Translate this page into:
Bone Tumors Management Survey in India – Radiologist Perspective

*Corresponding author: Rajesh Botchu, Department of Musculoskeletal radiology, Royal Orthopedic Hospital, Bristol Road South, Birmingham 312, United Kingdom. drbrajesh@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Vemuri NV, Songa R, Azzopardi C, Thaker S, Gupta H, Botchu R. Bone Tumors Management Survey in India – Radiologist Perspective. Indian J Musculoskelet Radiol 2020;2(2):108-14.
Abstract
Bone tumors are rare and the management of these in India is variable. We did a survey of the radiologists in India to assess the management of bone tumors. We discuss the results of the survey propose some guidelines and suggestion from a radiologist perspective.
Keywords
Bone
Tumor
Survey
India
INTRODUCTION
Bone tumors are relatively uncommon, constituting only 0.5% of global cancer incidence among all types of cancers.[1] In 2007, Gulia et al. performed a retrospective study to determine the occurrence of bone and soft-tissue tumors in India, which demonstrated that of all musculoskeletal neoplasms, around 60% were bone tumors and 36% were soft-tissue tumors. Of bone tumors, 66% were malignant, 15% were benign, and 19% were non-neoplastic. Furthermore, osteosarcoma was the most common malignant tumor and giant cell tumor was the most common benign tumor.[2]
Imaging and biopsy
Correct diagnosis and further management of the bone tumors is quite challenging. Radiological diagnosis of suspected bone tumors typically involves multimodality imaging including plain radiographs, computed tomography (CT), magnetic resonance imaging (MRI), and bone scans. The plain radiograph, although primary imaging modality, is a cornerstone for bone tumor evaluation, which assesses the location, matrix, characterization, and aggressiveness of the tumor. An aggressive appearing lesion should be considered malignant until proven otherwise and biopsy should be done in such lesions. Before biopsy, a cross-sectional imaging is necessary to stage the tumor and decide biopsy route that produces high yield with minimal complications. MRI is the best imaging modality for establishing soft-tissue involvement and local staging. CT can be used as an adjunct with MRI to evaluate cortical based tumors and periosteal reaction.[3]
Apart from few lesions such as enchondroma, osteochondroma, osteoid osteoma, simple bone cyst, fibrous dysplasia, or non-ossifying fibroma demonstrating pathognomonic appearance on radiographs and other imaging modalities, rest of the bone tumors need histopathological examination to ascertain type, aggressiveness, and histopathological grade the lesion.[3]
Radiological and histopathological grading of tumors is particularly important with the increasing use of limb-salvage surgery (LSS) as primary treatment for musculoskeletal malignancies. It serves as a prognostic marker and determines the need for neoadjuvant chemotherapy and possible radiotherapy. Biopsy techniques employed for tissue diagnosis may be percutaneous (fine-needle aspiration and core needle biopsy [CNB]) or open biopsy (incisional or excisional).
CNB is more accurate than fine-needle aspiration and open biopsy is considered more accurate than both these procedures. Comparative study conducted by Layfield et al. revealed that open biopsy had the highest diagnostic accuracy (89–95%) than core biopsy (78–84%); however, rate of complications is higher with open biopsy (17%) compared to CT-guided percutaneous CNB (1.1%) and image-guided biopsy is considered the gold standard.[4,5]
Meta-analysis by Suh and Yun over 15 studies and 969 sclerotic bone lesions concluded that the diagnostic yield of image guided percutaneous CNB of sclerotic lesion is 74% and diagnostic accuracy is 87%.[6]
Percutaneous core biopsy is a minimally invasive daycare procedure with low risk of contamination, biopsy track seeding, fewer complications, and diagnostic accuracy comparable to open biopsy. Jelinek et al. even proposed that in cases of non-diagnostic image-guided biopsy with CNB, open-procedure biopsy is likely to be associated with similar diagnostic difficulties.[7] However, open biopsy increases the risks of local contamination and clinical morbidity, with a worse prognosis in 8% of cases and increased risk of amputation.[8] In deep bone tumors, coordination with ultrasound or CT guidance increases the diagnostic accuracy.[9]
Survey of current practices in India
A multidisciplinary team approach, including radiologists, orthopedic oncosurgeons, and sarcoma pathologists, is an absolute prerequisite for adequate treatment of bone tumors and often a challenge. Situation in India is further complicated by lack of logistical (i.e., limited numbers of centers of excellence providing holistic tertiary care for bone tumors, lack of robust referral system, and vast demography) and workforce (inadequate numbers of musculoskeletal radiologists and orthopedic oncologists and sarcoma pathologists) support. Subspecialty radiology training, especially musculoskeletal radiology with a view to further sarcoma imaging, is very limited.[3]
The number of radiologists catering Indian population is substantially low compared to their Western counterparts. Statistically, in India, the radiologist to population ratio is approximately 1:100,000 compared to 4.8:10,000 in the UK and 10:10,000 in the US).[10] The role of radiologists in India, in suspected cases of bone tumors, is limited to identify, categorize, and tentatively stage the lesions and only a few radiologists perform image-guided bone tumor biopsy.
