Translate this page into:
Demystifying Pandora’s box: A landmark-based approach for gluteal region ultrasound with magnetic resonance imaging correlation

*Corresponding author: Dharmendra Kumar Singh, Department of Radiodiagnosis and Interventional Radiology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. dksinghrad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh U, Nayak BN, Kumar N, Jalan D, Sinha S, Saifi AS, et al. Demystifying Pandora’s box: A landmark-based approach for gluteal region ultrasound with magnetic resonance imaging correlation. Indian J Musculoskelet Radiol. 2024;6:82-7. doi: 10.25259/IJMSR_54_2024
Abstract
The gluteal region is situated at anatomically complex crossroads between the axial and appendicular skeleton and provides pathfinding for many critical neurovascular and myotendinous structures that are essential for synchronous co-ordination between the trunk and lower limbs and dynamic stability during locomotion. While these structures can be evaluated individually using cross-sectional imaging modalities such as magnetic resonance imaging, the extrapolation of the same on grayscale ultrasonography (US) is relatively difficult. Furthermore, the inherently compact arrangement of gluteal anatomy demands protocol-based approach to improve diagnostic efficacy. In this article, a novel approach using five key bony anatomical landmarks is introduced to the readers with the aim of simplifying the approach toward US of gluteal region. Consequently, the use of this staggered approach in patients presenting with deep gluteal pain will not only aid in diagnosis and localization of pathology to respective compartments but shall also serve as a cartograph to plan and perform safe and effective guided interventions.
Keywords
Gluteal pain
Piriformis syndrome
Greater trochanteric pain syndrome
Pudendal nerve entrapment
Hamstring injury
INTRODUCTION
The gluteal region rightfully earns the title of Pandora’s box owing to the inherent complexity of this region by virtue of its location at crossroads of the axial and appendicular skeleton. A large number of anatomical structures (muscles, ligaments, tendons, and neurovascular bundles) crosses this anatomical bridge to connect the axial skeleton to the lower limbs allowing for movement and locomotion.
Clinically, patients with gluteal pathology often present with non-specific deep hip pain which frequently poses a challenge to the clinician in localization of the culprit compartment responsible for pain.[1] While identification of individual components of the gluteal region is made possible on magnetic resonance imaging (MRI), these are difficult to discern on routine grayscale ultrasonography (US). This is further complicated by a lack of contrast resolution on US between similar structures in addition to an absence of a standardized technique for approaching the gluteal region.
This article aims to simplify the imaging approach toward gluteal region ultrasound using five distinct key bony landmarks that can aid in accurate localization of uni/multicompartmental pathology. Furthermore, it is in the authors’ experience that the use of these landmarks to understand locoregional anatomy lays down a strong foundation for performing safe and effective regional ultrasound-guided interventions.
To facilitate maximum retention of this novel concept, the authors would like to draw parallels from a skier going down a hill encountering valleys, thorns, and plateaus in their journey. Following are the key bony landmarks.
Landmark Alpha (Slope) – Bony cortex of Iliac bone
Landmark Beta (Valley) – Greater Sciatic Notch
Landmark Gamma (Thorn) – Ischial spine
Landmark Delta (Medial Plateau) – Ischial tuberosity
Landmark Epsilon (Lateral Plateau) – Greater trochanter (GT).
DISCUSSION
Landmark alpha
Analogy
Akin to a skier beginning their descent along a hill, the obliquely oriented bony cortex of the posterior surface of iliac blade descends infero-laterally from the posterior superior iliac spine to the GT.
