Translate this page into:
Estimation of the reference value of pubofemoral distance in normal infants by ultrasonography: A pilot study in Indian population

*Corresponding author: Siddhi Chawla, Department of Radiology, Sardar Patel Medical College, Bikaner, Rajasthan, India. siddhi.chawla870@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chawla S, Meena G. Estimation of the reference value of pubofemoral distance in normal infants by ultrasonography: A pilot study in Indian population. Indian J Musculoskelet Radiol. 2023;5:106-12. doi: 10.25259/IJMSR_9_2023
Abstract
Objectives:
The objectives of this study were to determine the normal values of pubofemoral distance (PFD) and its variation with age, sex, and laterality of hip in infants in the Indian population.
Material and Methods:
The PFD was measured in 141 infants falling under Grafs categories I, IIa, and IIb (Males: 77 and Females: 64) divided into two groups comprising the neonatal group (<1 month) and postneonatal group (>1–12 months). PFD measurement and Grafs’ method of alpha- and beta-angle measurement were both performed at the same time by doing an ultrasound of the hip. Probe was placed in the coronal plane in lateral decubitus with the flexed position in a neutral position. PFD was measured between the superior pubic rami and femoral head epiphyses.
Results:
The average PFD in 141 infants (282 hips) was 3.23 ± 0.83 mm. It was 3.15 ± 0.79 mm in the neonatal group (88 patients) and 3.47 ± 0.84 mm in the postneonatal group (53 patients). In males, the average PFD was 3.29 ± 0.85 mm, and in females, it was 3.23 ± 0.81 mm. No significant difference was observed in the average PFD among the two sexes and between the left and right hips of both neonatal and postneonatal groups.
Conclusion:
The study demonstrates reference PFD values in infants aged 0–12 months in neonatal and postneonatal age groups. Mean PFD values were not significantly influenced by the laterality or sex of the patient in both groups, however, increased with age. Further studies need to be done however to find its values in the cases with developmental dysplasia of the hip to determine the cutoff in such cases.
Keywords
Hip ultrasonography
Screening ultrasound
Developmental dysplasia of the hip
Pubofemoral distance
INTRODUCTION
Developmental dysplasia of the hip (DDH) encompasses a spectrum of abnormalities ranging from a stable hip having a mildly dysplastic acetabulum (AB) to a complete hip dislocation. This condition is a major health concern, affecting 6–20 children/1000.[1-3] Early diagnosis of the disease is based on clinical or radiological criteria. Delay in diagnosis and treatment might result in complications such as premature degenerative joint disease, functional impairments, chronic pain, and permanent disability. Using only physical examination, 50% of infants with dislocated hip joints are diagnosed by the end of their 1st year of life.[4]
Graf and Schuler[5] and Harcke and Grissom[6] proposed a dynamic ultrasound technique to assess hip instability. Studies have shown that the rates of open reductions and complications decreased when ultrasonography (USG) was used as a screening tool for hip dysplasia.[7-9] US is the preferred imaging method for diagnosis of DDH if screening is done for patients aged <4 months.[10,11] One major limitation of USG is that it is operator dependent and the technique used for hip examination can be complex and difficult to learn. At present, a combination of the static technique proposed by Graf and the dynamic technique proposed by Harcke is used.[10,12]
In 2012, study by Treguier et al.[1] for the 1st time emphasized that the US screening technique given by Couture et al.[13] to measure pubofemoral distance (PFD) is much simpler and reproducible. The authors concluded that PFD measurement with a threshold for abnormality of 6 mm at the age of 1 month, without asymmetry above 1.5 mm is suggestive of DDH. Multiple studies have been subsequently done to evaluate mean values of PFD in different countries and its comparison with the Grafs method in the early detection of DDH. There is no Indian study to date to determine the normal value of PFD and cutoff for a diagnosis of DDH.
The primary objective of the present study was to evaluate the normal PFD in children <12 months in the Indian population. The establishment of normal values is useful to conduct future studies in patients with DDH.
MATERIAL AND METHODS
The study was approved by the Ethics Committee of our institution. It was carried out from February 2022 to June 2022. Infants who were referred to the radiology department by various clinical departments for any indication requiring ultrasound were included in the study. Those children who were referred for orthopedic problems or had a clinical query/ diagnosis of DDH based on any clinical/imaging evaluation were excluded from the study. Children were divided into two groups based on their age neonatal (Age <1 month) and postneonatal (Age >1–12 months). Alpha- and beta-angles were measured initially in all, according to the technique proposed by Graf[4] to confirm that there was no dysplasia. The bony rim percentage (BRP) measurement was determined by the technique given by Teixeira et al.[14] The hips of the patients having normal values of BRP and placed in Graf ’s categories I and IIa classification were included in the study for measurement of PFD4. Graf IIC, III, D, and IV were not included as they were considered dysplastic. Graf IIB was not considered because this classification is defined after 12-week follow-up examinations for immature hips[14] [Figures 1-3].

