Translate this page into:
Distal femoral physeal fracture-dislocation (Salter-Harris-I) in a newborn: A case report

*Corresponding author: Riya Samanta, Department of Radiology, Mahajan Imaging, Safdarjung Hospital Sports Injury Centre, New Delhi, India. samanta.ria1011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Samanta R, Batta NS, Abhinetri KS, Gupta V. Distal femoral physeal fracture-dislocation (Salter-Harris-I) in a newborn: A case report. Indian J Musculoskelet Radiol. 2024;6:120-4. doi: 10.25259/IJMSR_11_2024
Abstract
Physeal fractures in newborns are relative rare injuries, most often occurring as a result of birth trauma. Salter-Harris fractures of the distal femur should be treated as knee dislocation and, hence, as a medical emergency. A high index of suspicion for vascular injury should be present. Reduction, stabilization, and, if necessary, vascular repair should be carried out at the earliest to avoid permanent damage/deformity. We report a case of distal femoral physeal fracture and dislocation in a 2-day old neonate presenting with a swollen knee and decreased motion of the right lower extremity shortly after delivery.
Keywords
Distal femur
Fracture
Salter-Harris
Physeal injuries
Newborn
INTRODUCTION
The distal femoral growth plate or the physis is responsible for the majority of the growth of the femur. Most periarticular injuries in the pediatric population involve the growth plates since the physes are the weaker link in the pediatric joints, as compared to the ligaments.[1]
The distal femoral physeal injuries are associated with a high incidence of long-term complications such as growth disturbances, with eventual leg length discrepancy and/or deformities. The potential for development of complications is related to the child’s age at the time of trauma.[1] Therefore, these injuries should be treated as emergencies, and prompt surgical management should be instituted to prevent the onset of complications such as permanent damage/deformity. Imaging modalities such as X-ray, ultrasonography (USG), computed tomography, and magnetic resonance imaging (MRI) aid to accurately diagnosing and characterize these injuries in the newborn.