Anatomy
This oblique slope provides attachment to the “rotator cuff of hip” composed, from outside in, of the Gluteus maximus (G. maximus), Gluteus medius (G. medius), and Gluteus minimus (G. minimus). These muscles have fibers oriented in different directions which reflect their functional nature (G. medius and G. minimus as abductors at hip joint and G. maximus as an extensor of hip joint) and aid in their identification [Figure 1].[2,3]
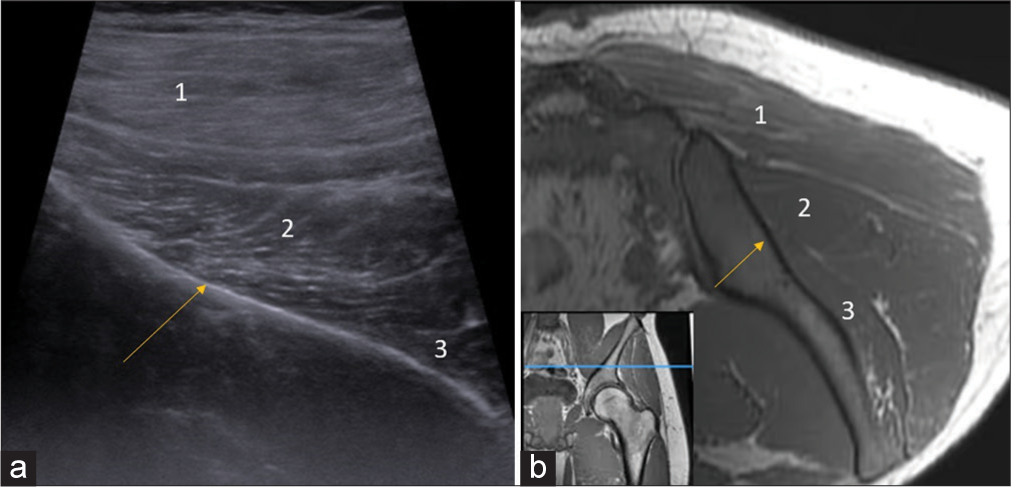
- (a) Ultrasonography (US) image and (b) corresponding T1-weighted (non-fat saturated) axial magnetic resonance imaging (MRI) section flipped 180° at the level of iliac blade (descending slope, arrow) demonstrate the layered arrangement of gluteal muscles (1-Gluteus Maximus, 2-Gluteus medius, 3-Gluteus minimus). Inset at the bottom left corner (b) shows the level of acquisition of both US and MRI section indicated by blue line in T1W coronal image of left gluteal region.
Pathologies
Common pathologies of the gluteal region include cellulitis, abscess (either due to external inoculation, extension from peri-anal fistula, and spread from sacro-iliac joint), or pressure sores.[4]
Landmark beta
Analogy
As the skier descends down the hill, in the route comes a deep valley. Anatomically, this corresponds to the region of the greater sciatic notch which on US is seen as a step-off defect in the bony cortex of ilium.
Anatomy
The greater sciatic notch is the single most important compartment of the gluteal region as it houses the majority of neurovascular bundles that innervate the hip and lower limb [Figure 2].
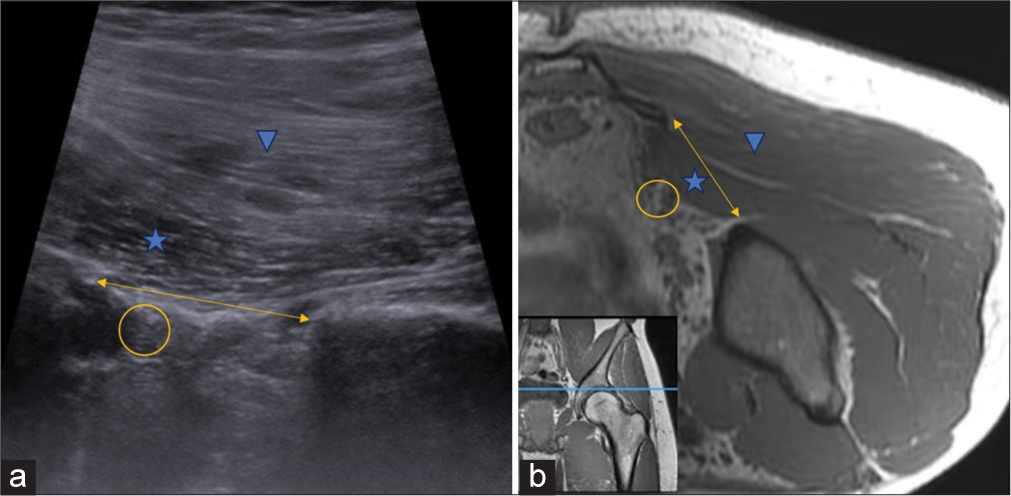
- (a) Ultrasonography (US) image and (b) corresponding T1-weighted (non-fat saturated) axial magnetic resonance imaging (MRI) section flipped 180° at the level of greater sciatic notch (double arrow) demonstrate the dip in iliac blade obliquity representing the notch. The piriformis muscle (asterisk) can be seen traversing horizontally, covered superiorly by the gluteus maximus muscle (arrowhead). The sciatic nerve (oval) can be seen located deep in the piriformis and must be protected during regional interventions. Inset at the bottom left corner (b) shows the level of acquisition of both US and MRI section indicated by blue line in T1W coronal image of left gluteal region.