- Graf classification I with normal bony rim percentage and pubofemoral distance (between cursors) in 10-day-old infant.
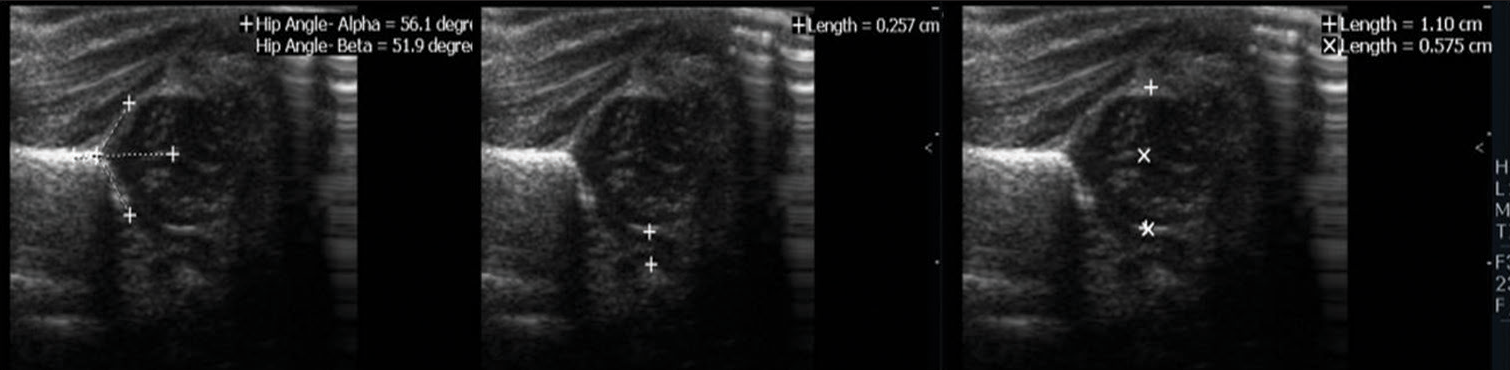
- Graf classification IIa with normal bony rim percentage and pubofemoral distance (between cursors) in 5-day-old infant.
- Graf classification I with normal bony rim percentage and pubofemoral distance (between cursors) in 8 m infant with hyperechoic femoral head epiphyseal center seen.
Ultrasound technique for measuring PFD
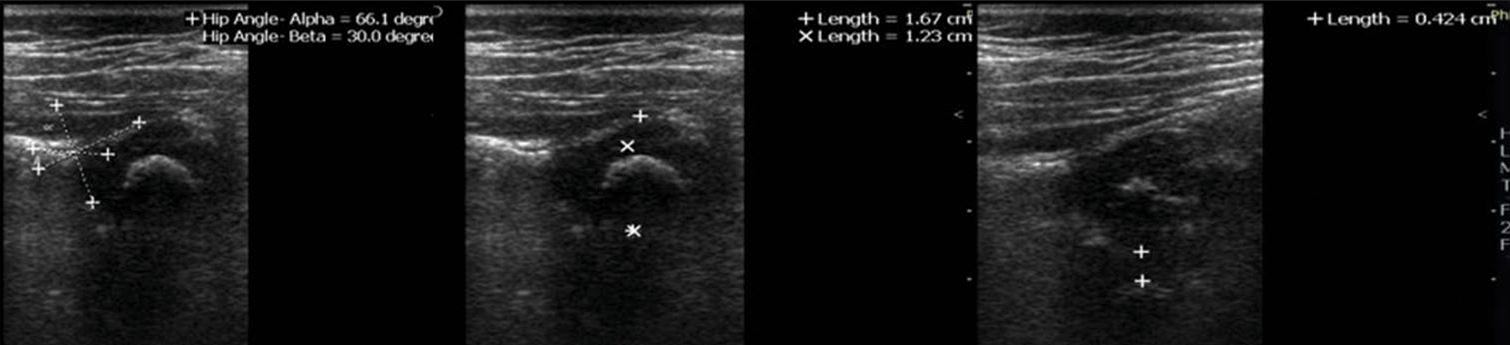
Ultrasound was performed in the presence of the parents by a single experienced radiologist with 5 years of experience in pediatric ultrasound. A high-frequency linear transducer (10–15 Hz) (Philips HDE7) was used. The technique was adopted by Teixeira et al.[14] The infant was positioned in a lateral position with the target hip flexed at 90° in a neutral position [Figure 4a]. The transducer was placed perpendicular to the examination table for examination of the hip in the coronal plane until the pubic bone (PB) and femoral head (FH) were seen. At this point, PFD was measured between the medial margin of the FH epiphysis and the superior pubic ramus. The quality criteria adopted to ensure that the above-mentioned imaging plane was adequate and included two cartilaginous landmarks, that is, epiphyseal center and the triangular hyperechoic fibrocartilaginous rim, and three bony landmarks, that is, horizontal iliac wing, the bony acetabular roof at its greatest depth, and the PB [Figure 4b]. Measurement of PFD was done for both hips.
