Translate this page into:
Botchu-Beale accessory ligament of lateral ankle

*Corresponding author: Rajesh Botchu, Department of Musculoskeletal Radiology, Royal Orthopedic Hospital, Birmingham, England, United Kingdom. drbrajesh@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Hegde G, Penakacherla N, Beale D, Botchu R. Botchu-Beale accessory ligament of lateral ankle. Indian J Musculoskelet Radiol 2023;5:44-6.
Abstract
Variations in anatomy of the tendons and ligaments are not uncommon and cause a diagnostic dilemma. We describe a novel ligament encountered in the ankle extending from posterior inferior tibiofibular ligament to calcaneum. Awareness of normal variant is essential during evaluation of a study.
Keywords
Accessory ligament
Ankle
Lateral
INTRODUCTION
The lateral ligament complex of the ankle is complex and consists of the anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), and calcaneofibular ligament (CFL).[1] The lateral ankle tendons include peroneus brevis and peroneus longus. Peroneus tertius is an accessory muscle that has a variable course. Variations in the anatomy of the tendons and ligament are occasionally encountered resulting in diagnostic dilemmas while interpreting imaging studies. Anatomical variations involving the ankle ligaments are less frequent compared to the tendon. CFL is an important lateral ligament, and a few variations in the anatomy of CFL have been described.[2] This article describes a novel ligament that we encountered on magnetic resonance imaging (MRI) of the ankle, extending from the posterior inferior tibiofibular ligament (PITFL) to the calcaneum.
CASE REPORT
A 65-year-old female presented with insidious onset of hindfoot pain. MRI was performed to evaluate this, which revealed marked talonavicular degenerative change. The ATFL was thickened and edematous in keeping with a grade 2 sprain. CFL was attenuated but intact. The peroneal tendons (peroneus longus and peroneus brevis) were in a normal position without any tendinopathy or tenosynovitis. The superior and inferior peroneal retinaculum was slightly thickened (2 mm) but intact. There was an accessory thick (4 cm × 4 mm) ligament that was posteromedial to the peroneus brevis. This was outside the common peroneal tendon sheath. This accessory ligament (AL) was attached to the fibular origin of the PITFL, coursing posteromedial to the peroneus brevis and attaching to the lateral part of the calcaneum, 6 mm posterior to the peroneal tubercle of the calcaneum [Figures 1-4]. There was no edema in relation to this. Anterior inferior tibiofibular ligament (AITFL) and PITFL were normal and intact without any abnormality. She was managed symptomatically as there was lateral ankle instability.