The key structure of this region is the Piriformis muscle, a pyramid-shaped, relatively flat-oriented muscle that originates from the lateral margin of sacrum, courses just inferior to the inferior border of G. medius muscle, and inserts onto the superior tip of GT in close proximity to G. medius and G. minimus tendons.
This implies that while visualizing the Piriformis muscle in long axis, no other muscle will be seen in the sectional image except for the G. maximus muscle which forms the roof of the subgluteal space. Piriformis plays a vital role in maintaining postural stability during static (standing) and dynamic (walking) activities and divides the greater sciatic notch into a supra-piriformis and infra-piriformis compartments.[5]
The supra-piriformis compartment contains the superior gluteal neurovascular bundle supplying the G. medius and G. minimus.
The infra-piriformis compartment houses chiefly the inferior gluteal neurovascular bundle, sciatic nerve (located just deep to piriformis), and the pudendal nerve.[6]
Pathologies
Piriformis syndrome is the most common pathology at this landmark and refers to sciatic nerve entrapment secondary to hypertrophied piriformis muscle with altered echopattern and vascularity, presenting as an elusive cause of nondiscogenic/extraspinal cause of gluteal pain and/or sciatica. Diagnosis is often suggested by an asymmetry in size of muscle (compared to contralateral side) and other ancillary features such as increased hypoechogenicity and vascularity within the muscle.[7]
Superior gluteal nerve damage often manifests as weakness in the abduction of hip with a limping gait and occurs iatrogenically following total hip arthroplasty or following ilio-sacral screw placement. Similarly, inferior gluteal nerve damage is a known complication of posterior approach to hip arthroplasty and is often diagnosed secondary to signal alterations in G. maximus on MRI sections.[8]
Landmark gamma
Analogy
Just after crossing the valley, the skier encounters a solid thorn angled toward them in their course. This is represented by the ischial spine which serves as the third important landmark of this region.
Anatomy
The bony ischial spine serves as an anchor for the attachment of sacrospinous ligament, separating the superiorly located greater sciatic foramen from the inferiorly located lesser sciatic foramen. Furthermore, this thorn-like bony projection segregates the sciatic nerve (located superficial and lateral to the ischial spine) from the pudendal nerve (located deep and medial to the ischial spine) [Figure 3].