- (a) Image demonstrating the positioning of the patient in lateral decubitus with the side to be examined upward, and the correct positioning of the transducer. The examined limb is in flexed and neutral position with a transducer perpendicular to the bed, to obtain an image of the hip in the coronal plane. (b) Anatomical landmarks in the normal hip: Muscular planes: Tensor fascia lata (TFL) muscle, gluteus medius (GMED) muscle, and gluteus minimus (GMIN) muscle. Bony landmarks: Acetabulum (AB) and pubic bone (PB). Cartilaginous structures: Femoral head (FH), acetabular cartilage (AC), and pubic cartilage (PC). Others: Labrum (LA) and ligamentum teres (LT) (indistinguishable from the fatty pulvinar (PU) and pubofemoral distance (between cursors).
Statistical analysis
The data were recorded in the form of tables. The mean and the standard deviation of the PFD were calculated in both neonatal and postneonatal groups as well as sexes. The mean difference between the two hips was also calculated. Student’s t-test was applied to compare the mean and standard deviation in the male and the female groups as well as, left and right hips in both neonatal and postneonatal groups, and P-value was calculated for these parameters to determine the significance.
RESULTS
It was seen that the average PFD in 141 infants included in the study (282 hips) was 3.23 ± 0.83 mm. In the neonatal group (<1 month) with 88 patients, the average PFD was 3.15 ± 0.79 mm (confidence interval [CI] 95%). In the postneonatal group (>1–12 months) with 53 patients, the average PFD was 3.47 ± 0.84 mm (CI 95%) [Table 1, Figure 5]. The mean difference in PFD values between the neonatal and postneonatal two groups was 0.55 mm ± 0.52 (0–3.5 mm). There was no significant difference between the PFD of the left and right hips among the neonatal and postneonatal groups [Table 2, Figures 6 and 7]. In males (77 infants; 154 hips), the average PFD was 3.29 ± 0.85 mm, and in females (64 infants, 128 hips), it was 3.23 ± 0.81 mm. P valve comparing both groups was 0.5471, and thus, there was no significant difference among the PFD of the two sexes [Table 3, Figure 8]. Further, there was no significant difference between left and right hips among the PFD of the male and female groups [Table 4, Figure 9].