MATERIAL AND METHODS
With above in mind, we conducted a survey among 100 radiologists across India. This is an anonymous online survey. Each radiologist was given a series of 10 questions aiming to understand the confidence level, approach, biopsy techniques, and treatment practiced in India by radiologists [Tables 1 and 2].
| Questionnaire | Responses | |||
|---|---|---|---|---|
| Number of bone tumors seen by radiologist per year | <5 (21%) | 5–10 (27%) | >10 (52%) | - |
| Confidence level in diagnosing bone tumor | Very confident (12%) | Confident (70%) | Unsure (18%) | - |
| How many of the radiologist perform bone biopsy | Yes (48%) | No (52%) | - | |
| Responses towards approach after diagnosing bone tumor | Send report to referrer (42%) | Refer to regional bone tumor center (22%) | Do CT-guided biopsy by yourself (19%) | Ask for help (9%) and others (8%) |
| Biopsy planning | Myself (6%) | Discuss with referrer (31%) | Discuss with bone tumor specialist (41%) | Multidisciplinary meeting (22%) |
| Image based questionnaire | Responses | ||
|---|---|---|---|
| Long bone biopsy route | Route A: 23% | Route B: 63% | Route C: 14% |
| Spinal biopsy route | Route A: 47% | Route B: 17% | Route C: 34% |
| Biopsy recommended or not | Yes (19%) | Maybe (29%) | No (52%) |
| Treatment options | Analgesics (29%) | Surgery (24%) | Radiation ablation (47%) |
RESULTS
Out of 100 radiologists, 52% of radiologists report more than 10 tumors per year, 21% reports <5 tumors per annum while 27% reports 5–10 tumors [Graph 1]. Among them, though majority (82%) radiologists were confident in diagnosing bone tumors [Graph 2], only around half of them had performed bone tumor biopsy before [Graph 3].
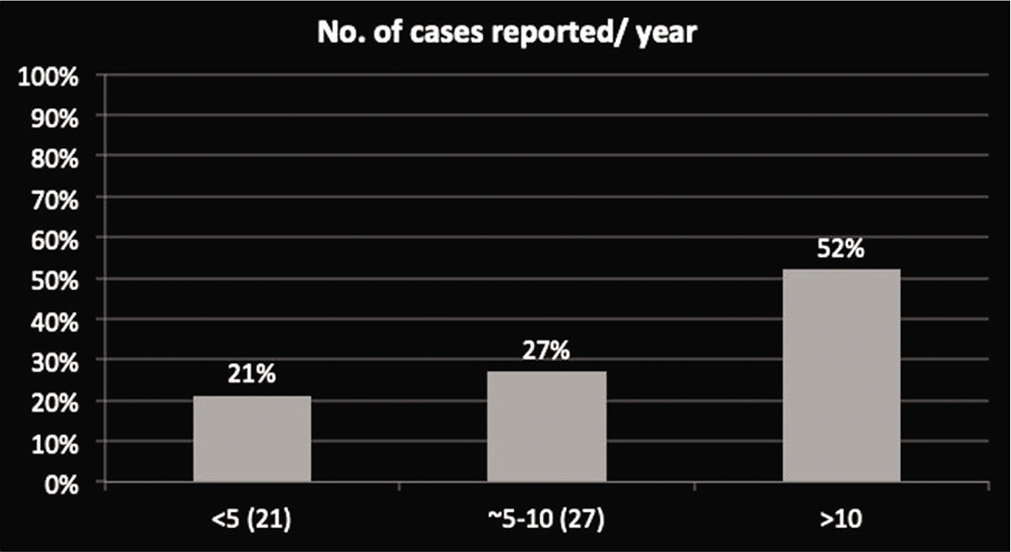
- Number of cases reported per annum by radiologist.
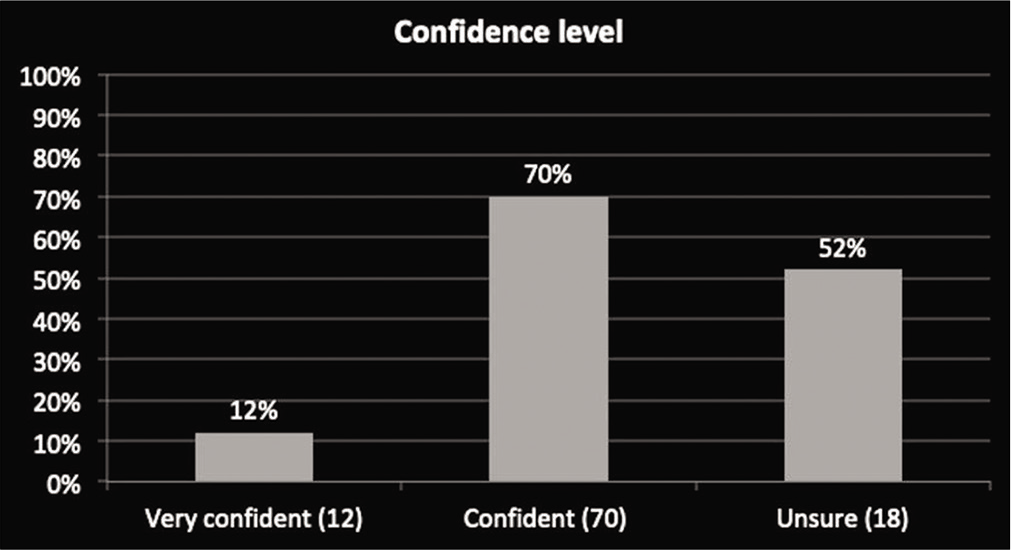
- Confidence level of radiologist in diagnosing bone tumor.