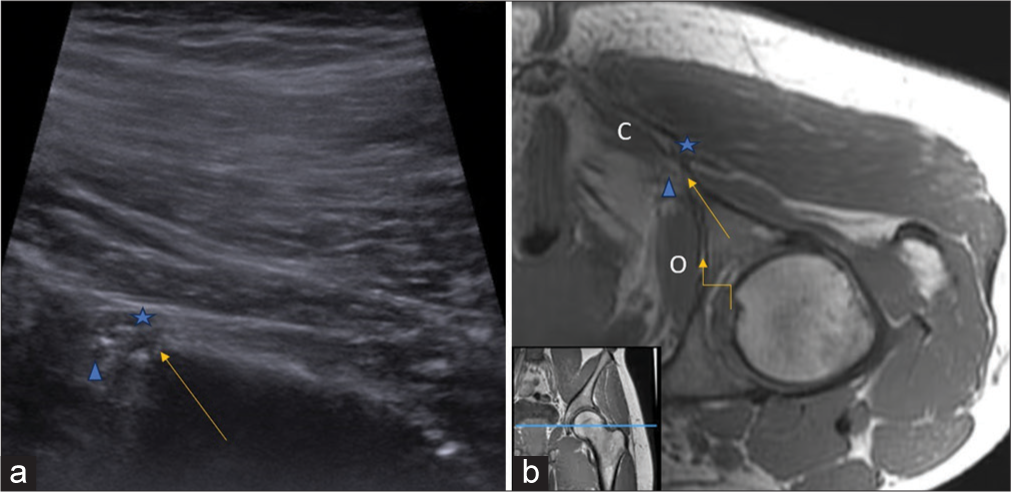
- (a) Ultrasonography (US) image and (b) corresponding T1-weighted (non-fat saturated) axial magnetic resonance imaging (MRI) section flipped 180° at the level of ischial spine (arrow) show the sciatic nerve (asterisk) and pudendal nerve (arrowhead) located superficial and deep to ischial spine, respectively. The pudendal nerve courses between the “Lobster’s claw” limited by obturator internus (O) laterally and coccygeus muscle (C) medially into the Alcock’s canal (curved arrow). Inset at the bottom left corner (b) shows the level of acquisition of both US and MRI section indicated by blue line in T1W coronal image of left gluteal region.
From this point, the pudendal nerve courses anteriorly, along the medial surface of ischial spine between the sacrospinous and sacrotuberous ligaments, into the Alcock’s canal. This unique anatomical arrangement is referred to as “Lobster’s claw” predisposing the nerve to impingement.[9]
Pathologies
Understanding of this anatomical arrangement is of paramount importance in approaching patients with deep pelvic pain who are suspected to have pudendal neuralgia and require targeted intervention for its management.[10]
Pudendal nerve entrapment syndrome[11] is subdivided into four distinct subtypes on the basis of site of suspected impingement, as follows:
Type 1: Below piriformis muscle after exit from greater sciatic notch
Type 2: Most common between sacrospinous and sacrotuberous ligaments
Type 3: At Alcock’s canal
Type 4: Impingement of terminal branches.
Landmark delta
Analogy
For the penultimate stop, the skier stumbles upon a plateau formed by a bony projection at the inferior – most part of the pelvis – the ischial tuberosity.
Anatomy
The medial plateau (ischial tuberosity) with its two facets (infero-medial and supero-lateral) provides attachment for powerful hip extensors and knee flexors, namely the hamstring group of muscles. The flattened and crescent-shaped lateral facet serves as an attachment site for semimembranosus tendon. This tendon also has an accessory anterior expansion along the inferior ischium that blends with the ischio-condylar part of adductor magnus – which earns its label as “mini hamstring.”[12,13]
The medial facet provides attachment to the conjoint tendon of biceps femoris and semitendinosus with reinforcements from the sacro-tuberous ligament descending inferolateral from the sacrum [Figure 4].[14]
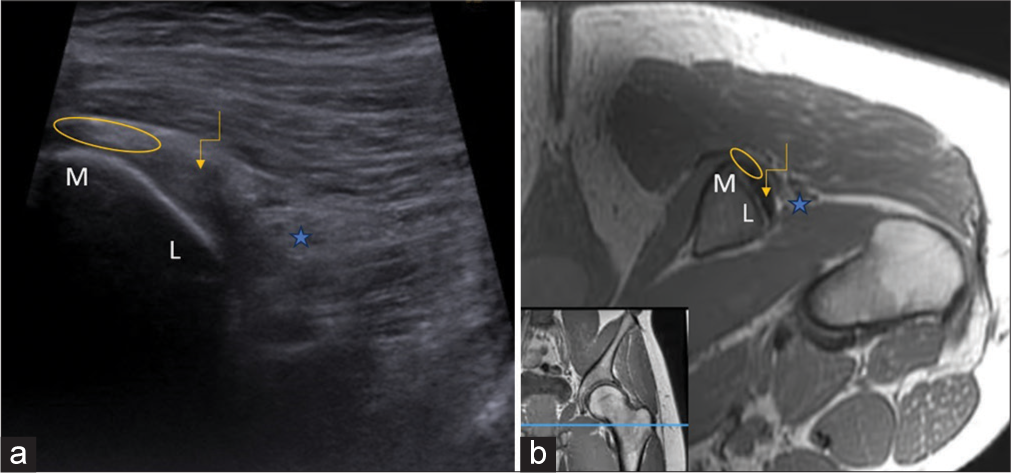
- (a) Ultrasonography (US) image and (b) corresponding T1-weighted (non-fat saturated) axial magnetic resonance imaging (MRI) section flipped 180° at the level of ischial tuberosity with its two facets, medial (M) and lateral (L) along with the attachment of conjoint tendon (ellipse) medially and semimembranosus (curved arrow) superolaterally. The sciatic nerve (asterisk) is seen immediately adjacent to semimembranosus attachment. Inset at the bottom left corner (b) shows the level of acquisition of both US and MRI section indicated by blue line in T1W coronal image of left gluteal region.