| Diagnosis | PFD (mm) | Standard deviation (mm) |
|---|---|---|
| Neonatal group (n=176) | 3.15 | 0.79 |
| Post neonatal group (n=106) | 3.47 | 0.84 |
PFD: Pubofemoral distance
| Mean PFD (mm) | Standard deviation | P-value | |
|---|---|---|---|
| Neonatal group(n=88) | |||
| Left hip | 3.09 | 0.69 | 0.2803 |
| Right hip | 3.22 | 0.89 | |
| Post neonatal group(n=53) | |||
| Left hip | 3.49 | 0.83 | 0.8545 |
| Right hip | 3.46 | 0.85 |
PFD: Pubofemoral distance
| Mean PFD | Standard deviation | P-value | |
|---|---|---|---|
| Male (n=154) | 3.29 | 0.85 | 0.5471 |
| Female(n=128) | 3.23 | 0.81 |
PFD: Pubofemoral distance
| Mean PFD (mm) | Standard deviation | P-value | |
|---|---|---|---|
| Female (n=64) | |||
| Left hip | 3.24 | 0.73 | 1 |
| Right hip | 3.24 | 0.88 | |
| Male (n=77) | |||
| Left hip | 3.24 | 0.81 | 0.4209 |
| Right hip | 3.35 | 0.89 |
PFD: Pubofemoral distance
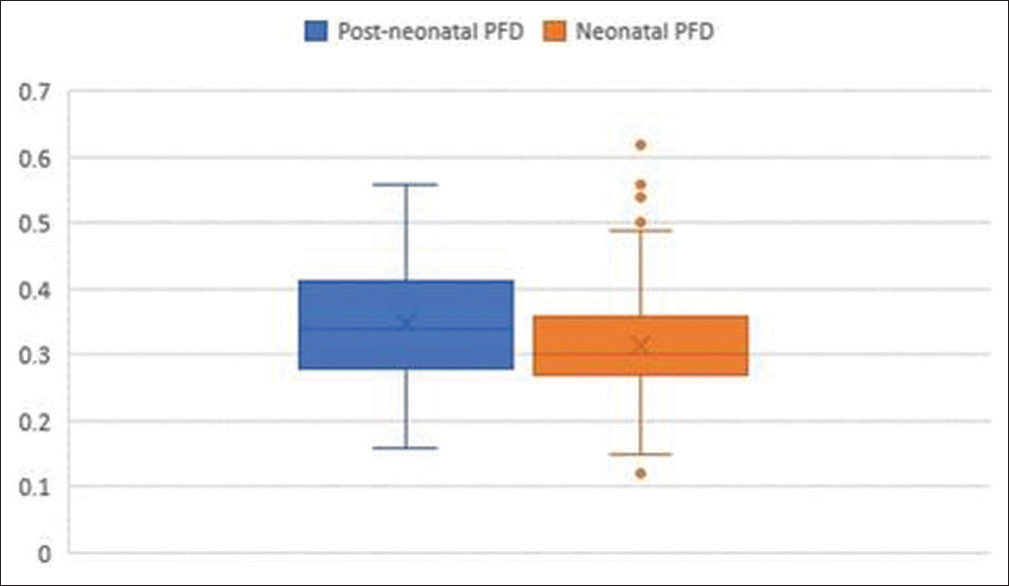
- Average pubofemoral distance in neonatal age group (88 infants) and postneonatal age group (53 infants).
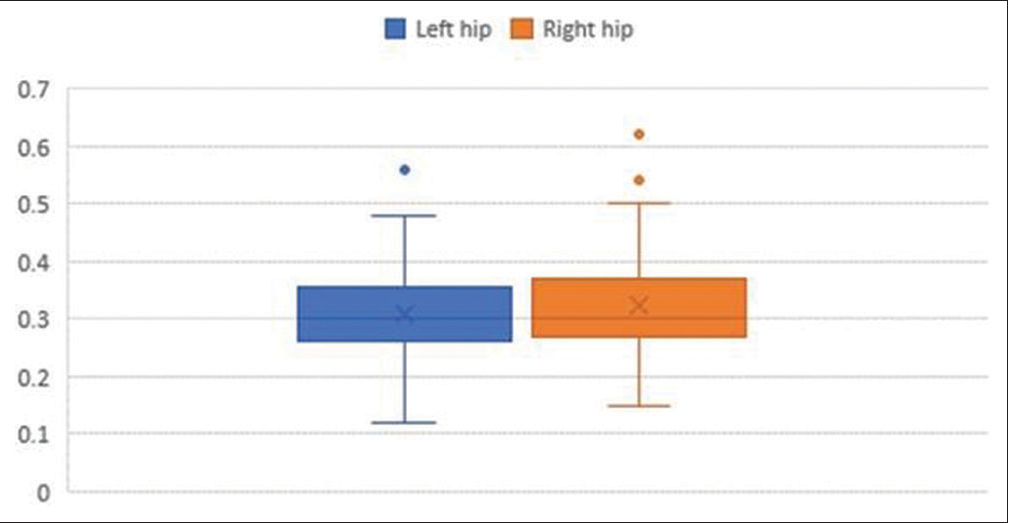
- Average pubofemoral distance in the left and right hip in neonatal (<1 month) age group (88 infants).
