Translate this page into:
Bicipitoradial bursitis and biceps tendinitis: Repetitive use versus rheumatoid arthritis

*Corresponding author: Daniel Victor Šimac, Department of Rheumatology and Clinical Immunology, Clinical Hospital Center Rijeka, Rijeka, Croatia. danielsimac@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Simac DV, Mayer M. Bicipitoradial bursitis and biceps tendinitis: Repetitive use versus rheumatoid arthritis. Indian J Musculoskelet Radiol. 2023;5:143-5. doi: 10.25259/IJMSR_19_2023
Abstract
Bicipitoradial bursitis (BRB) is the inflammation of the bicipitoradial bursa, a bursa located in the cubital fossa between the biceps tendon and radial tuberosity. It is a relatively uncommon condition mostly attributed to repetitive use; however, it can be associated with other conditions, including rheumatoid arthritis (RA). We present a 52-year-old woman who presented with novel joint pain with swelling lasting 2 months with elevated rheumatoid factor (RF) 246.2 IU/mL and anti-cyclic citrullinated peptide (CCP) antibodies >1200 IU/mL, highly suggestive of RA. It should be noted the patient works as a butcher, with earlier conditions, including carpal tunnel syndrome (CTS) which was operated on. The patient also had numbness of the right hand with electromyoneurography (EMNG) suggestive of CTS relapse and noticed swelling of the cubital fossae. As a part of the workup, a right elbow ultrasound was done showing a mass, which was confirmed by magnetic resonance imaging as BRB. Given the clinical picture, elevated RF and anti-CCP antibodies, and BRB, it was concluded that the patient likely has early RA, and BRB as a result of both repetitive use in combination with the early RA onset which possibly exacerbated an earlier, stable condition. BRB can be large enough to compress local neural structures causing symptoms, which may be an explanation for the EMNG result of CTS relapse, possibly caused by BRB instead as CTS relapse is relatively uncommon. Although a rare condition usually attributed to repetitive use, BRB can also be associated with other conditions including RA as in our case.
Keywords
Bicipitoradial bursitis
Rheumatoid arthritis
Musculoskeletal ultrasonography
INTRODUCTION
Bicipitoradial bursitis (BRB), the inflammation of the bicipitoradial bursa, a bursa located in the cubital fossa between the biceps tendon and radial tuberosity, is relatively uncommon.[1-4] The condition presents with cubital fossa swelling, joint pain, and limitation in movement, and compression of the radial or median nerves, with associated symptoms, is also possible.[1-4] It is usually attributed to repetitive use, that is forearm supination and pronation and may be accompanied by biceps tendon pathology.[1,3] Other causes are possible, including rheumatoid arthritis (RA) or spondyloarthropathy.[1-3] Diagnosis is made based on anamnesis, physical examination, and imaging, notably magnetic resonance imaging (MRI) and ultrasound, which also allows for aspiration or injection for diagnosis or treatment.[1-4] Surgical treatment is an option if conservative treatment is unsuccessful.[1]
CASE REPORT
A female patient, at 52 years old, with a history of cervicobrachial and lumbosacral syndromes, and carpal tunnel syndrome (CTS), with earlier operative treatment of an L5/S1 discus hernia and bilateral carpal tunnel decompression, first presented to our department in spring 2022 with novel joint pain with swelling and morning stiffness the past 2 months, numbness in the right hand with electromyoneurography (EMNG) suggestive of CTS relapse, despite earlier surgical treatment, and elevated rheumatoid factor (RF) 246.2 IU/mL and anti-cyclic citrullinated peptide (CCP) antibodies >1200 IU/mL; antinuclear antibodies (ANAs) were also done and negative. The patient also had bilateral antecubital swelling, and it is important to note that the patient works as a butcher. Seropositive early RA was suspected, a workup was ordered, and prednisone was initiated which saw some improvement.
Initial workup included laboratory tests, hand and foot radiographs, and hand ultrasound, which interestingly did not yield results suggestive of systemic inflammatory arthritis such as RA, inflammatory markers were normal, joint radiographs showed degenerative changes, and hand ultrasound did not show any inflammatory activity. During the hand ultrasound, due to the antecubital fossa swelling, the right elbow was also examined, which showed a large heterogeneous hypo- to isoechogenic mass around the biceps tendon with thickening and roughness at the insertion point on the radius, thought to be a possible hematoma, synovitis, or combination, with a possible rupture of the biceps tendon [Figure 1]. An MRI was ordered, which showed signs of advanced distal biceps tendinitis with the erosion of the radial tuberosity at the insertion point, and an oval-shaped bordered collection (25 mm × 13 mm × 12 mm), with homogeneous isointense signal in T1-weighted images and high border signal and inhomogeneous hypointense content in proton density fat saturation images, which corresponded to BRB [Figure 2]. The patient was referred for an orthopedic consult.
