Translate this page into:
Improving pre-operative MRI diagnosis of peroneal tendon tears with a new objective sign and assessing the value of peroneus brevis fatty atrophy

*Corresponding author: David J. Wang, Department of Medical Imaging, St. Joseph’s Health Care London, London, Ontario, Canada. djwang89@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wang DJ, Harris G, Boubalos JJ, Swami VG, Lau JT, Naraghi AM, et al. Improving pre-operative MRI diagnosis of peroneal tendon tears with a new objective sign and assessing the value of peroneus brevis fatty atrophy. Indian J Musculoskelet Radiol 2022;4:18-25.
Abstract
Objectives:
We aimed to compare the diagnostic performance of an objective set of magnetic resonance imaging (MRI) criteria named the cleft sign with traditional reads for pre-operative diagnosis of peroneal tendon tears. We also investigated the relationship between peroneus brevis tendon tears and muscle quality.
Material and Methods:
Two blinded readers retrospectively and independently evaluated pre-operative ankle MRI studies of 38 patients who had undergone peroneal tendon surgery for peroneal tendon tears, peroneus brevis muscle quality, and the cleft sign. MRI examinations from 38 control subjects were also reviewed for peroneus brevis muscle quality. The diagnostic performances of MRI for peroneal tendon tears with and without application of the cleft sign were analyzed. The correlation between peroneus brevis fatty atrophy and tendon tears was also examined.
Results:
In patients without prior peroneal surgery, the sensitivity and specificity of MRI for peroneus brevis tendon tears were 60%/89% and 80%/78% for readers 1 and 2, respectively. Application of the cleft sign significantly increased sensitivity in reader 1 to 95%, with a non-significant increase in accuracy in both readers. The interobserver reliability for the cleft sign was moderate for peroneus brevis (κ = 0.57). No significant difference in peroneus brevis muscle quality was present between subjects with and without peroneus brevis tendon tears and between surgical and control patients.
Conclusion:
In patients without prior peroneal tendon surgery, the cleft sign can significantly improve reader diagnostic sensitivity for peroneus brevis tears. The muscle quality of the peroneus brevis has limited value in MRI diagnosis of peroneal tendon tears.
Keywords
Peroneal tendon tear
Peroneus brevis
Peroneus longus
Cleft sign
INTRODUCTION
Peroneal tendon tears are a common cause of chronic lateral ankle pain and instability.[1] Injuries are most commonly traumatic but can also result from inflammatory conditions such as rheumatoid arthritis.[2] Anatomical variations such as the presence of peroneus quartus and peroneal tubercle hypertrophy may also be contributory.[3] Given the non-specific clinical presentation, the diagnosis of peroneal tendon injury is often delayed.[2] Even with a comprehensive history and physical examination, MRI in the current era is invaluable in distinguishing between various causes of ankle symptoms, such as ligamentous injury, tendinous pathology, osteochondral lesions, and synovitis. Peroneal pathologies include tendinosis/tenosynovitis, tear, and subluxation/ retinaculum injury, with commonly associated soft-tissue findings including lateral collateral ligament complex tears, anterolateral impingement lesions, and synovitis.[1-3] In patients with known pathology who have failed conservative management, MRI also plays an important role in pre-operative planning. Surgical management of peroneal tendon tears includes debridement, repair/tubularization, tenodesis, tendon transfer, and autograft/allograft reconstruction.[4,5]
Despite the value of MRI, diagnosing peroneal tendon pathology can be challenging due to various anatomic and technical considerations. The oblique inframalleolar course of the tendons can predispose to magic angle and partial volume averaging effects.[6] The normal flattening of the peroneus brevis tendon in the retromalleolar groove can also simulate a partial thickness tear.[7] Reported diagnostic performances of pre-operative MRI for peroneus brevis tendon tears have varied widely, with sensitivities and specificities ranging between 55–97% and 63–90%, respectively.[1,8-14] These previous studies have been limited by small sample sizes and heterogeneous study designs, most notably with inconsistent imaging criteria of tendon tears.
To improve the diagnostic accuracy of MRI for peroneus brevis tendon injuries, recent authors have suggested analyzing the peroneus muscle belly for signs of fatty infiltration.[15] Based on shoulder rotator cuff literature, it has been hypothesized that the degree of muscle fatty degeneration correlates with tendon pathology and is a predictor of outcome after surgical tendon repair.[16,17] The authors found that patients with peroneus brevis tendon tears on MRI demonstrated significantly higher grades of fatty atrophy compared with controls. However, one important limitation of their study was the lack of surgical confirmation of tendon status.