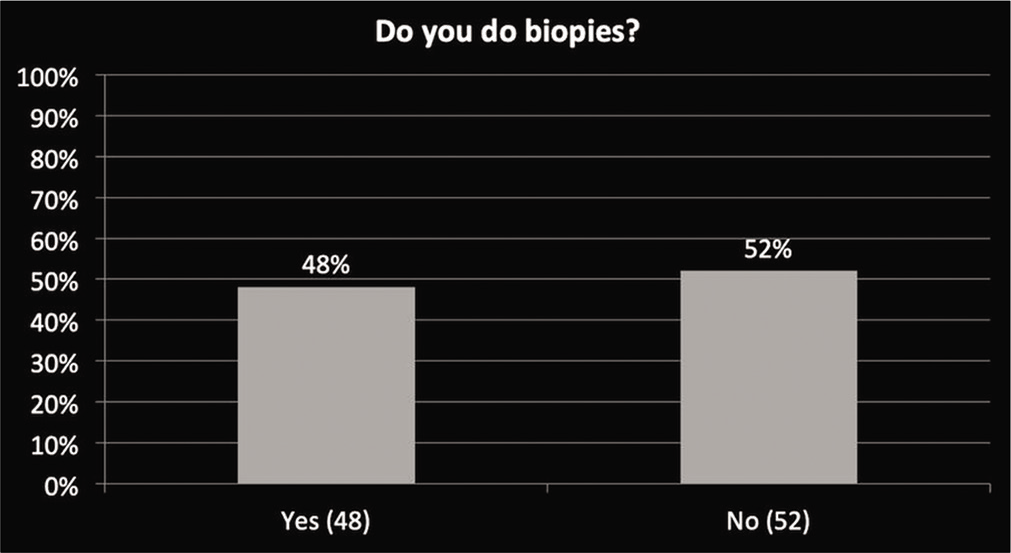
- Number of radiologist that do bone tumor biopsy.
Varied responses were noticed regarding the approach to the bone tumors where only 22% of radiologists refer the patient to regional bone centers. While most of the radiologists (88%), either send reports to the referrer (42%), do CT-guided biopsy themselves (19%) or ask for help or other responses (17%) [Graph 4].
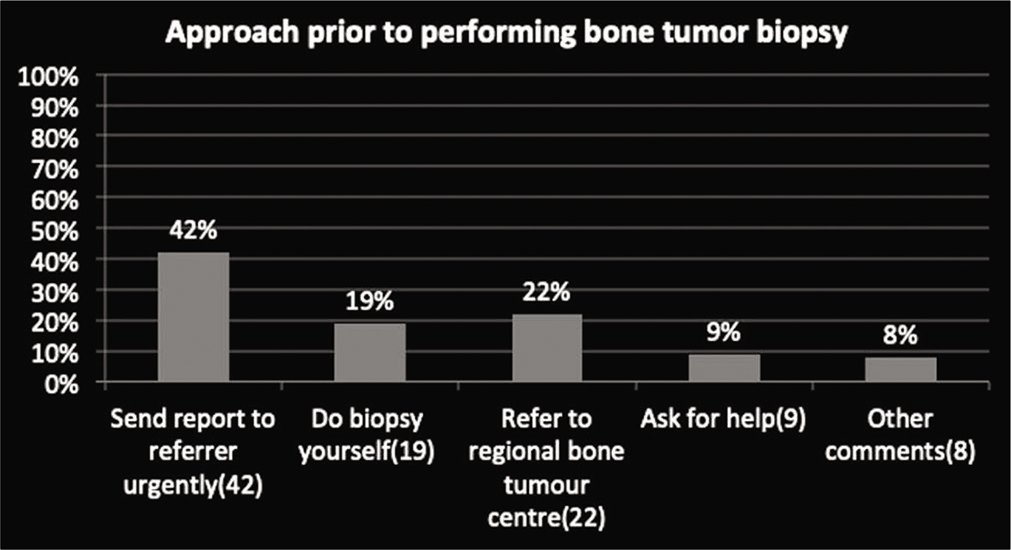
- Approach to the bone tumor.
Pertaining to the approach to the tumor, among 78 responses most of the radiologists, that is, around 63% of radiologists take an expert opinion before doing biopsy either from a bone tumor orthopedic specialist (41%) or from multidisciplinary meeting (22%), and 31% of radiologists discuss with the referrer [Graph 5].
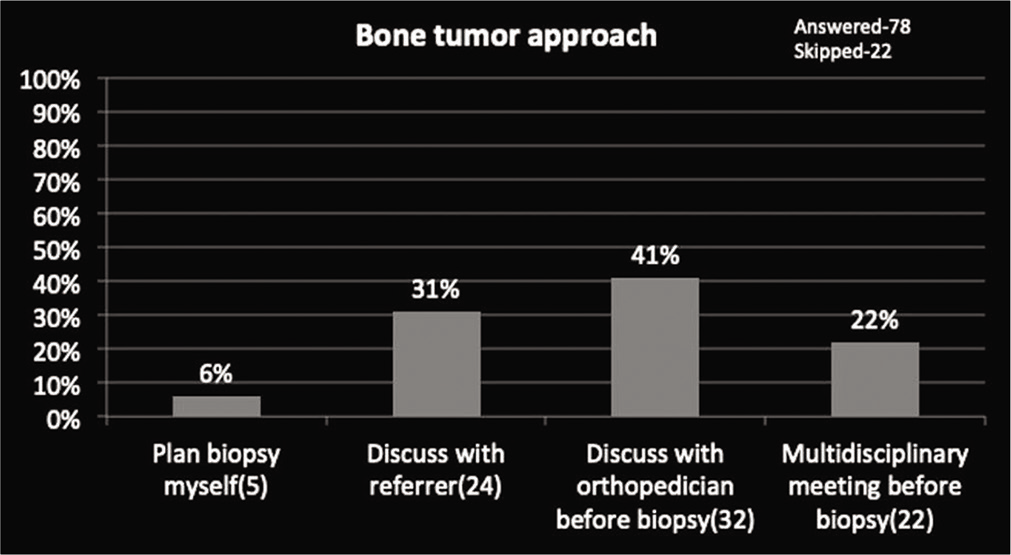
- Approach before performing bone tumor biopsy.