Salter-Harris classification
The Salter-Harris classification[2] [Figure 1 and Table 1] has described five types of physeal injuries. Studies have shown that displaced fractures have a significantly higher growth disturbance rate than undisplaced fractures.[3]
| Sr. No. | Type | Description |
|---|---|---|
| 1. | Salter–Harris I | Fracture plane passes through the growth plate/physis |
| 2. | Salter–Harris II | Fracture plane courses through the growth plate/physis and exits through the metaphysis |
| 3. | Salter–Harris III | Fracture plane courses through the growth plate/physis and exits through the epiphysis. |
| 4. | Salter–Harris IV | Fracture extends from the metaphysis -growth plate/physis and down to the epiphysis. |
| 5. | Salter–Harris V | Compression and damage to the growth plate/physis secondary to a crush injury. |
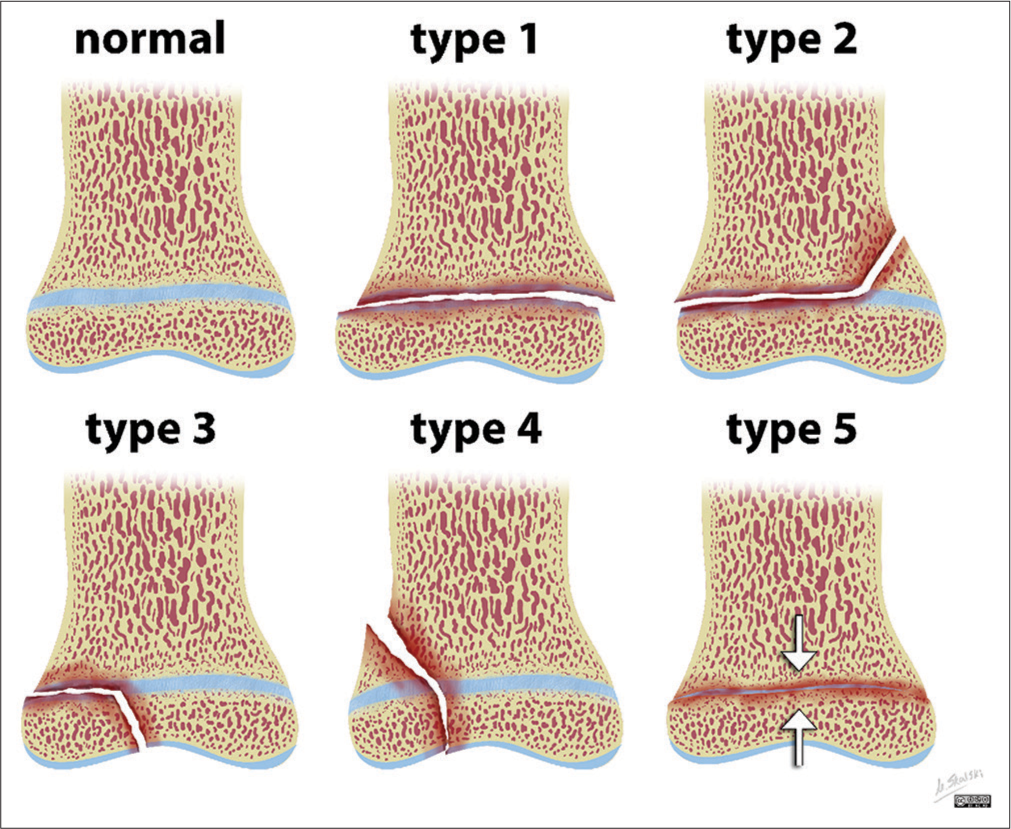
- Illustration of Salter-Harris classification for physeal injuries. Case courtesy of Matt Skalski, Radiopaedia.org, rID: 27144.
CASE REPORT
A 2-day-old neonate presented with a swollen knee and decreased motion of the right lower extremity shortly after a difficult vaginal breech delivery which involved forced traction of the limb. The prenatal course was unremarkable, and the child was born at term. At the presentation, the child was afebrile. Clinical examination revealed warmth and tenderness at the right knee joint. The range of motion was restricted at the knee joint but normal at the hip joint. The popliteal and distal pulses were palpable. There was no evident neurological deficit.
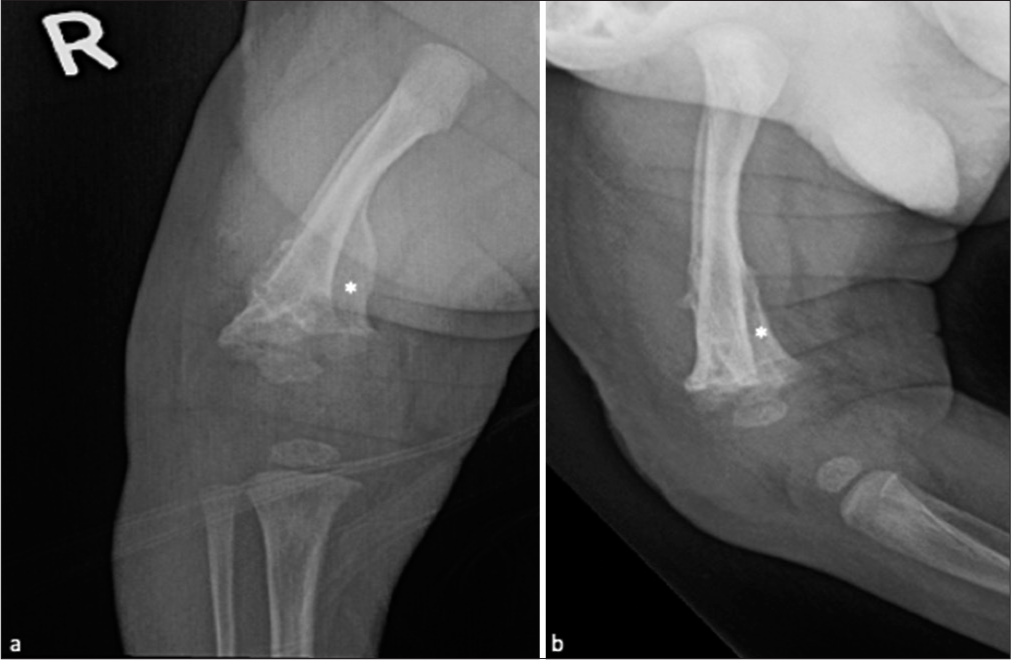
Frontal and lateral radiographs of the right knee [Figure 2] revealed a loss of congruence between the distal femoral epiphysis and metaphysis, and hence, a Salter-Harris type I injury was inferred. As the femoral epiphyseal ossification center was very small, it was difficult to determine if the normal anatomical relationship between the distal femoral epiphysis and the tibia was maintained or not. Commenting on absence of a definite epiphyseal injury was also difficult.