The objectives of this study are to further investigate the performance of pre-operative MRI for peroneal tendon tears and to establish a set of practical and objective imaging criteria for diagnosing peroneal tendon tears. Second, we aim to examine the value of peroneus brevis muscle status on MRI in assessing tendon tears.
MATERIAL AND METHODS
Patient selection
Approval from the Research Ethics Board was obtained and patient consent was waived. One hundred and five consecutive patients who had undergone peroneal tendon surgery between January 1, 2004, and December 31, 2019, were identified from a surgical database. Inclusion criteria were patients who had a complete pre-operative ankle MRI before peroneal tendon surgery. Patients who had incomplete MRI examinations and those with a time interval of >1 year between MRI and surgery were excluded from the study, yielding 38 subjects with complete pre-operative MRIs available for review. Thirty-eight age- and sex-matched controls from the same study period were selected through a search of the radiology information system. Control patients had a variety of clinical symptoms but were excluded if the indication suggested lateral ankle pain or clinically suspected peroneal pathology. Controls who had descriptions of peroneal tendon pathology on the MRI report were also excluded from the study. The control subjects were included for comparison of peroneal muscle morphology between surgical and non-surgical patients.
Clinical data evaluation
All clinical data were accessed through the electronic patient record. The patients’ sex and age were recorded. Intraoperative findings for the peroneus brevis and peroneus longus tendons were recorded as “tear” and “no tear” as the types of tendon tears were not consistently described. The dates of the pre-operative MRI and surgery were recorded. Prior lateral ankle surgical intervention was recorded as either directly involving the peroneal tendons (peroneal tendon repair, debridement, and rerouting for lateral ligament reconstruction) or not (Open reduction and internal fixation [ORIF], fibular groove deepening, etc.).
MRI evaluation
All MRI examinations were obtained on a Signa Excite 1.5T scanner (General Electric Medical Systems, Milwaukee, Wisconsin) using system software 12.0 and a 4-channel receive-only extremity coil (Quad Knee Coil, General Electric Medical Systems). The patients were scanned supine with ankle dorsiflexion of 90 degrees with the following protocol:
Sagittal T2-weighted fast spin echo with fat saturation; TR 3000 ms, TE 80 ms, slice thickness 4.0 mm, and field of view (FOV) 16 × 16 cm.
Sagittal T1-weighted spin echo; TR 400 ms, TE 9 ms, slice thickness 4.0 mm, and FOV 16 × 16 cm.
Axial T2-weighted fast spin echo with fat saturation; TR 4000 ms, TE 85 ms, slice thickness 4.0 mm, and FOV 16 × 16 cm.
Axial intermediate-weighted fast spin echo; TR 3500 ms, TE 40 ms, slice thickness 4.0 mm, and FOV 16 × 16 cm.
Coronal intermediate-weighted fast spin echo; TR 3500 ms, TE 40 ms, slice thickness 4.0 mm, and FOV 14 × 14 cm.
The MRI examinations of the surgical and control subjects were randomized and independently reviewed by two musculoskeletal fellows who were blinded to the original MRI and operative reports. The readers assessed for abnormalities of the peroneus brevis and longus tendons and the peroneus brevis muscle belly quality.
Given the variable criteria for tendinosis and partial tears, readers assessed tendon morphology as tendon thickening +/− increased signal, reflecting tendinosis and intrasubstance tears, and tendon flattening, reflecting the expected flattening of the peroneus brevis in the retromalleolar groove. Partial thickness tears were subdivided into longitudinal split tears and transverse tears. Given the lack of an established definition for partial thickness peroneal tendon tears and our objective of creating such criteria, reviewers were initially asked to assess partial tears based on prior experience, with findings including intratendinous fluid signal clefts and tendon separation into two discrete bundles. Complete tendon tears were defined as abnormal intermediate or T2-weighted signal replacing the entire cross-sectional area of the tendon, with no visible intact tendon fibers.
For analysis of pre-operative MRI performance, we combined the reviewers’ selections into binary categories of “tear” (including partial tear – longitudinal split and transverse tears and complete tears) and “no tear” (including normal, tendon thickening, and thinning). This was done to account for insufficient sample sizes for each tear type and to reflect the surgical data, which recorded peroneal pathology as tears versus no tear but did not consistently distinguish between tear types or tendinosis. Ultimately, our goal was to describe MRI findings that could accurately predict a surgically proven tear.