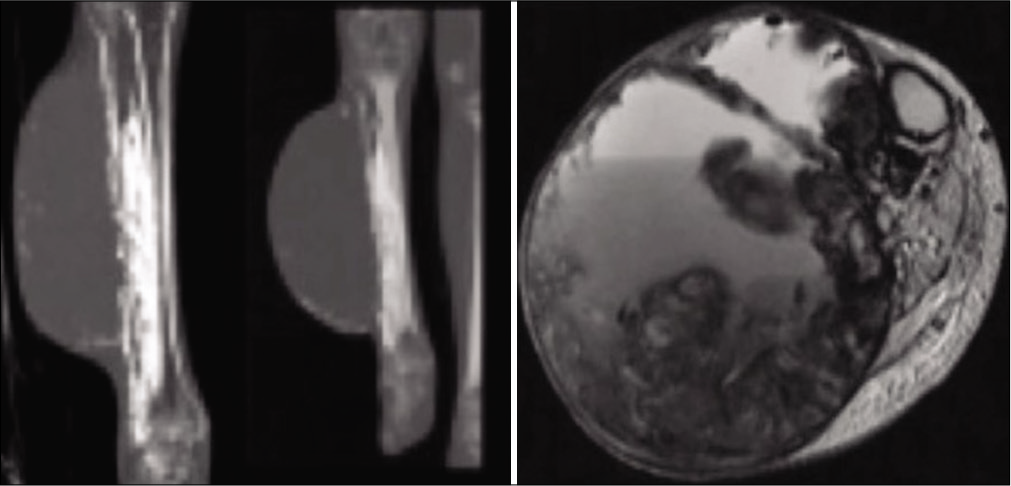
We received assorted responses regarding biopsy approach to extremity and spinal lesions, that is, 63% and 47% of radiologists chose an approach with least complications while rest of the radiologists, that is, 47% and 73% opted for other two options suggesting diversity in opinions [Graphs 6 and 7, Figures 1 and 2].
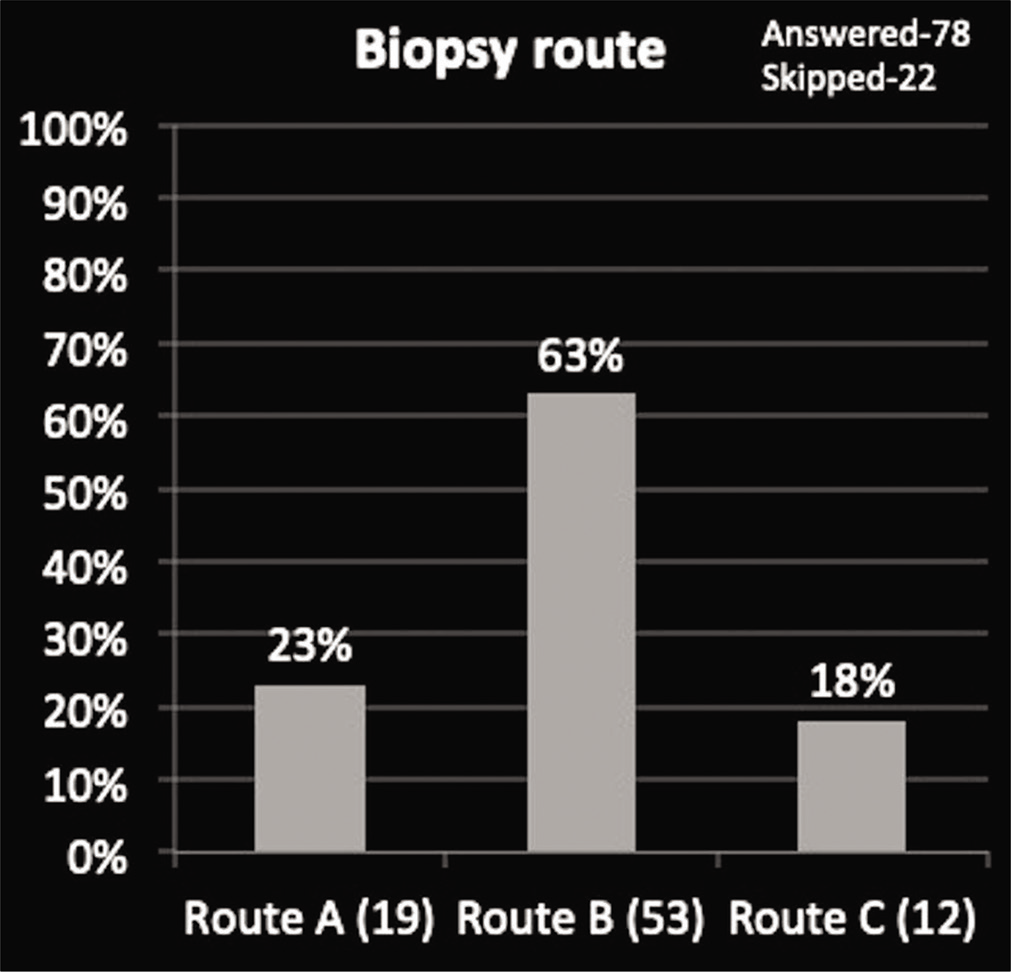
- Choice of biopsy route to the long bone tumor.