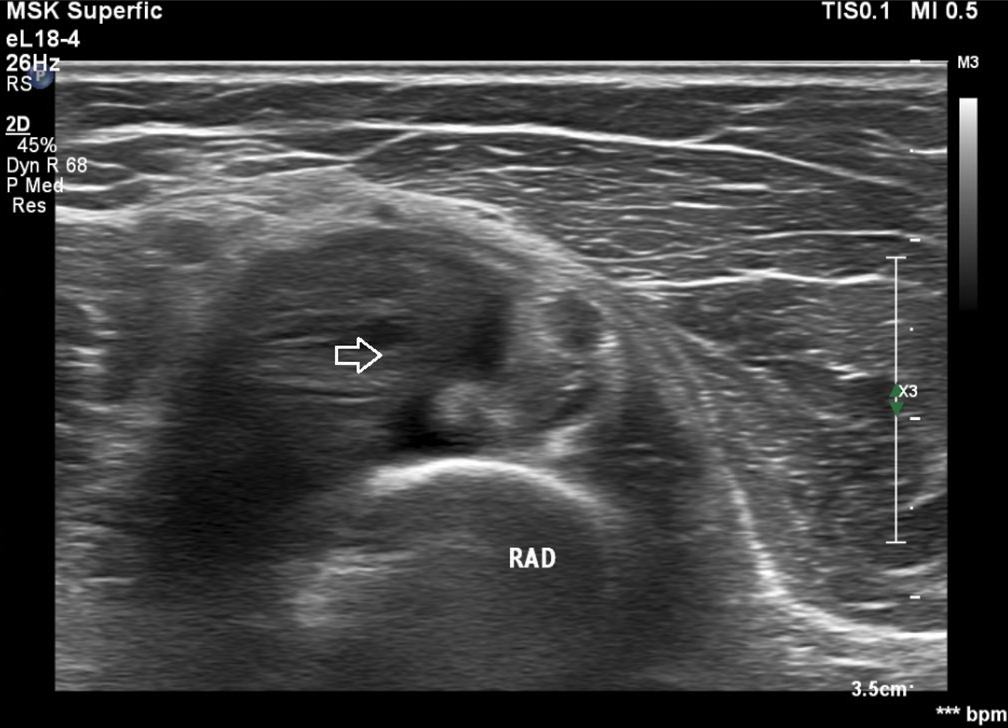
- Ultrasound image of nonspecific mass in antecubital fossa of the right elbow. Arrow: Mass, RAD: Radius.
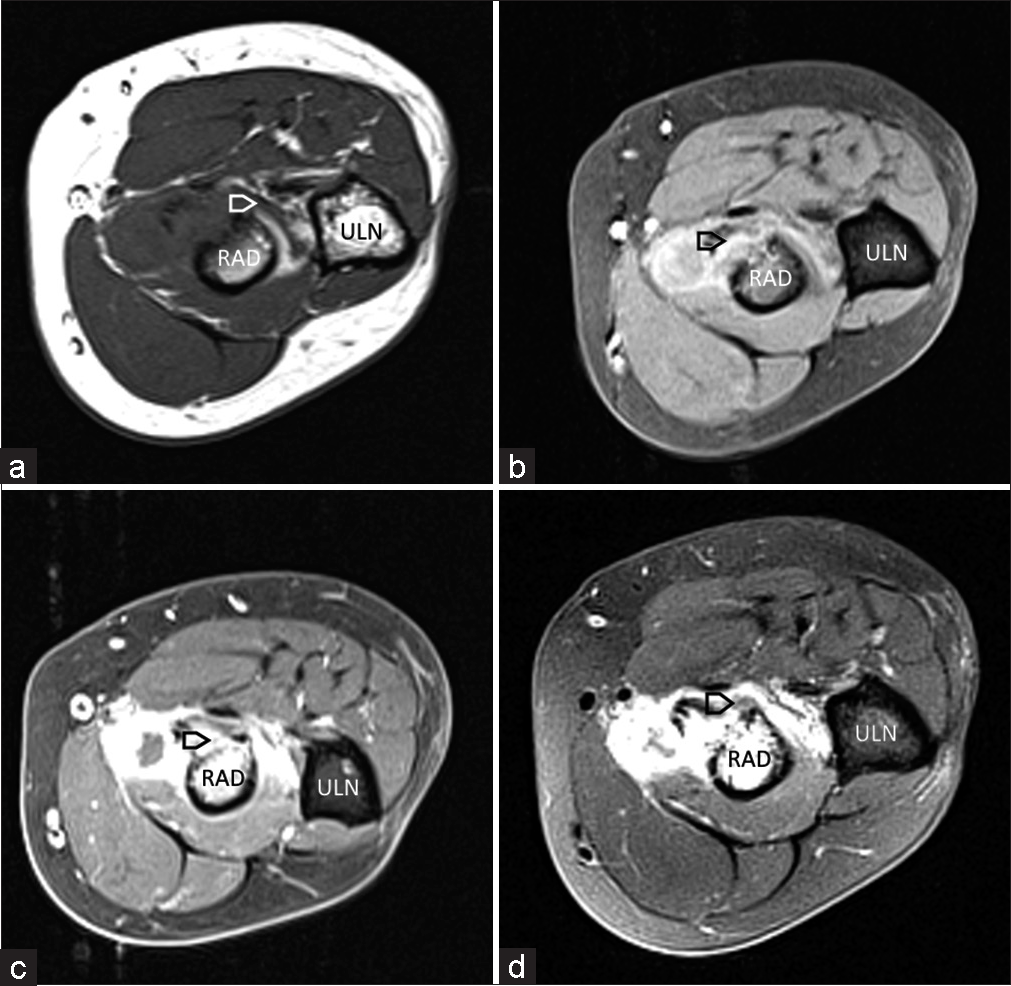
- (a-c) T1-weighted MRI images of mass in antecubital fossa of the right elbow, corresponds to bicipitoradial bursitis (BRB). (d) Proton density fat saturation image of mass in antecubital fossa of the right elbow, corresponds to BRB. Arrow: BRB, RAD: Radius, ULN: Ulna.