The peroneus brevis muscle belly was assessed using the Goutallier classification for rotator cuff atrophy.[16,17] Assessment was based on non-fat saturated axial intermediate-weighted images as we do not routinely include an axial T1-weighted sequence on standard ankle MRI examinations [Figure 1]. Atrophy was determined based on analysis of the entirety of the muscle belly visualized within the field of view. Patients whose MRI studies did not include the peroneus brevis muscle belly in the field of view were excluded for this portion of the analysis.
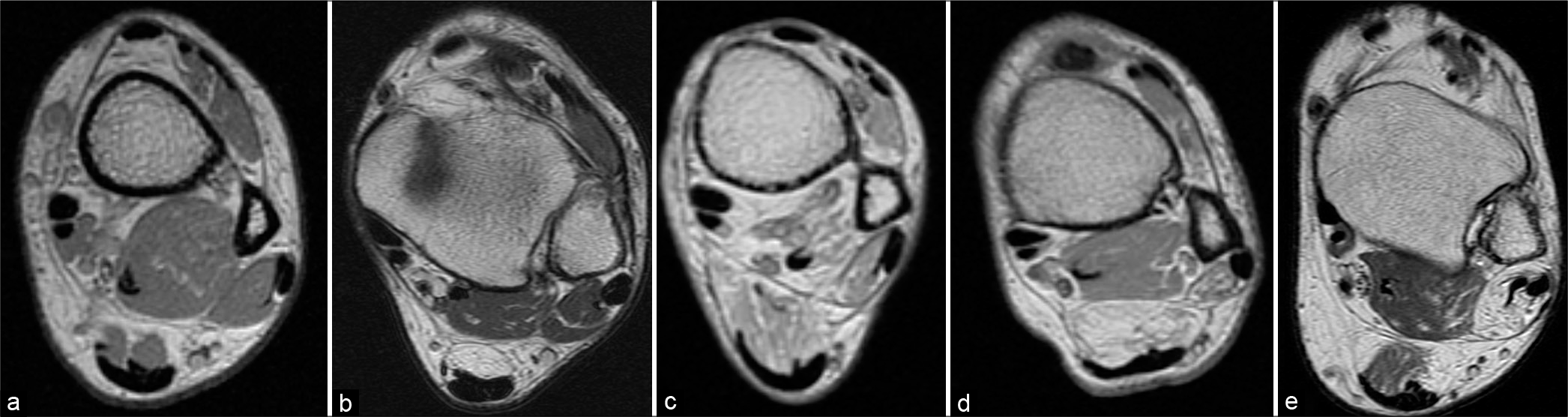
- Peroneus brevis muscle fatty atrophy grading. (a) Grade 0, absence of intramuscular fat. (b) Grade 1, muscle contains some fatty streaks. (c) Grade 2, < 50% muscle fatty atrophy. (d) Grade 3, 50% muscle fatty atrophy. (e) Grade 4, >50% muscle fatty atrophy.
Cleft sign analysis
We developed a practical set of objective criteria for the assessment of peroneal tendon tears, which we termed the “cleft sign.” This is defined as an intratendinous intermediate to high T2-weighted signal, involving at least 50% of the tendon diameter, that breaches the tendon surface and is present on at least two consecutive axial slices [Figures 2 and 3].