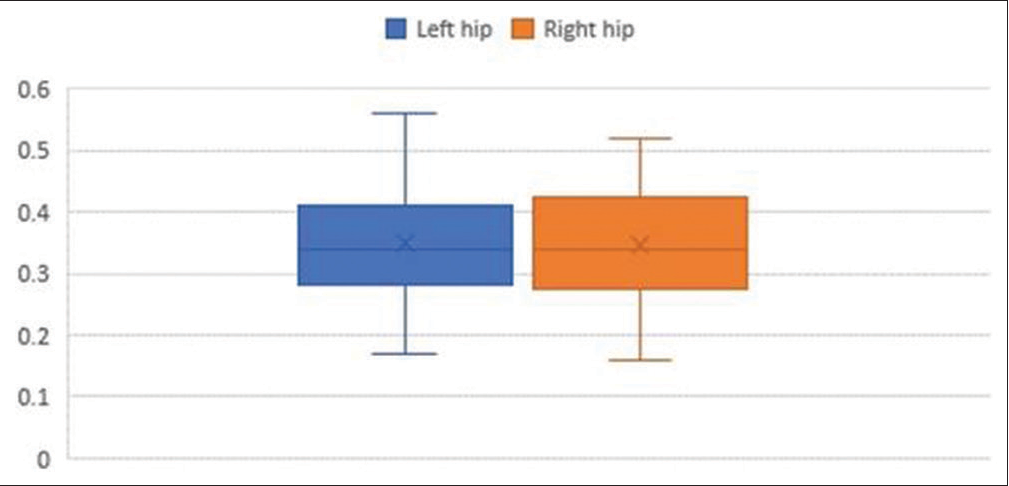
- Average pubofemoral distance in the left and right hip in the postneonatal (>1 month–12 month) age group (53 infants).
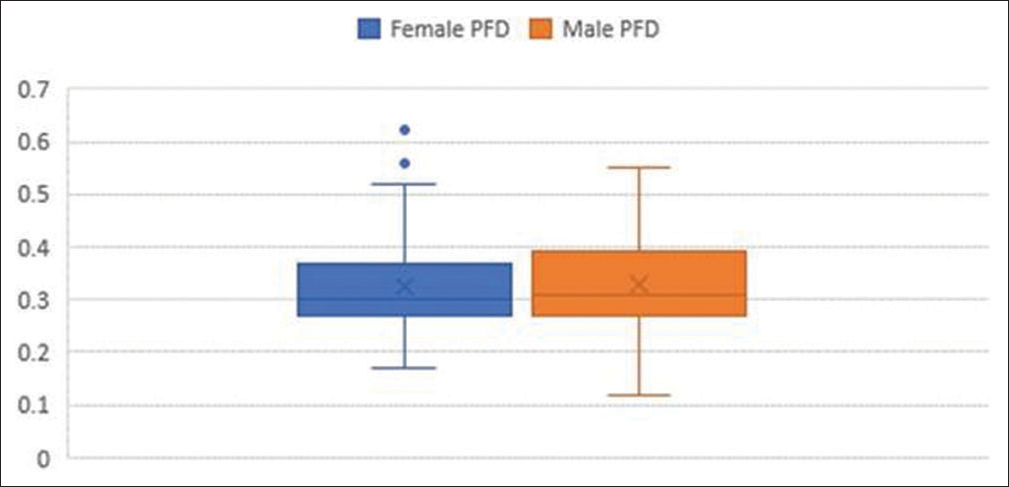
- Average pubofemoral distance in males (77) and females (64).
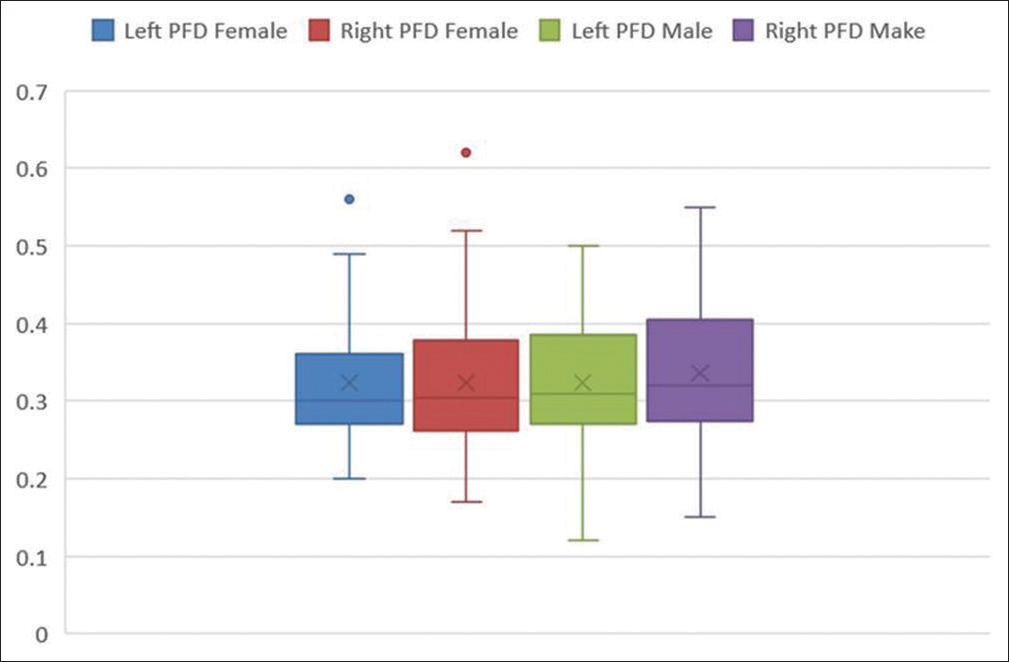
- Average pubofemoral distance in the left and right hips of males and females.
