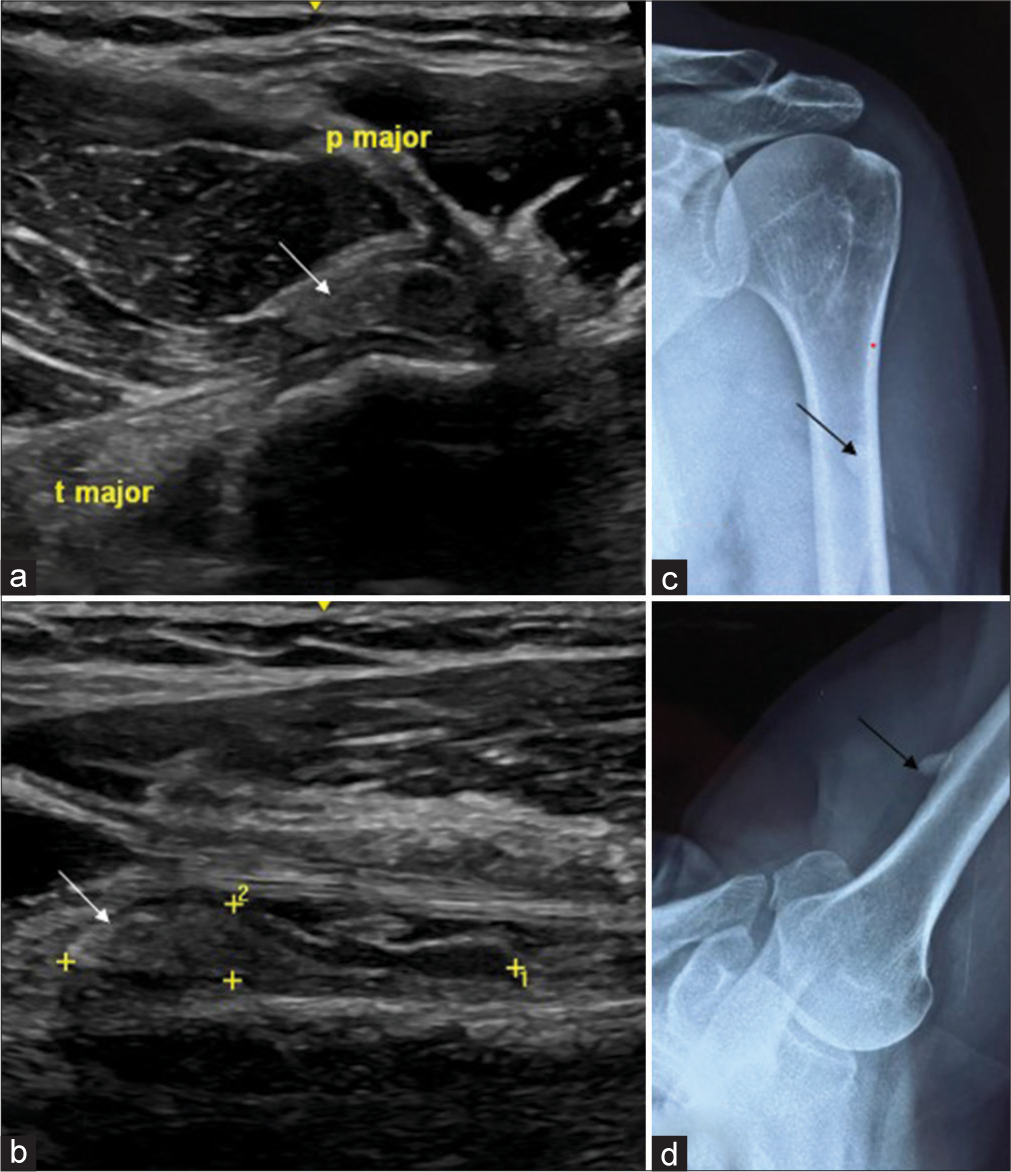
- A 49 years old gentleman came with a history of pain in the anterior aspect of the arm for 1 week. (a) High-resolution ultrasound (HRUS) short-axis, (arrow) (b) long-axis, revealed (arrow) a large (24 x 5 x 10 mm) type 3 focus of amorphous, ill-defined calcification along the floor of the bicipital groove in the region of the attachment sites of the pectoralis major and latissimus dorsi (labelled). There were associated oedematous changes within the coracobrachialis muscle as well as the tendon of pectoralis major. (c) Plain radiograph Anterior Posterior (AP) and (d) lateral showed a well-defined radiopacity in the anterior aspect of the arm just anterior to the upper humeral shaft (arrow), The + symbol is caliper that comes when any measurement is taken in an ultrasound machine. +1 means first measurement. +2 means second measurement.