- Axial Proton density images at different levels showing thickened peroneal retinaculum (small arrow) and accessory ligament (long arrow) (Ref to Figure 1).
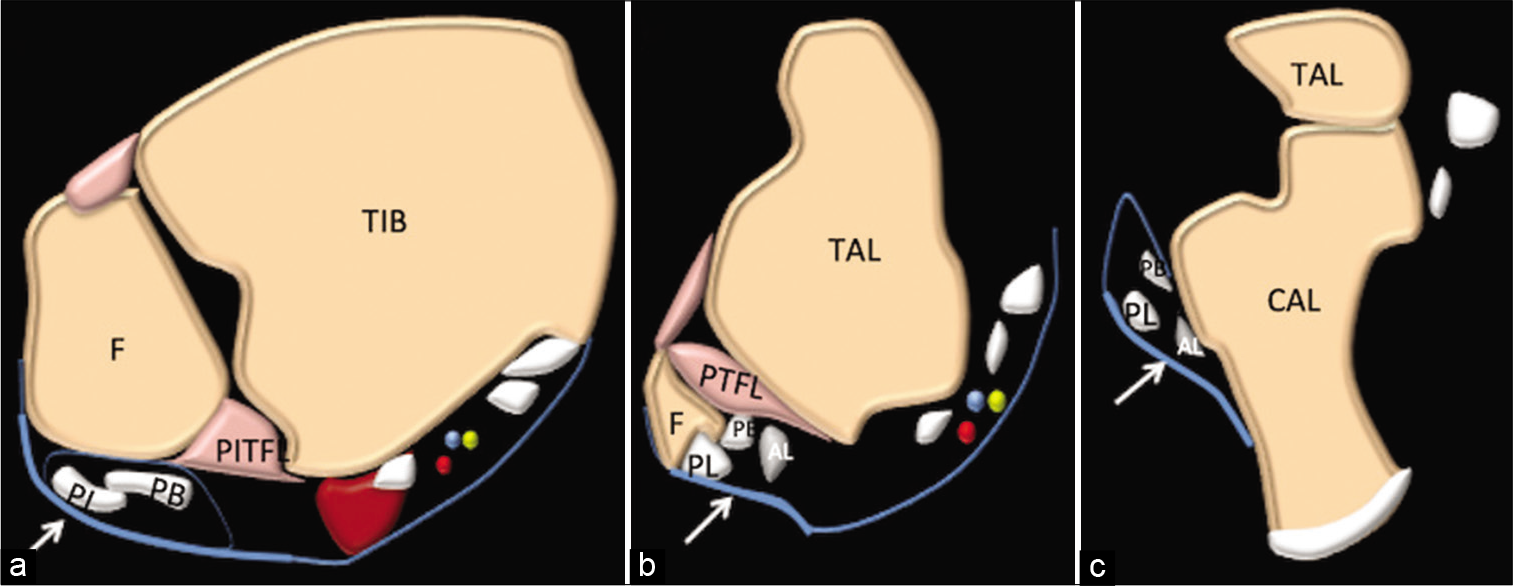
- Axial schematic at different levels showing thickened peroneal retinaculum (small arrow) and accessory ligament (AL). Tibia, fibula, peroneus brevis, peroneus longus (a-c) (Ref to Figure 2).
DISCUSSION
The most common sport injuries involve the ankle with a predilection for the lateral ankle ligaments.[2] The lateral ankle ligaments are complex groups of ligaments that comprise ATFL, CFL, AITFL, PITFL, and PTFL.[3] PITFL is a multifascicular triangular ligament that extends from the posteromedial part of the lateral malleolus to the posterior margin of the distal tibia.[4] This has a superficial and deep component (inferior transverse tibiofibular ligament). No other structure has been described in the literature to arise from this ligament. The morphology of PITFL in our patient was normal. AL arose from the fibular origin of the PITFL.
CFL arises from the anterior aspect of the lateral malleolus coursing inferiorly and attaching to the lateral surface of the calcaneus posterior to the peroneal tubercle. CFL is usually a single structure. The common morphological variants include V and Y shaped CFL where the proximal component has an attachment to the fibula and talus. The lateral talocalcaneal ligament, which is parallel and anterior to CFL, reinforces the CFL in a third of cases. CFL, in our case, was a single band with normal anatomy though slightly attenuated.
Posterior fibulotalocalcaneal (PFTL) ligament is another recently described ligament complex, which comprises inferior fascicles of ATFL, CFL, and connecting arciform fibers and hence located anterior to the CFL.[5] AL differs from the PFTL as it is seen arising from fibular origin of PITFL and located posterior to the CFL.
Peroneus quartus is an accessory muscle with a varied origin (peroneus longus, peroneus brevis, fibula, or any combination of these). PQ has a small muscle belly with tendon coursing along the posterior aspect of the fibula and inserting either into the lateral aspect of calcaneus, talus, cuboid, or fifth metatarsal.[3,6] Peroneus tertius is an accessory muscle that arises from the anterior aspect of the distal fibula (distal third or distal half) and commonly inserts onto the base or shaft of 5th metatarsal or the EDL.[7,8] The location of AL and absence of muscle belly in our case enabled us to prove that this was not an accessory muscle.
Limitations of this report are that we are reporting this AL based on MRI findings and do not have operative confirmation. However, to the best of our knowledge, this entity has not been described in the literature. Awareness of anatomical variations is essential to decrease morbidity. While evaluating MRI of ankle, one needs to analyze all the components of the lateral ankle ligament complex. The usual pattern of injury involves ATFL, CFL, AITFL, PITFL, and PTFL. However, congenital variations with attenuated ligaments can be associated with ALs or abnormal course. This can be an incidental finding as in our case or symptomatic which include pain, instability, and impingement.
CONCLUSION
We describe a new anatomical variant, the AL. One needs to aware of this entity while reporting MR of ankle and evaluating the lateral ligament complex to decrease morbidity.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Anatomy of the ankle ligaments: A pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557-69.
- [CrossRef] [PubMed] [Google Scholar]
- A rare pattern of ligamentous injury of the ankle: A case report and review of the literature. J Foot Ankle Surg. 2021;60:870-2.
- [CrossRef] [PubMed] [Google Scholar]
- The calcaneofibular ligament has distinct anatomic morphological variants: An anatomical cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2020;28:40-7.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated posterior high ankle sprain: A report of three cases. J Orthop Surg (Hong Kong). 2013;21:391-5.
- [CrossRef] [PubMed] [Google Scholar]
- The lateral fibulotalocalcaneal ligament complex: An ankle stabilizing isometric structure. Knee Surg Sports Traumatol Arthrosc. 2020;28:8-17.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneus quartus muscle: MR imaging features. Radiology. 1997;202:745-50.
- [CrossRef] [PubMed] [Google Scholar]
- The accessory peroneal (fibular) muscles: Peroneus quartus and peroneus digiti quinti. A systematic review and meta-analysis. Surg Radiol Anat. 2015;37:617-27.
- [CrossRef] [PubMed] [Google Scholar]
- The fibularis (peroneus) tertius muscle in humans: A meta-analysis of anatomical studies with clinical and evolutionary implications. Biomed Res Int. 2017;2017:6021707.
- [CrossRef] [PubMed] [Google Scholar]


![Coronal PD image showing accessory ligament (arrow). Axial images [Figure 3 and 4] at different levels (a-c).](/content/107/2023/5/1/img/IJMSR-5-044-g001.png)
![Coronal schematic image showing accessory ligament (AL), CF (CFL), PB (peroneus brevis), PL (peroneus longus) and CAL (calcaneum). Axial images [Figures 3 and 4] at different levels (a,b,c).](/content/107/2023/5/1/img/IJMSR-5-044-g002.png)