Of note, the sciatic nerve lies just lateral to the semimembranosus attachment as it descends infero-laterally from the ischial spine.
Pathologies
The ischial tuberosity apophysis can undergo avulsion fracture secondary to a violent force at the hip in a skeletally immature patient. Lower-grade repetitive injury may be devoid of avulsion and instead present as apophysitis resulting in marrow edema without any obvious separation of the apophysis from its attachment.[15]
Contrarily, in adults, hamstring injuries often manifest as either tendinosis or tear with progressive tendon degeneration often leading to longitudinal interstitial tendon splits.[16]
Adductor myotendinous strains occur predominantly in athletes and must be differentiated from adductor avulsions as both are treating differently with conservative and surgical management, respectively.[16]
Landmark epsilon
Analogy
As the skier comes to an end of their journey, they encounter a final obstacle in their path, a lateral plateau, represented by the GT of femur.
Anatomy
The GT of femur and the ischial tuberosity of pelvis are located at the same anatomical level and are bridged by a strong transversely oriented muscle the quadratus femoris [Figure 5]. This strong external rotator and adductor of the hip originates from the ischial tuberosity anterior to the origin of hamstring tendons and inserts onto the quadrate tubercle of posterior intertrochanteric ridge of femur. This muscle forms the bed for sciatic nerve to descending posteriorly into the thigh.[17]
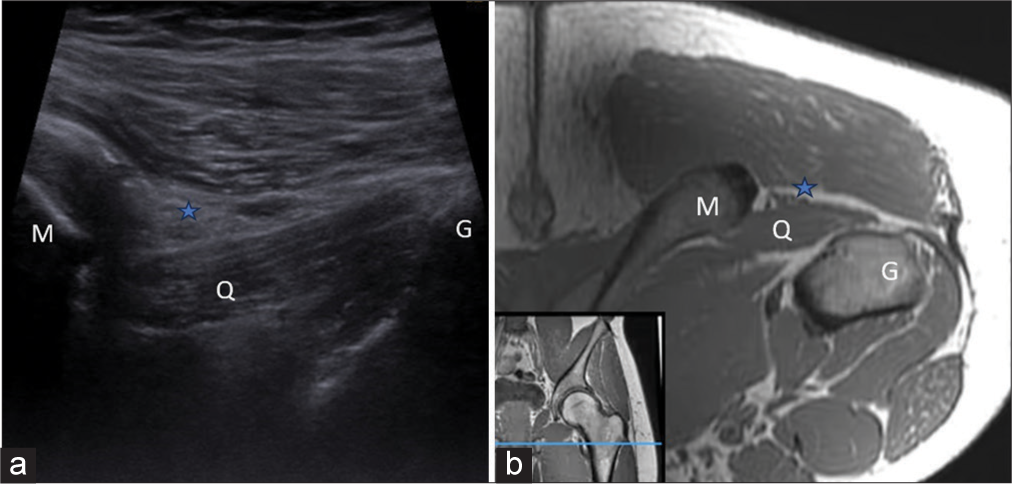
- (a) Ultrasonography (US) image and (b) corresponding T1-weighted (non-fat saturated) axial magnetic resonance imaging (MRI) section flipped 180° at the level of greater trochanter lateral plateau (G) shows quadratus femoris muscle (Q) bridging the two plateaus (medial plateau, M and lateral plateau, G) and forming the bed for sciatic nerve (asterisk) to pass into the thigh. These two landmarks also serve to identify the dimensions of ischio-femoral/quadratus femoris space to evaluated ischiofemoral impingement. The greater trochanter (G) is also a frequent site of injury in many patients with greater trochanteric pain syndrome. Inset at the bottom left corner (b) shows the level of acquisition of both US and MRI section indicated by blue line in T1W coronal image of left gluteal region.