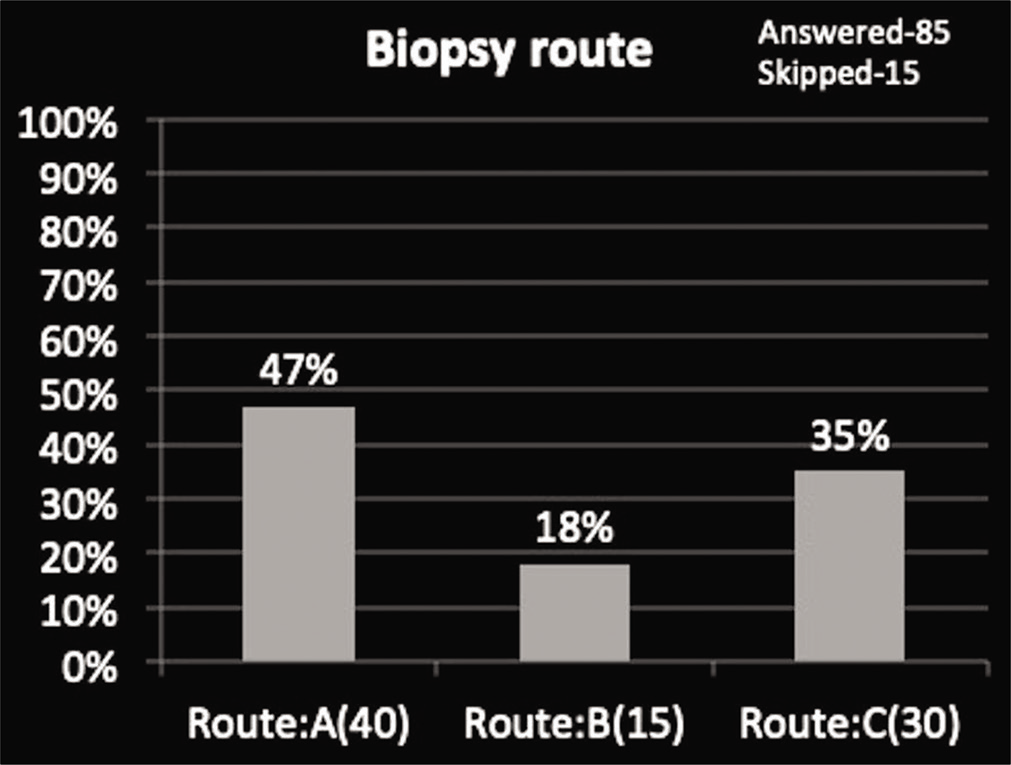
- Choice of biopsy route to the sacral tumor.
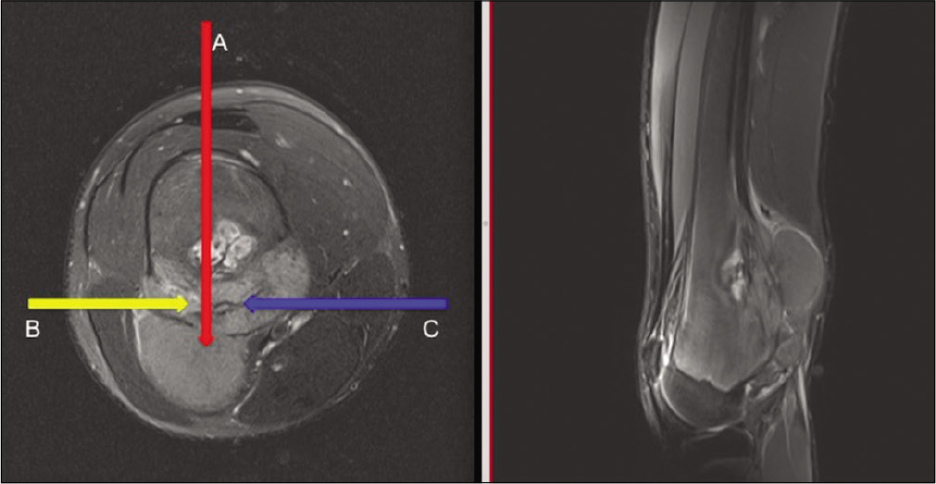
- Image of the femoral tumor with biopsy routes (A, B, and C).
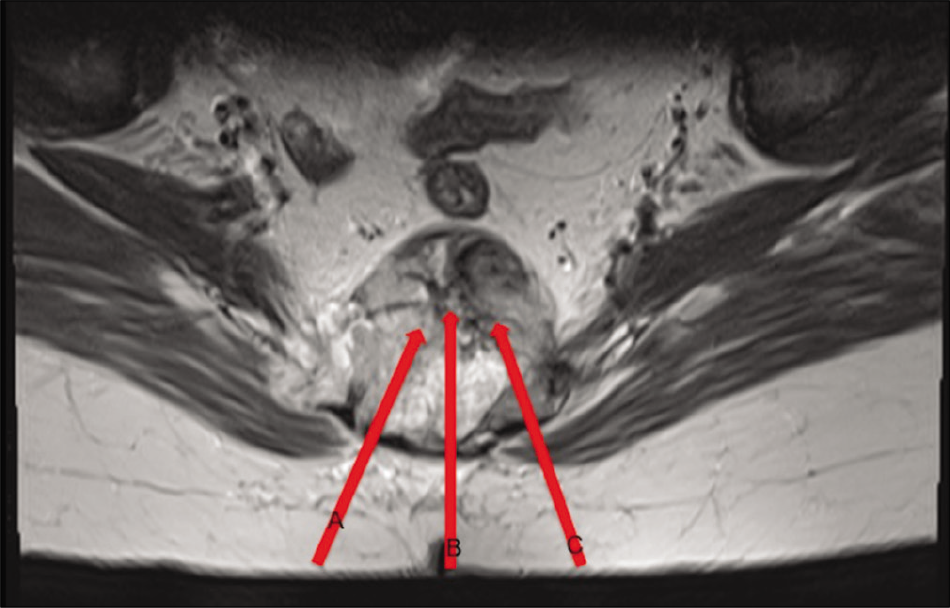
- Image of the spinal tumor with biopsy routes (A, B, and C).