Case 2
A 35-year gentleman presented with pain and stiffness over the lateral aspect of his right elbow one year after he had a fall from a bike. Currently, the patient complained of aggravation of pain for the past 3 days without any obvious triggering factor [Figure 2 a and b]. HRUS showed a focus of type 2 calcification was seen within the humeral attachment of the radial collateral ligament [Figure 2c]. Another large amorphous type 3 focus of calcification was seen within the posterior part of the common extensor origin with surrounding fluid, fat stranding suggestive of grade III hyperemia [Figure 2d] on power Doppler. The fluid collection with calcifications was seen to communicate with the elbow joint associated with mild joint effusion. A small focus of type 2 calcification was also noted within the distal attachment of the triceps tendon.
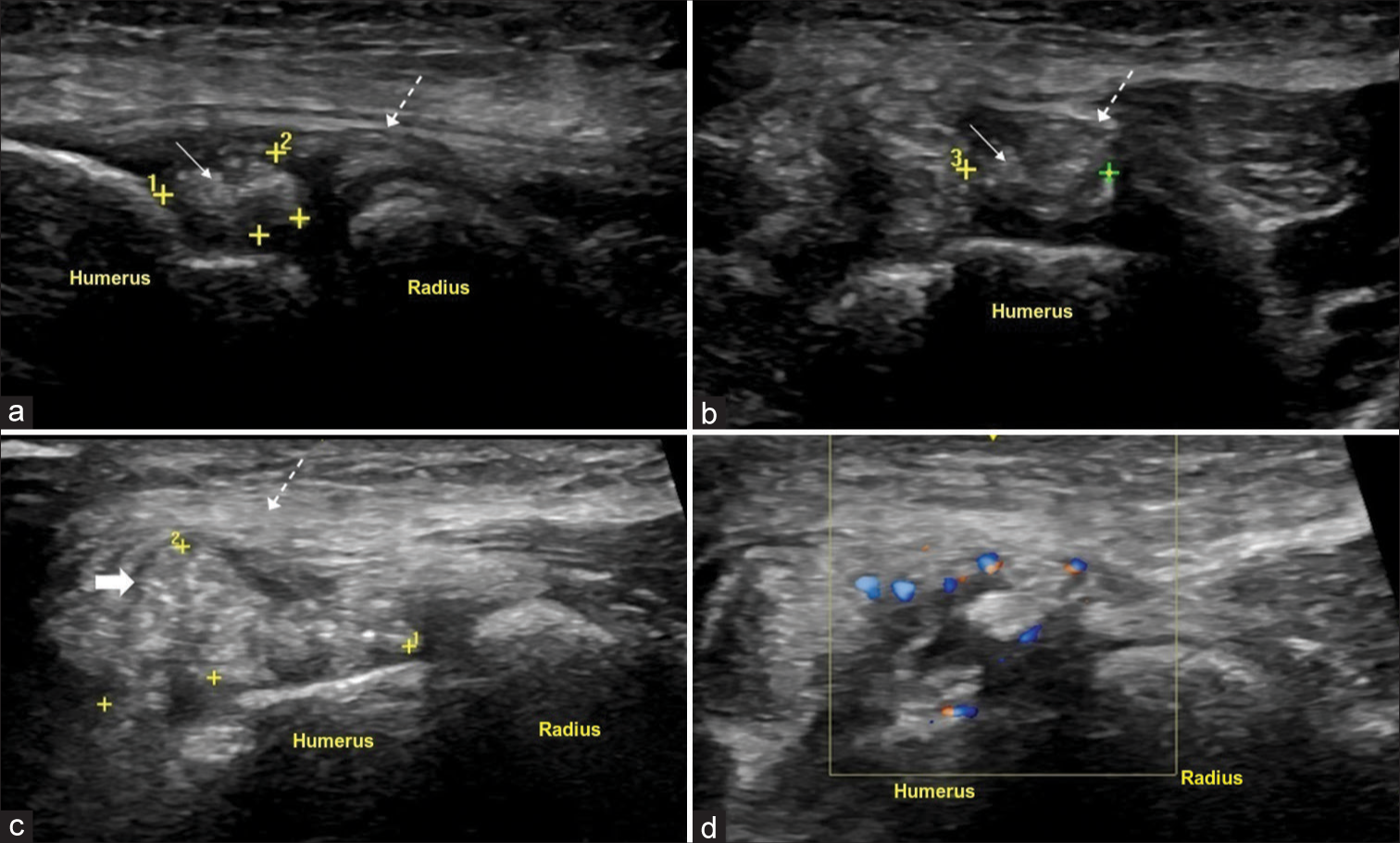
- A 35-year gentleman presented with pain and stiffness over the lateral aspect of the right elbow one year after he had a fall from a bike, now patient complained of aggravation of pain for the past 3 days. (a, b) High resolution ultrasound (HRUS) showed (thin arrow) a focus of type 2 calcification was seen within the humeral attachment of the radial collateral ligament. (c) Another (thick arrow) large amorphous type 3 focus of calcification within the (dotted arrows in a,b,c) posterior part of the common extensor