Two important spaces form the critical limit of this landmark: The Ischio-femoral space (symptomatic when <17 mm) and the Quadratus femoris space (symptomatic when <8 mm). Knowledge of their anatomy is a pre-requisite for managing ischio-femoral impingement and atypical groin pain.[18]
The bony surface of the GT consists of four facets: Anterior, lateral, posterior, and posterosuperior. The G. medius muscle attaches to the posterosuperior and lateral facets. The G. minimus muscle attaches to the anterior facet [Figure 6]. The trochanteric bursa covers the posterior facet and the lateral insertion of the G. medius muscle beneath G. maximus muscle and iliotibial band. The sub G. medius bursa is located in the superior part of the lateral facet, underneath the G. medius tendon. The sub G. minimus bursa lies in the area of the anterior facet, underneath the G. minimus tendon, medial and cranial to its insertion, and extends medially covering the distal anterior part of the hip joint capsule.[19,20]
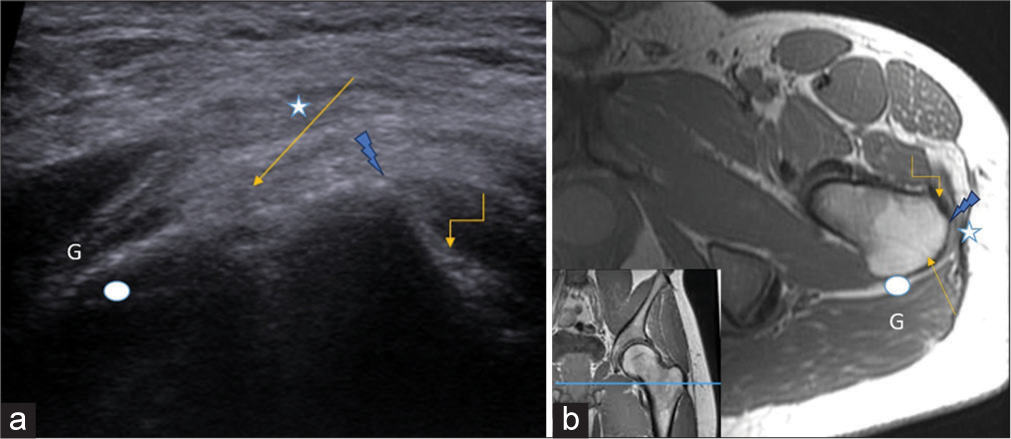
- (a) Axial ultrasound image and (b) corresponding T1-weighted axial non-fat saturated image demonstrate the anatomy of greater trochanter. The anterior facet harbors Gluteus minimus tendon insertion (curved arrow), the flattened lateral facet serves as an attachment for Gluteus medius (straight arrow), and the beginning of posterior facet (white oval) covered by Gluteus maximus (G. maximus) muscle (G). Iliotibial band (asterisk) is seen extending between G. maximus muscle and tensor fascia lata. The pyramidal-shaped bony projection between anterior and lateral facets is clearly seen (lightening arrow). Inset in (b) shows the level of acquisition of both US and MRI section indicated by blue line in T1W coronal image of left gluteal region.