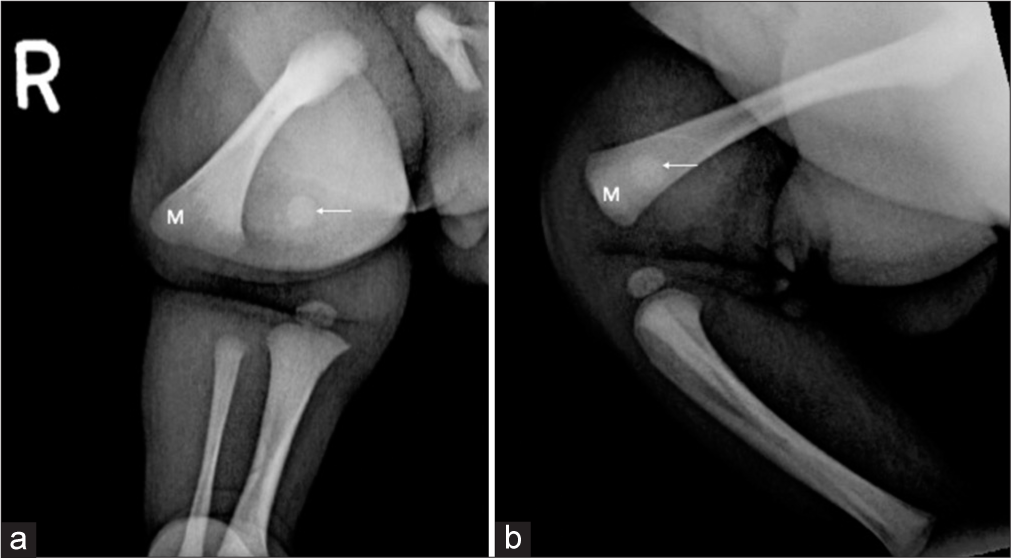
- Two-day-old neonate with Salter-Harris I fracture of the distal right femur. (a) Frontal and (b) lateral radiographs of the right knee revealed loss of congruence between the distal femoral epiphysis (arrow) and metaphysis (M).
Subsequently, MRI of the distal thigh and knee was performed [Figure 3]. MRI revealed a distal femoral physeal fracture (Salter-Harris-I) with lateral dislocation of the femoral metaphysis relative to the epiphysis. The dislocated metaphyseal end of the distal femur was seen to be projecting into the subcutaneous fat resulting in a focal bulge of the overlying skin. The distal femoral epiphysis (cartilaginous femoral condyles) was in congruence with the proximal tibia with preserved knee joint space. No significant joint effusion was noted. Marked surrounding soft-tissue/intramuscular hemorrhage and edema – predominantly in the vastus lateralis and intermedius were noted. Visualized vascular flow voids were relatively preserved.
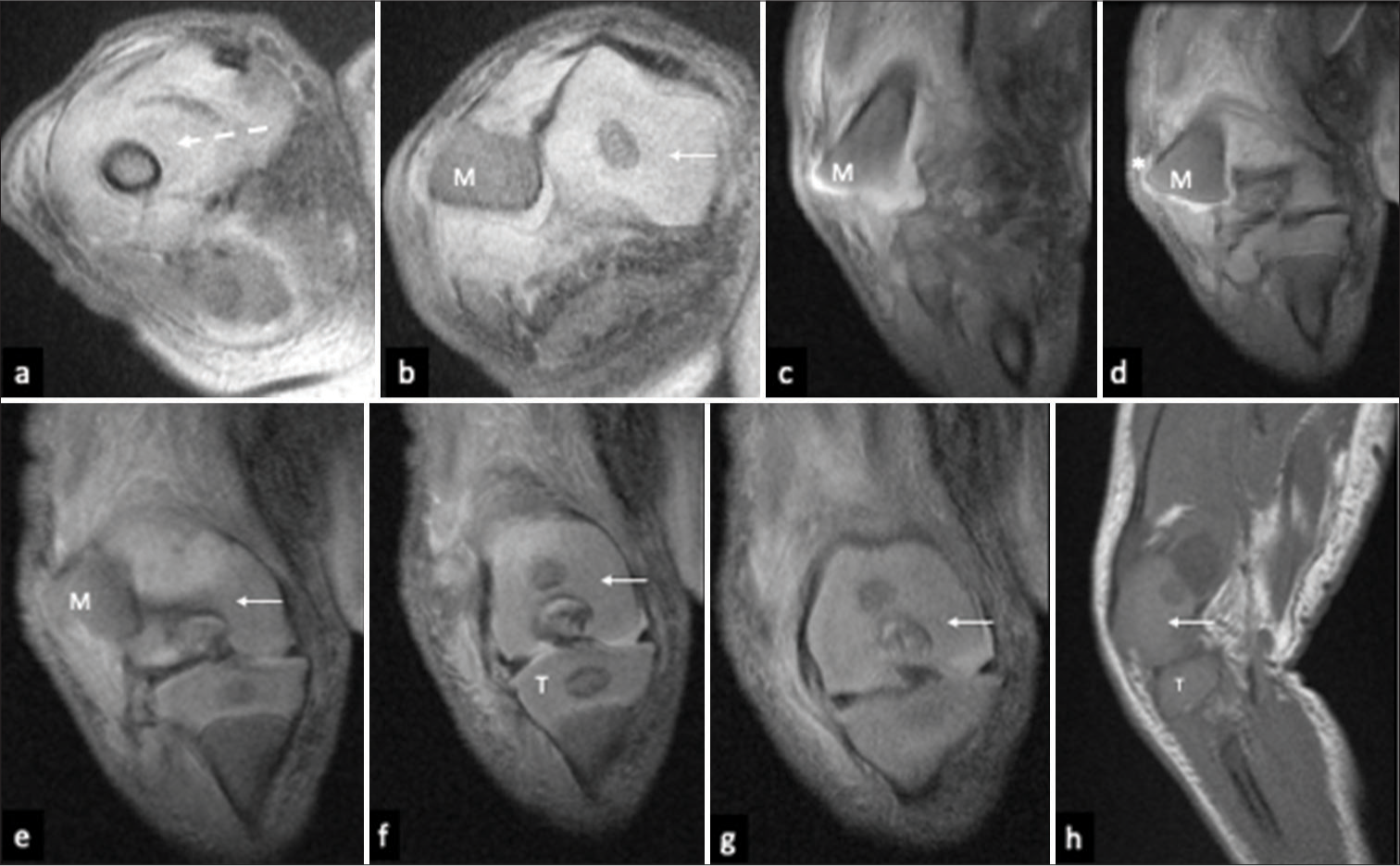
- Magnetic Resonance Imaging (MRI) of the right knee revealed distal femoral physeal fracture (Salter-Harris-I) with lateral dislocation of the femoral metaphysis (M). (a and b), Axial PDFS, (c-g) coronal PDFS and (h) sagittal T1-weighted MR images revealed marked soft tissue/muscle edema in the anterior thigh distally (dashed arrow), projection of the dislocated metaphyseal end of the distal femur into the subcutaneous fat (asterisk), causing a focal bulge in the overlying skin and preserved congruence of distal femoral epiphysis (cartilaginous femoral condyles) (arrow) with the proximal tibia (T).
The child was subsequently taken to orthopedic surgery for open reduction and pinning of the distal femoral fracture. The distal femoral physeal fracture was successfully reduced anatomically and fixated with two laterally placed pins.
Follow-up radiograph was performed a month after surgery [Figure 4] which revealed anatomic alignment of the femur following reduction and pinning. Extensive periosteal reaction and new bone formation were noted in the distal femur. Pin removal was done after 2 days of the postoperative radiograph.