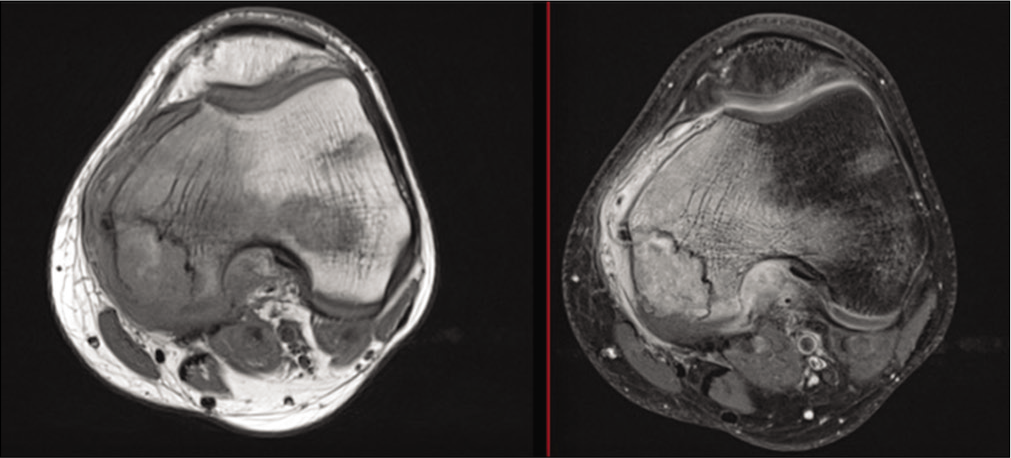
Concerning the treatment of a given lesion, out of three options, 47% of radiologists agreed with a single option (biopsy and radiofrequency ablation) while the rest of radiologists (53%) opted for the other two options (surgery and injection with painkillers) revealing farrago of choices [Graph 8 and Figure 3]. For a suspected case of bone tumor, around half of the radiologists opted to never do a biopsy, around one-fourth of radiologists opted to do a biopsy and remaining one-fourth of the radiologists were unsure [Graph 9 and Figure 4].
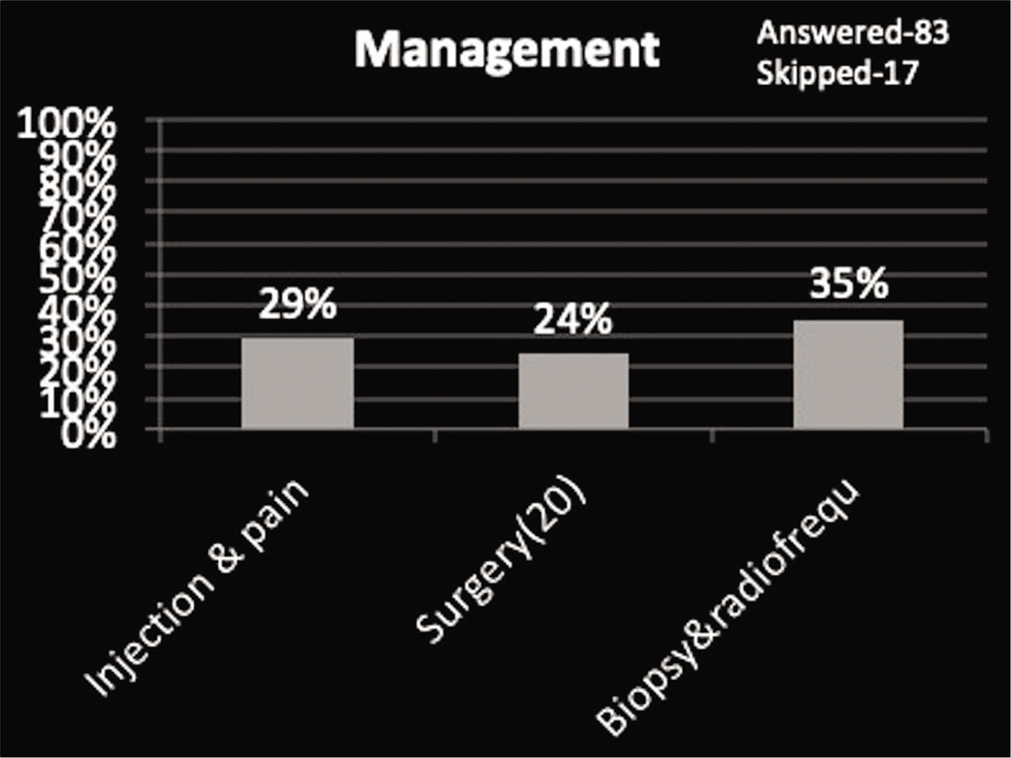
- Choice of treatment for chondroblastoma.
- Image of chondroblastoma with survey of treatment option.