origin with the surrounding fluid, fat stranding and (d) grade III hyperaemia on power Doppler. The + symbol is caliper that comes when any measurement is taken in an ultrasound machine. +1 means first measurement. +2 means second measurement.
Case 3
A 42-year-old lady came to the department with pain in her left wrist for three months, which was exacerbated over the past five days. On examination, there was swelling and redness in the anterior aspect of the distal forearm and wrist. HRUS [Figure 3] showed a few large Type 3 calcifications in the carpal tunnel underneath the flexor tendons. The largest focus of calcification had an anechoic matrix suggestive of liquefaction of the calcium.
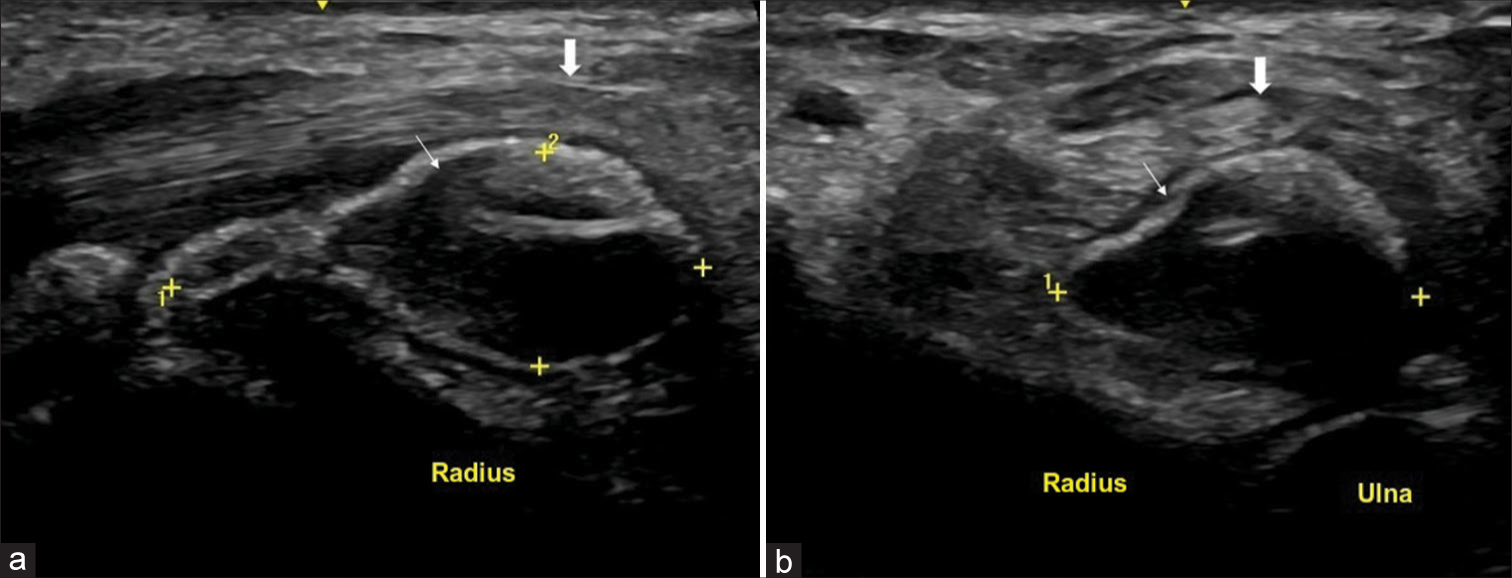
- A 42-year-old lady came to the out patient department with pain in her left wrist for 3 months, which was exacerbated over the last 5 days. (a) High resolution ultrasound (HRUS) long-axis and (b) short-axis showed few large type 3 calcifications in the carpal tunnel, underneath the flexor tendons. The largest (thin arrow) focus of calcification measuring 26 x 16 x 9 mm had an anechoic matrix suggestive of liquefaction of the calcified core. There was associated (thick arrow) tenosynovitis of the overlying flexor tendons. The + symbol is caliper that comes when any measurement is taken in an ultrasound machine. +1 means first measurement. +2 means second measurement.