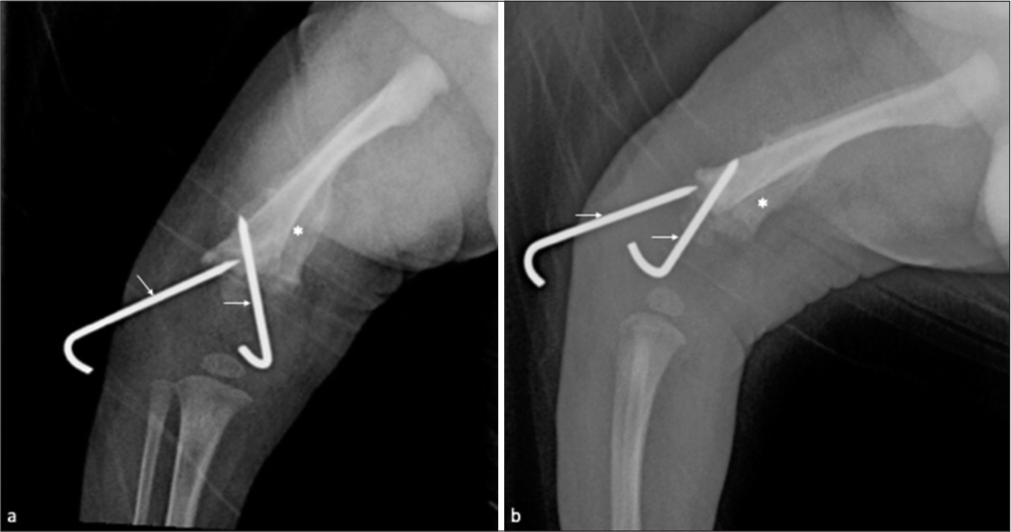
- (a) Frontal and (b) lateral follow-up radiographs, a month later, revealed anatomic alignment of the femur following reduction and pinning (arrow). There was extensive periosteal reaction and new bone formation (asterisk) in the distal femur.
A radiograph was obtained a week following pin removal, which revealed normal alignment of the bones [Figure 5] and extensive distal femoral periosteal reaction. Another radiograph was obtained around 1 year later, which revealed normal outline and alignment of the bones [Figure 6] without any deformity.
- (a) Frontal and (b) lateral radiographs obtained after a week following pin removal revealed normal alignment of the bones with extensive periosteal reaction (asterisk) in the distal femur.
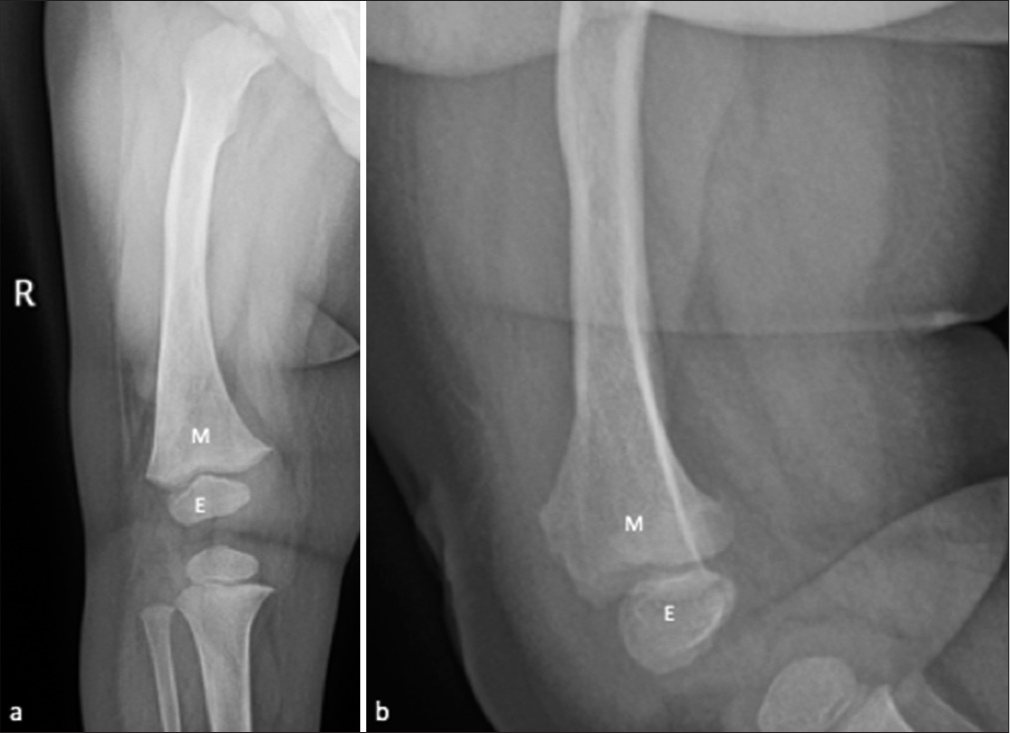
- (a) Frontal and (b) lateral radiographs obtained a year later - revealed normal outline and alignment of the bones, that is, the distal femoral metaphysis (M) and epiphysis (E) without any deformity.