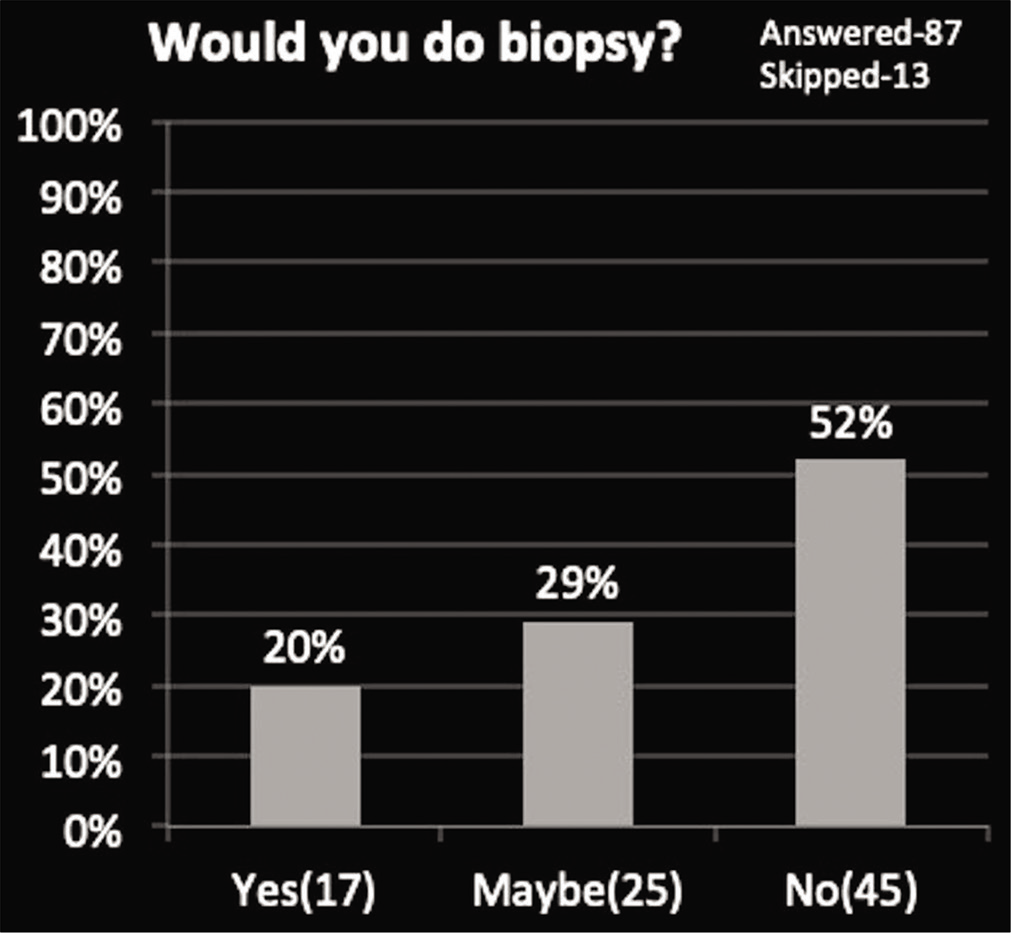
- Need for biopsy in a given lesion.
- Image of bone tumor with survey of need for biopsy.
DISCUSSION
Histopathological diagnosis is essential to stage the tumor, categorize its subtype, and plan further management. Although open biopsy is the gold standard for tissue sampling, image-guided percutaneous biopsy is investigation of choice because of its cost-effectiveness, low complications, and acceptable diagnostic yield. The study by Stoker et al. in 208 cases of bone tumors revealed that diagnostic accuracy of percutaneous needle biopsy was 97% comparable to open biopsy.[11] Pohlig et al. retrospectively compared percutaneous CNB with open surgical biopsy (SB) in 48 bone tumors. The diagnostic accuracies were 100% for CNB and 93.3% for SB.[12] Diagnostic accuracy is increased for percutaneous needle biopsy under image guidance, especially for deep-seated bone tumors.
Image-guided bone tumor biopsy remains a preferred and globally accepted method for histopathological diagnosis readily surpassing open biopsy, however, it has limited availability in India due to the availability of fewer specialist radiologists with expertise in performing imaging-guided musculoskeletal tumor biopsies, and according to our survey, more than half of radiologists never performed a bone tumor biopsy before and among the radiologists those who perform biopsies had diverse opinions regarding approach in a given bone tumor. Few Indian studies regarding diagnostic accuracy of image-guided core needle bone tumor biopsy were found in literature, however, none addressing the current practices, role of radiologist, and guidelines to be followed. Results from our study irrefutably depict the diversity in opinions among radiologists regarding biopsy approach and treatment of given bone tumor. Given the dire need to shift the paradigm from open biopsy to image-guided CNB, limited subspecialty radiologists and knowledge gap among general radiology population certain guidelines are necessary to maintain a degree of parallelism among the general radiologists performing bone tumor biopsies.
Probably major reasons, these differences exist among the general radiology community might be due to:
The need to coordinate biopsy approaches with surgical plans is unique to musculoskeletal tumors and, therefore, not widely known among radiologists in other subspecialty areas.
Bone tumors have been shown to recur locally from tumor seeding along biopsy tracks after CNB warranting en bloc resection of the tract.
Survival rates for patients who experience local recurrence of these sarcomas are very low, even after repeat surgery (often amputation) and chemotherapy.[13,14]
Indications and contraindications of tumor biopsy:[15]
Definitive diagnosis of bone lesion with indeterminate features
Definitive diagnosis of bone tumor with aggressive features and to determine its subtype for choosing appropriate management
Confirm/exclude metastasis in known primary malignancy
Confirm/exclude mass lesion causing pathological fracture.