Pathologies
Quadratus femoris pathologies often include sprains that occur in athletes and manifest as altered fiber orientation and/or muscle edema at myotendinous junction.[17]
In cases of ischio-femoral impingement syndrome, anatomical narrowing between the two bony barriers (ischium and femur) may predispose to muscle injury and sciatic nerve impingement manifesting as edema at the site of maximum impingement.[18]
Clinically presenting lateral hip pain can occur secondary to varying combinations of insertional enthesopathy, tendon tears, bursitis, and calcific tendinitis at the GT and these pathologies are responsible for the syndrome known as “Greater Trochanter Pain Syndrome.”[19,20]
CONCLUSION
The gluteal region is a complex, multi-compartmental bridge between the axial and appendicular skeleton and serves as an important crossroads for many critical structures responsible for mobility and stability. While MRI provides higher contrast resolution and confers the ability to discern each structure separately, the same cannot be reciprocated by US due to its operator-dependent nature. Furthermore, interventional management for gluteal pathologies is predominantly US based. Hence, the landmark approach provides details into the intricate anatomy of the gluteal region and offers the benefit of improved diagnostic efficacy which ultimately translates into improved interventional outcome.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- MR imaging of the hip abductors: Normal anatomy and commonly encountered pathology at the greater trochanter. Magn Reson Imaging Clin N Am. 2005;13:691-704, vii
- [CrossRef] [PubMed] [Google Scholar]
- Injury of the gluteal aponeurotic fascia and proximal iliotibial band: Anatomy, pathologic conditions, and MR imaging. Radiographics. 2013;33:1437-52.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic examination of the buttock. J Clin Ultrasound. 2013;41:546-55.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically relevant bony and soft tissue anatomy of the proximal femur. Orthop J Sports Med. 2014;2:2325967114535188.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of piriformis syndrome: A rare anatomic variant analyzed by magnetic resonance imaging. J Clin Imaging Sci. 2018;8:6.
- [CrossRef] [PubMed] [Google Scholar]
- Use of diagnostic musculoskeletal ultrasound in the evaluation of piriformis syndrome: A review for rehabilitation providers. Int J Sports Phys Ther. 2024;19:768-72.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of entrapment neuropathies of the lower extremity. Radiographics. 2010;30:983-1000.
- [CrossRef] [PubMed] [Google Scholar]
- La prise en charge moderne des névralgies pudendales. A partir d'une série de 212 patientes et 104 interventions de décompression [Modern algorithm for treating pudendal neuralgia: 212 cases and 104 decompressions] J Gynecol Obstet Biol Reprod (Paris). 2003;32:705-12.
- [Google Scholar]
- High-resolution ultrasound of the pudendal nerve: normal anatomy. Muscle Nerve. 2013;47:403-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pudendal nerve entrapment syndrome In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024.
- [Google Scholar]
- A qualitative and quantitative analysis of the attachment sites of the proximal hamstrings. Knee Surg Sports Traumatol Arthrosc. 2015;23:2554-61.
- [CrossRef] [PubMed] [Google Scholar]
- The adductor magnus “mini-hamstring”: MRI appearance and potential pitfalls. Skeletal Radiol. 2016;45:213-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical study of the proximal origin of hamstring muscles. J Orthop Sci. 2012;17:614-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring injuries of the hip. Magn Reson Imaging Clin N Am. 2005;13:677-90, vi
- [CrossRef] [PubMed] [Google Scholar]
- Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90:2365-74.
- [CrossRef] [PubMed] [Google Scholar]
- Quadratus femoris tendinitis as a cause of groin pain. Br J Sports Med. 1997;31:348-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ischiofemoral impingement syndrome: An entity with hip pain and abnormalities of the quadratus femoris muscle. AJR Am J Roentgenol. 2009;193:186-90.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodality imaging of greater trochanter lesions. Pol J Radiol. 2021;86:e401-14.
- [CrossRef] [PubMed] [Google Scholar]
- Greater trochanter of the hip: Attachment of the abductor mechanism and a complex of three bursae--MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221:469-77.
- [CrossRef] [PubMed] [Google Scholar]