DISCUSSION
Fracture-separation of the distal femoral epiphysis is a relatively uncommon injury in neonates but is known to occur as a complication of difficult vaginal delivery, particularly in cases of breech presentation.[4] Physeal fracture of the distal femur in a newborn with complete distraction has rarely been reported in literature.
Salter-Harris-type I injury is when the fracture plane courses through the growth plate, resulting in separation between the metaphysis and epiphysis and leading to an increased width of the physis/growth plate.
Physeal fractures in newborns can often be misdiagnosed as dislocations or osteomyelitis/septic arthritis due to limb swelling and tenderness [Table 2].[5] As the aforementioned conditions are uncommon at birth, a diagnosis of Salter-Harris type I fracture should be strongly considered. The distal femoral epiphyseal ossification takes place at about 38 weeks of gestation. Plain radiographs are primarily used for evaluating these physeal fractures after 38 weeks of gestation and typically show physeal widening with metaphysealepiphyseal dislocation.[4] However, a radiographic diagnosis may be challenging in preterm neonates as the epiphyseal ossification center is non-ossified and, hence, not visible yet. In such cases, USG may be helpful in providing a detailed image of the cartilaginous epiphysis and periosteal reaction associated with the fracture.[4] USG has previously been reported to be helpful in the detection of neonatal physeal injuries/fractures at the proximal and distal humerus as well as proximal femur and is comparable in accuracy to MRI, although operator dependent.[5]
| Sr. No. | Differential Diagnosis | Differentiating features |
|---|---|---|
| 1. | Osteomyelitis | Soft tissue swelling/edema/abscess Bone marrow edema Regional osteopenia Periosteal reaction Focal osteolysis/cortical loss/loss of trabecular bony architecture |
| 2. | Septic arthritis | Fever Locoregional redness and increased temperature Imaging: early: Normal bony alignment, juxta-articular osteopenia, joint effusion with/without debris and joint capsular edema. Late: Loss of joint space, cartilage and bone destruction and eventually, ankylosis. |
| 3. | Knee dislocation | Loss of alignment between femur and tibia. Preserved femoral epi-metaphyseal alignment |
MRI is a helpful imaging modality in accurately diagnosing physeal injuries and has the benefit of being radiation free.[6] The other advantages of MRI include better definition of the fracture extent and the degree of dislocation/distraction, identification of occult fractures, and demonstration of other associated injuries such as ligamentous lesions. However, it may be challenging to assess critically ill patients, and sedation may be required to acquire images of good quality.
Reduction and fixation/pinning are the management of choice in Salter-Harris-I injuries. Follow-up radiographs can confirm the restitution of alignment and aid assessment of bone healing as evidenced by the presence of periosteal reaction as well as new bone formation at the site of trauma.[7] Despite adequate treatment, a possibility of poor surgical outcome and debilitating sequelae exists; complications include permanent restriction of range of motion, angular deformity, arrested growth, and subsequent limb length discrepancy.[8] Therefore, a proper evaluation with serial radiographs is always suggested during follow-up.
CONCLUSION
Any child presenting with a tender and swollen limb in the first few days of life should be evaluated with the available imaging to rule out a possibility of physeal injury and should be differentiated from its mimics by means of appropriate clinical and radiological examinations. Despite its rarity and diagnostic dilemma, Salter-Harris-I physeal injury in newborns has good outcomes, with osseous remodeling and early recovery abetted by prompt as well as accurate diagnosis in conjunction with appropriate orthopedic surgical management.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Salter Harris fractures of the distal femur: Learning points from two cases compared. J Investig Med High Impact Case Rep. 2013;1:2324709613500238.
- [CrossRef] [PubMed] [Google Scholar]
- Injuries involving the epiphyseal plate. J Bone Joint Surg. 1963;45:587-662.
- [CrossRef] [Google Scholar]
- Fracture-separation of the distal femoral epiphysis in a premature neonate. J Ultrasound Med. 2006;25:1603-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture of lower femoral epiphysis in an infant at birth: A rare obstetrical injury. J Perinatol. 2001;21:550-2.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging in acute physeal injuries. Skeletal Radiol. 1994;23:627-31.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting the outcome of physeal fractures of the distal femur. J Pediatr Orthop. 2007;27:703-8.
- [CrossRef] [PubMed] [Google Scholar]