All three patients were offered an ultrasound-guided barbotage in the same outpatient department setting. Since all three cases, the calcifications had liquefied components, they were amenable to a USG-guided aspiration, and subsequently, dry needling of the gritty foci was also done. The procedure was explained in detail to the patients in the discussion session.
Below are the real-time videos of the procedure performed in all three cases in the same clinical setting [Videos 1-3].
Video 1:
Video 1:In case 1, dry needling of the gritty foci along the floor of the bicipital groove was done in an attempt to break it into small fragments. It was followed by an aspiration of calcifications. The movement of the calcifications within the needle is visible. It was followed by barbotage with normal saline injection and gentle pulsing was done so that calcific fragments were suspended into the saline. After completion of the procedure, 40 mg of triamcinolone acetonide was injected at the site.Video 2:
Video 2:In case 2, the aspiration of the liquefied Type 3 calcifications within the posterior part of the common extensor origin was done. It was followed by dry needling of the gritty foci and injection of triamcinolone acetonide at the end of the procedure.Video 3:
Video 3:In case 3, the liquefied core of the large focus of calcification in the distal forearm underneath the flexor tendons was aspirated. It was followed by injection of normal saline injection and 40 mg of triamcinolone acetonide.DISCUSSION
Ultrasound-guided aspiration and barbotage are an effective, minimally invasive method of treatment in patients with calcific tendonitis, especially those who have severe pain that does not respond to conservative management, that is, oral analgesics, physical therapy[6] and also for cases of severe acute calcific tendonitis with rupture of the Type 3 calcium into the peritendinous tissues.[7] The procedure consists of needling the calcification to break it down into small fragments, followed by lavage using normal saline to remove these fragments. Usually, it is followed by a bursal steroid injection to reduce inflammation.
Pre-requisites for the procedure
Materials
Chlorhexidine solution, betadine solution, sterile drape, sterile gauze, 2% lignocaine injection, normal saline, 18-gauge needle, 10 cc syringe, and triamcinolone acetonide 40 mg/mL.
At least, two people are required to perform the procedure. Any joint and skin infection is to be ruled out. The patient should be explained about the procedure and its possible complications. Written, informed consent should also be taken. The calcific tendinopathy does not fall into the spectrum of inflammatory disorders; therefore, the inflammatory markers are not elevated. Routinely, laboratory investigations are not done unless there was a history of bleeding disorder and also ruling out systemic diseases or medications predisposing to prolonged bleeding.
Procedure
The patient is put in the optimum position, depending on the procedure. The entry site should be cleaned with betadine and chlorhexidine in an inside-out manner and then draped with a sterile cloth. The expected needle track, that is, skin and the underlying soft tissues, should be anesthetized with 2% lignocaine. Under ultrasound guidance, an 18-gauge needle should be advanced to the calcification parallel to the long axis of the probe, so that the entire needle is visualized, that is, “in-plane” technique. The entry site of the needle should be slightly away from the probe if the calcification is deeper, and the entry site should be close to the probe if the calcification is superficial. Dry needling is attempted to break it into small fragments. Then, normal saline is injected and gentle pulsing is done so that calcified fragments suspend into the saline. It is then followed by an aspiration of this saline with suspended calcifications. This process of saline injection and aspiration can be repeated to remove the residual calcifications. Another method is using two needles, one for injecting saline and the other one for aspiration. In this double-needle technique, the first needle is inserted into the deeper portion of the calcification with the needle bevel directed upward, while the second needle is inserted into the superficial portion of the calcification parallel and above the first needle with its bevel directed downward.[8,9] After completion of the procedure, 40 mg of triamcinolone acetonide is injected into the adjacent bursa or peritendinous region. Care should be taken not to inject the steroid into the tendon. The injection of steroid is avoided in patients with diabetes mellitus, which could potentially lead to a rise in the blood sugar level. The needle is removed, and hemostasis is achieved. A sterile dressing is applied at the entry site.