Contraindication
Acute infection at the site of biopsy
Bleeding disorders
Inaccessible site.
Although there is no single definitive approach, few guidelines are to be followed before performing a bone biopsy (CT/USG).
The needle path should not open compartmental barriers, anatomic planes, joint space, and tissue area around neurovascular bundles and if possible compartmental tumor contamination should be contained to preserve function.
The shortest distance to the lesion is not necessarily the optimal route unlike in other tumors.
The biopsy tract and immediate surrounding tissue be removed en bloc with the tumor at the time of resection.[13,14
If soft-tissue component of bone tumor exists, biopsy should be taken from it. However, in cases where soft-tissue component infiltrating vastus lateralis muscle, plan the biopsy to avoid rectus muscle to retain extensor function of the knee.
If cortex is to be breached, an oblong-shaped round edged entry is preferred to retain maximum residual strength to prevent pathological fracture.[16]
In USG-guided bone tumor biopsy with soft-tissue component, solid tumor with vascularity must be the target to increase yield.
Anatomically based guidelines can be used by the radiologists to plan image-guided core needle biopsies of extremity long bone lesions that may be treatable with LSS proposed by Patrick et al.[9]
Preprocedural planning
-
Cross-sectional imaging (CT/MRI).
To determine nature of lesion (aggressive/ indeterminate features).
To plan best biopsy route following sarcoma principles (shortest possible route without violating sarcoma principles).
For selective tissue sampling part of tumor that results in high yield (avoiding cystic and necrotic component).
Multidisciplinary meeting if possible/communicating with operating surgeon and deciding appropriate route of biopsy.
Coagulation profile and platelet counts.
Procedural planning
Appropriate patient positioning depending on site of bone tumor for easy accessibility.
Strict aseptic conditions.
Good local anesthesia/sedation/general anesthesia.
Selecting appropriate bone biopsy needle depending on location and nature of lesion, cortical breach, and tumoral soft-tissue component.
At least two good samples.
CONCLUSION
A more flexible approach is a necessity in India toward bone tumors due to limited specialist bone tumor centers and experienced MSK radiologists. Our survey concludes that though most of the general radiologists in India are confident in diagnosing bone tumors, there been a substantial diversity in opinions and lack of parallelism regarding management, particularly while performing bone biopsy. Need of the hour is a “Hybrid radiologist,” that is, general radiologist with subspecialty musculoskeletal imaging interest and some training in bone tumor imaging to understand basic imaging features and key principles of biopsy and management of bone tumors. This can be achieved by filling the knowledge gap through change in the training focus to allow a more broad-based learning among general radiology population in India.
Limitations
This study has a limitation of being conducted in a smaller sample size, and number of general and subspecialty radiologists participated in the study were not subcategorized.
References
- Bone tumors in a tertiary care hospital of south India: A review 117 cases. Indian J Med Paediatr Oncol. 2011;32:82.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological data and case load spectrum of patients presenting to bone and soft tissue disease management group at a tertiary cancer center. Indian J Cancer. 2016;53:333.
- [CrossRef] [PubMed] [Google Scholar]
- Staging of bone tumors: A review with illustrative examples. Am J Roentgenol. 2006;186:967-76.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy and clinical utility of biopsy in musculoskeletal lesions: A comparison of fine-needle aspiration, core, and open biopsy techniques. Diagn Cytopathol. 2014;42:476-86.
- [CrossRef] [PubMed] [Google Scholar]
- Computed tomography-guided percutaneous biopsy of bone lesions: Rate of diagnostic success and complications. Radiol Bras. 2014;47:269-74.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic outcome of image-guided percutaneous core needle biopsy of sclerotic bone lesions: A meta-analysis. Am J Roentgenol. 2019;212:625-31.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of primary bone tumors with image-guided percutaneous biopsy: Experience with 110 tumors. Radiology. 2002;223:731-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic work up and recognition of primary bone tumours: A review. EFORT Open Rev. 2016;1:247-53.
- [CrossRef] [PubMed] [Google Scholar]
- Current concepts in the biopsy of musculoskeletal tumors. Sci World J. 2013;2013:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- The training and practice of radiology in India: Current trends. Quant Imaging Med Surg. 2014;4:449-50.
- [Google Scholar]
- Needle biopsy of musculoskeletal lesions. A review of 208 procedures. J Bone Joint Surg Br. 1991;73:498-500.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous core needle biopsy versus open biopsy in diagnostics of bone and soft tissue sarcoma: A retrospective study. Eur J Med Res. 2012;17:29.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomically based guidelines for core needle biopsy of bone tumors: Implications for limb-sparing surgery. Radiographics. 2007;27:189-205. discussion 206
- [CrossRef] [PubMed] [Google Scholar]
- A meta-analysis supports core needle biopsy by radiologists for better histological diagnosis in soft tissue and bone sarcomas. Medicine (Baltimore). 2018;97:e11567.
- [CrossRef] [PubMed] [Google Scholar]
- CIRSE guidelines on percutaneous needle biopsy (PNB) Cardiovasc Intervent Radiol. 2017;40:1501-13.
- [CrossRef] [PubMed] [Google Scholar]
- Image-guided musculoskeletal biopsies. Semin Intervent Radiol. 2010;27:191-8.
- [CrossRef] [PubMed] [Google Scholar]