DISCUSSION
DDH denotes a range of hip abnormalities in the newborn period that can progress to dislocation and deformities. Worldwide, the incidence of DDH varies widely from as <1/1000 to as many as 34/1000 live births.[15] It occurs more often in girls with the predominant involvement of the left hip.[16] In our study, however, the number of males (77) was more than females (64) likely due to hospital and referral bias as we included all infants who were sent by any departments with complaints that were non-orthopedic in nature.
The incidence in India varies from as low as 0.17 in southern India to as high as 18.7 in a few parts of northern India.[17-21] Kremli et al.[22] reported a very low prevalence of DDH in communities that carry children around the waist of mothers with the hips abducted and flexed such as India, China, and Africa. Poor socioeconomic status and a large number of children give parents less time to attend to children. As such, despite the relatively low prevalence in our country, late diagnosis of DDH is common.[23]
The pathophysiology of DDH includes both instability and abnormal morphology.[24,25] Instability of ligaments results in malposition of the head of the femur outside AB which impedes proper development of AB. This results in deformity of FH which becomes flattened posterolaterally. This space between the FH and AB is eventually filled with fibro-fatty tissue called pulvinar (PU). The capsule also thickens and may develop an hourglass deformity. Due to abnormal dynamics, FH ossification is often delayed. The changes develop usually over a period of time and if detected after the age of 3 months, it is considered a late diagnosis.[25]
The techniques of clinical evaluation as given by Ortolani which includes maneuvers[26] with other tests (like Barlow’s test) to identify dislocated and unstable hips miss the mild forms of acetabular dysplasia and instability to an extent of 50%. These patients present with deformities in later years of life.[4] Thus, the role of screening infants with ultrasound is of immense importance to identify cases with DDH.[14] Many studies in the past estimated the efficacy of screening infants by USG and showed a higher sensitivity for the detection of DDH as compared to physical examination alone.[9,24] In India, currently, only clinical screening is done which is carried out by a pediatrician or obstetrician at the time of birth. The use of USG as a screening test is currently limited to infants with a positive physical examination[6] and those considered at risk for DDH. No national screening protocol or national registry and data exist on the incidence of DDH estimated clinically or ultrasonographically.[27]
Being a radiation-free and pediatric-friendly modality, there are no absolute contraindications for the use of USG in the infant’s hip for DDH. It can be used for diagnosis as well as for follow-up of a patient undergoing treatment. Being an operator-dependent modality, ultrasound has a few drawbacks. The results can be false-positive in patients <2 weeks old due to inherent physiological laxity in the hip joint capsule.[6,25] With increasing age, USG becomes less reliable as compared to radiography due to progressive ossification of the FH.
The techniques of USG have evolved with time. The quest for making an early, reliable, and easily reproducible objective method for diagnosis continues with the ultimate aim to improve long-term outcomes for these patients. At present, Graf and Schuler method[5] combined with the Harcke and Grissom technique[6] is used for assessing the hips in newborns and for determining the efficacy of treatment protocols for long-term benefit in patients. Although used extensively, this technique can be complex and difficult to perform by inexperienced sonographers and radiologists, and it requires a steep learning curve.[28-30] The interobserver agreement regarding measurements of Graf alpha- and beta-angles can be poor and might depend on the radiologist’s experience.[31,32] The discordance in the absolute angle values might lead to overtreatment or even to false-negative cases.