There is increased resorption of the residual calcifications after the procedure; hence, all the calcifications need not necessarily be removed during the procedure.
Post-procedural
The patient is given oral analgesics to relieve the pain and should continue physiotherapy. Complications include vasovagal reactions, hematoma formation, infections, and rarely tendon rupture.
A randomized controlled trial by De Witte et al. showed that there was a significant reduction in the size of the calcification with ultrasound-guided barbotage with bursal steroid injection versus only subacromial-subdeltoid bursa corticosteroid injection.[10]
The best results of ultrasound-guided barbotage are seen in patients with Types 2 and 3 calcifications. The success rate with large Type 1 calcification is limited, and the ideal treatment in this case is arthroscopic removal. However, smaller Type 1 calcifications are amenable to barbotage.[11]
Conservative management includes non-steroidal anti-inflammatory drugs and physical therapy. The other methods of treatment are ultrasound therapy and extracorporeal shock wave therapy, along with passive benign exercise to restore range of motion. The ultrasound-guided barbotage was superior as compared to extracorporeal shock wave therapy in regard to clinical improvement and pain relief.[12,13] If the patient does not respond to conservative management, he can be offered open or arthroscopic surgery to remove calcific deposits.[14]
CONCLUSION
Ultrasound-guided aspiration and barbotage is a simple, minimally invasive procedure for the treatment of severe acute calcific tendonitis that can be performed as a day-care procedure in the same setting. It can be considered the treatment of choice for severe acute calcific tendonitis with rupture into the peritendinous tissues. Calcifications can occur in very unusual sites, as elicited in the above article. High-resolution ultrasound can serve as a one-stop shop for the diagnosis and management of this highly debilitating condition.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available online at
Financial support and sponsorship
Nil.
References
- Calcific tendinitis: Intramuscular and intraosseous migration. Diagn Interv Radiol. 2019;25:480-4.
- [CrossRef] [PubMed] [Google Scholar]
- Calcific tendonitis: Natural history and association with endocrine disorders. J Shoulder Elbow Surg. 2007;16:169-73.
- [CrossRef] [PubMed] [Google Scholar]
- Calcifying tendinopathy: A local or a systemic condition? Rev Bras Ortop. 2015;47:479-82.
- [CrossRef] [Google Scholar]
- Calcific tendinopathy of the rotator cuff: Pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997;5:183-91.
- [CrossRef] [PubMed] [Google Scholar]
- The role of ultrasound guided percutaneous needle aspiration and lavage (barbotage) in the treatment of calcific tendinitis. Egypt J Radiol Nucl Med. 2015;46:63-70.
- [CrossRef] [Google Scholar]
- Ultrasound appearance of the migration of tendon calcifications. J Ultrasound Med. 2019;38:2493-506.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound guided barbotage In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- [Google Scholar]
- Double-needle ultrasound-guided percutaneous treatment of rotator cuff calcific tendinitis: Tips and tricks. Skeletal Radiol. 2013;42:19-24.
- [CrossRef] [PubMed] [Google Scholar]
- Calcific tendinitis of the rotator cuff: A randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med. 2013;41:1665-73.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound imaging-guided percutaneous treatment of rotator cuff calcific tendinitis: Success in short-term outcome. Br J Radiol. 2016;89:20150407.
- [CrossRef] [PubMed] [Google Scholar]
- Which method is more effective in treatment of calcific tendinitis in the shoulder? Prospective randomized comparison between ultrasound-guided needling and extracorporeal shock wave therapy. J Shoulder Elbow Surg. 2014;23:1640-6.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided percutaneous irrigation of calcific tendinopathy. Semin Musculoskelet Radiol. 2016;20:409-13.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of calcific tendinitis of the shoulder. Clin Shoulder Elbow. 2020;23:210-6.
- [CrossRef] [PubMed] [Google Scholar]