Given the clinical picture, along with high RF values and anti-CCP antibodies, in spite of the absence of inflammatory markers in laboratory test results and activity on the ultrasound, RA was still suspected, and sulfasalazine was initiated. It was concluded that the BRB and biceps tendinitis is the result of repetitive use exacerbated by RA. The right-hand numbness may also be a result of BRB instead of CTS relapse.
DISCUSSION
Diagnosing early RA can be challenging,[5] the patient in our case is no exception, especially after managing such an early referral. The clinical picture of pain with swelling in the joints, with morning stiffness, and it should be noted that the joints were symmetrically affected, with elevated RF and anti-CCP antibodies, is highly suggestive of early RA.[5] Still, the history of mechanical and degenerative problems may be misleading, but it is important to note that the complaints in our patient were novel and different from earlier issues. The lack of elevated inflammatory markers is also misleading, but it is known that inflammatory markers can be normal in up to 60% of early RA patients.[5] There were no significant changes, nor erosions, on hand and foot radiographs, but likely it was too early for significant changes to be seen, over 70% of radiographs can be normal in early disease.[5] Inflammatory activity was missing on ultrasound, that is erosions, synovitis, or power Doppler activity. Although ultrasound in rheumatology has come a long way, routinely used in our center, and early changes can be seen and correlate to disease activity, especially in follow-up and for accessing treatment, these changes are not always seen.[6] Other diagnoses are possible, such as spondyloarthritis or systemic autoimmune disease, but are less likely given elevated RF and anti-CCP antibodies, and negative ANA.
BRB and biceps tendinitis discovered using ultrasound and confirmed using MRI are changes often associated with repetitive use as mentioned, which can undoubtedly be attributed to our patient working as a butcher, especially with earlier mechanical conditions, and although the condition is rare, it has been associated with RA.[1-4] Likely, bursitis and tendinitis, in this case, is a combination of repetitive use with the onset of RA, and possibly, RA exacerbated an earlier, stable condition. The numbness in the right hand should also be commented on, as the patient had an EMNG test result attributed to CTS relapse. Given the fact that surgically treated CTS relapse is not that common, ranging from 3% to 25%, usually due to unsuccessful surgical treatment or scarring, and given that BRB can compress nearby neural structures and cause symptoms, it is more likely the symptoms and EMNG results in our patient were a result of bursitis, not CTS.[7]
CONCLUSION
BRB, although a rare condition associated with repetitive use, can be associated with other conditions, including RA as in our case.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Bicipitoradial bursitis: A review of clinical presentation and treatment. J Orthop Trauma Rehabil. 2014;18:7-11.
- [CrossRef] [Google Scholar]
- Bicipitoradial bursitis: MR imaging findings in eight patients and anatomic data from contrast material opacification of bursae followed by routine radiography and MR imaging in cadavers. Radiology. 1999;212:111-6.
- [CrossRef] [PubMed] [Google Scholar]
- Bicipitoradial bursitis: A diagnosis challenge! Clin Case Rep. 2020;8:2265-8.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative diagnosis of bicipitoradial bursitis: A case report. Pan Afr Med J. 2014;17:41.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of early rheumatoid arthritis: What the non-specialist needs to know. J R Soc Med. 2004;97:421-4.
- [CrossRef] [PubMed] [Google Scholar]
- The discriminatory capacity of ultrasound in rheumatoid arthritis: Active vs inactive, early vs advanced, and more. Rheumatology (Oxford). 2012;51:vii, 6-9
- [CrossRef] [PubMed] [Google Scholar]
- Does recurrence of carpal tunnel syndrome (CTS) after complete division of the transverse ligament really exist? J Clin Med. 2021;10:4208.
- [CrossRef] [PubMed] [Google Scholar]