The measurement of PFD, on the other hand, is a simple tool that is feasible for different coronal planes.[13,33] It corresponds to an enlargement of the PU in the case of DDH, which could occur precociously before acetabular changes.[1] A single measurement taken between two fixed points is not likely to create confusion and decrease the variability among people measuring it. Moreover, PFD measurements and the Graf method can be complementary in the diagnosis and management of DDH.[29,34]
The previous studies that have reported normal values of PFD in the hip include Treguier et al.[1] They studied 1439 normal hips of infants in tertiary hospitals in France and reported an average PFD of 4.6 ± 1.0 mm (1.9–9.1 mm). Teixeira et al.[14] studied 116 infants in Brazil and the mean PFD of the non-dysplastic group comprising 211 hips (69 females and 37 males) was 3.09 mm at the neutral position and 3.64 mm with the hip in the flexed position. Motta et al.[34] studied 1670 neonates in Brazil and compared the Grafs method with PFD. The mean PFD in non-dysplastic hips in their study was 3mm. Ban et al.[35] evaluated PFD in 240 infants in China and established reference PFD values in infants aged <12 months. The mean PFD in infants <1 month was 0.185 ± 0.018 cm (0.180–0.190) and the mean value of PFD increased in values with age. There was no significant influence on the value of PFD by laterality or gender. Husum et al.[36] in Denmark measured PFD and performed the Graf method comparing a group of infants under treatment for DDH with another group of untreated infants. They concluded that the mean PFD in the control group is 3.4 mm (3.3–3.6). In our study, the mean PFD was 3.23 ± 0.83 mm which was similar to the studies in which the PFD was measured in a position similar to the Grafs method.[14,34,36] There is discrepancy in our study as compared to Ban Y et al.[35] because they used abducted and flexed position of hip to evaluate PFD (similar to Treguier et al.[1]) unlike our study which used neutral and flexed position.
Studies have shown that PFD measurements are highly accurate for assessing dysplastic hip.[1,34,36,37] Interobserver agreement for performing PFD measurements was almost perfect, regardless of the observer’s experience.[1,34-37] In addition, these measurements do not change significantly with different hip positions (flexion or neutral) of dysplastic hips.[1] In our country where an adequate number of skilled radiologists are not available in peripheral healthcare facilities, a simple ultrasonographic technique like PFD can be employed, which can be performed with ease and is comparatively a simple measurement that is easily reproducible[1] making mass screening and therefore early detection of DDH possible. Further studies need to be done, however, to find its values in the cases with DDH to determine the cutoff in such cases in the Indian population.
There were many limitations to our study. The sample size was small and the patients were recruited from the population which came to the hospital. It is our belief that a larger sample size would further validate the study and taking a sample from the general population is needed to remove the hospital-based population bias. Another limitation of the study was that patients who already had normal hips based on our ultrasound criteria were included in the study. Clinical evaluation and follow-up of the cases for the development of DDH later in life could not be done.
CONCLUSION
We believe that PFD measurement is a simple and reproducible ultrasound parameter. In our study, the average PFD in 141 infants was 3.23 ± 0.83 mm. In the neonatal group, the average pubofemoral distance was 3.15 ± 0.79 mm and in the postneonatal group, it was 3.47 ± 0.84 mm. No significant difference was observed in the average PFD among the two sexes and between the left and right hips of both neonatal and postneonatal groups. There is a need for more studies having a larger population and from different locations across India to establish an Indian nomogram, with the ultimate objective to standardize measurement references for the diagnosis of DDH.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pubofemoral distance: An easy sonographic screening test to avoid late diagnosis of developmental dysplasia of the hip. Eur Radiol. 2013;23:836-44.
- [CrossRef] [PubMed] [Google Scholar]
- Late diagnosis of congenital dislocation of the hip and presence of a screening programme: South Australian population-based study. Lancet. 1999;354:1514-7.
- [CrossRef] [PubMed] [Google Scholar]
- Routine ultrasound screening for neonatal hip instability. Can it abolish late presenting congenital dislocation of the hip? J Bone Joint Surg Br. 1994;76:534-8.
- [CrossRef] [Google Scholar]
- The use of ultrasonography in developmental dysplasia of the hip. Acta Orthop Traumatol Turc. 2007;41(Suppl 1):6-13.
- [Google Scholar]
- Guide to sonography of the infant hip In: Stuttgart. New York: Thieme Medical Publishers; 1987.
- [Google Scholar]
- Performing dynamic sonography of the infant hip. AJR Am J Roentgenol. 1990;155:837-44.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of a nationwide general ultrasound screening system for developmental disorders of the hip: The Austrian hip screening program. J Child Orthop. 2014;8:3-10.
- [CrossRef] [PubMed] [Google Scholar]
- Cochrane review screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013;8:11-54.
- [CrossRef] [PubMed] [Google Scholar]
- Role of ultrasound in evaluation of developmental dysplasia of the hip in infants. Open J Pediatr. 2017;7:1-12.
- [CrossRef] [Google Scholar]
- AIUM practice guideline for the performance of an ultrasound examination for detection and assessment of developmental dysplasia of the hip. J Ultrasound Med. 2013;32:1307-17.
- [CrossRef] [PubMed] [Google Scholar]
- ACR appropriateness criteria on developmental dysplasia of the hip--child. J Am Coll Radiol. 2009;6:551-7.
- [CrossRef] [PubMed] [Google Scholar]
- European society of paediatric radiology's task force group on DDH-recommendations on hip screening. In: IPR London. London: European Society of Paediatric Radiology; 2011. p. :2011.
- [Google Scholar]
- Ultrasound of the neonatal hip: Initial evaluation and follow-up. J Radiol. 2011;92:142-65.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between graf method and pubofemoral distance in neutral and flexion positions to diagnose developmental dysplasia of the hip. Eur J Radiol. 2015;84:301-6.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of developmental dysplasia of hip among neonates in a tertiary care setting of Odisha. Indian J Orthop. 2003;3:346-9.
- [Google Scholar]
- The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011;2011:238607.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital malformations in live born infants in a rural community. Indian Pediatr. 1983;20:45-9.
- [Google Scholar]
- Spectrum of congenital malformations in the new born. Indian J Pediatr. 1980;47:239-44.
- [CrossRef] [PubMed] [Google Scholar]
- Hip instability in new borns in an urban community. Natl Med J India. 1992;5:269-72.
- [Google Scholar]
- Late presentation of developmental dysplasia of the hip in children from southwest India-will screening help? Indian J Orthop. 2003;37:210-4.
- [Google Scholar]
- Hip ultrasonography in infants and children. Indian J Radiol Imaging. 2007;17:280-9.
- [CrossRef] [Google Scholar]
- Musculoskeletal system and vascular imaging In: Pediatric Sonography (3rd ed). United States: Lippincott Williams; 2002. p. :625-72.
- [Google Scholar]
- A little known sign and its importance for the early diagnosis of congenital hip preluxation. Paediatrics. 1937;45:129-36.
- [Google Scholar]
- Ultrasound profile of hips of South Indian infants. Indian Pediatr. 2011;48:475-7.
- [CrossRef] [PubMed] [Google Scholar]
- The role of ultrasound in the diagnosis and management of congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1991;73:622-8.
- [CrossRef] [Google Scholar]
- Assessment of variations in the measurement of hip ultrasonography by the graf method in developmental dysplasia of the hip. J Pediatr Orthop B. 2001;10:89-95.
- [CrossRef] [PubMed] [Google Scholar]
- Inter-and intraobserver reliability in Graf 's sonographic hip examination. Z Orthop Unfall. 2008;146:624-9.
- [CrossRef] [PubMed] [Google Scholar]
- The reliability of ultra-sonographic assessment of neonatal hips. J Bone Joint Surg Br. 1993;75:479-82.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonography in developmental dysplasia of the hip: What have we learned? Pediatr Radiol. 2012;42:1418-31.
- [CrossRef] [PubMed] [Google Scholar]
- Dépistageéchographique de la luxation congénitale de hanchecentrésurlamesure du fond cotyloidien In: Journées Franc¸ Aises de Radiologie. Paris: Elsevier Masson SAS; 2006.
- [CrossRef] [Google Scholar]
- Measurement of pubofemoral distance in the diagnosis of developmental dysplasia of the hip: Sensitivity and specificity. J Ultrasound Med. 2022;41:1205-12.
- [CrossRef] [PubMed] [Google Scholar]
- Establishing reference values for the pubofemoral distance in normal infant medial hips by ultrasound. Acta Radiol. 2021;62:551-6.
- [CrossRef] [PubMed] [Google Scholar]
- Suggestion for new 4.4 mm pubo-femoral distance cut-off value for hip instability in lateral position during DDH screening. Acta Orthop. 2019;90:88-93.
- [CrossRef] [PubMed] [Google Scholar]
- The pubo-femoral distance decreases with Pavlik harness treatment for developmental dysplasia of the hip in newborns. Skeletal Radiol. 2017;46:1201-7.
- [CrossRef] [PubMed] [Google Scholar]