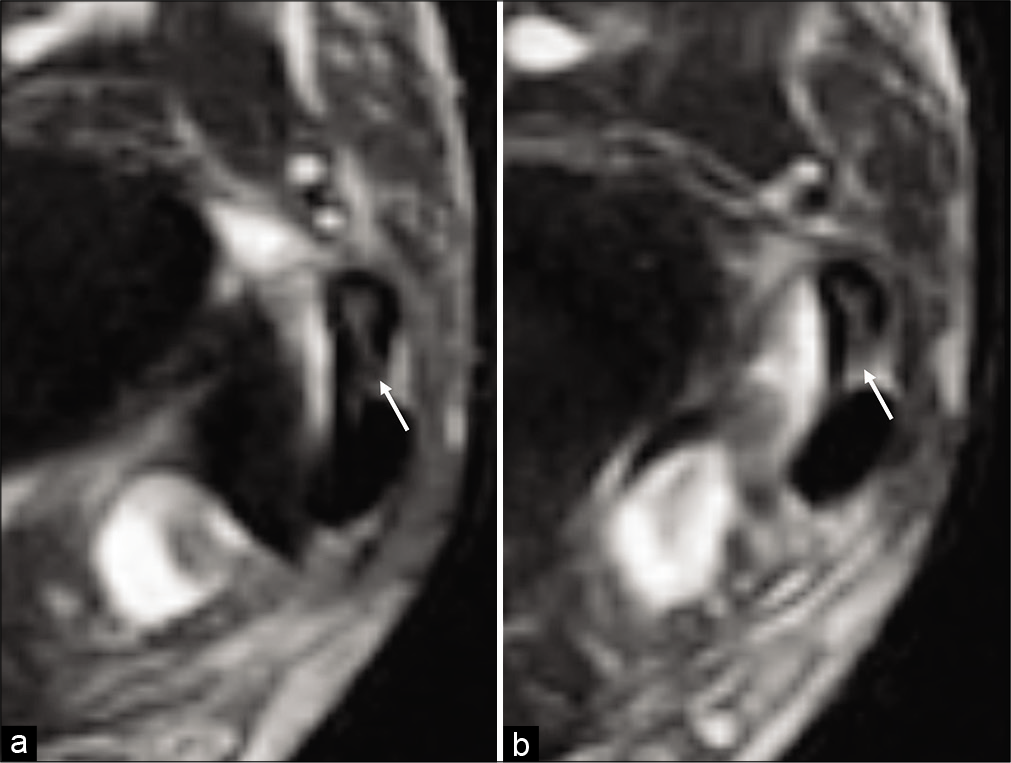
- A 35-year-old man with a surgically confirmed partial thickness tear of the peroneus brevis tendon following an acute soccer injury. Consecutive axial T2-weighted fat saturated MR images from superior (a) to inferior (b) of the inframalleolar lateral ankle demonstrate the cleft sign, manifested as intermediate signal within the peroneus brevis tendon spanning at least 50% of the tendon and breaching the posterior tendon surface (white arrow), present on both slices.
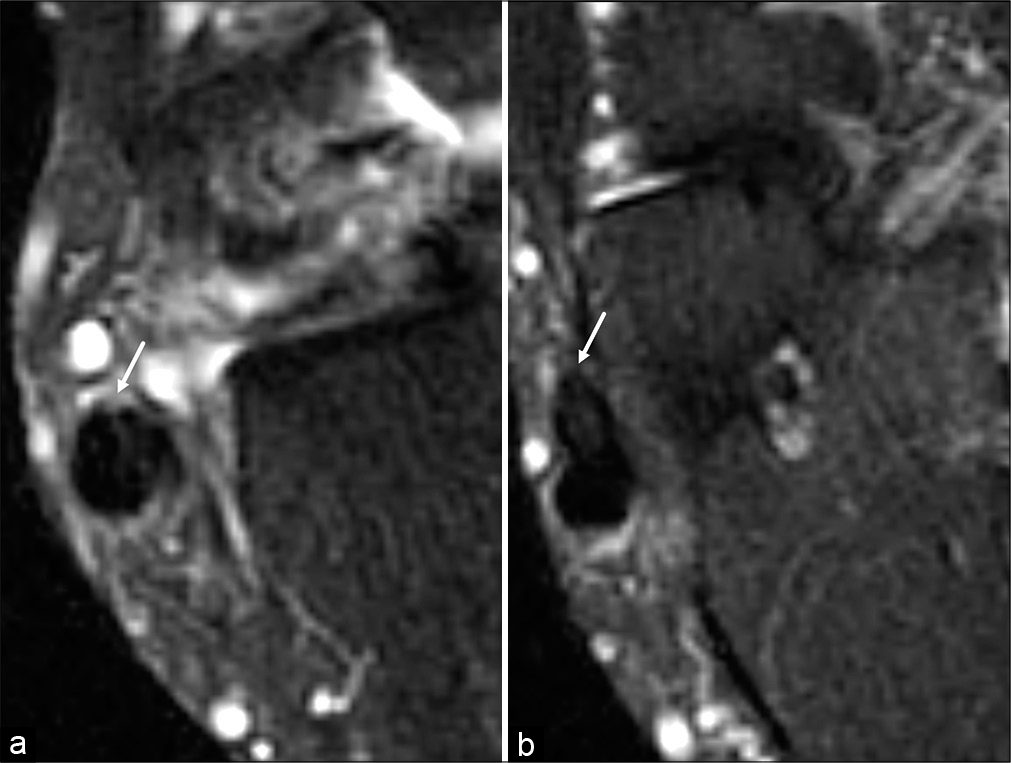
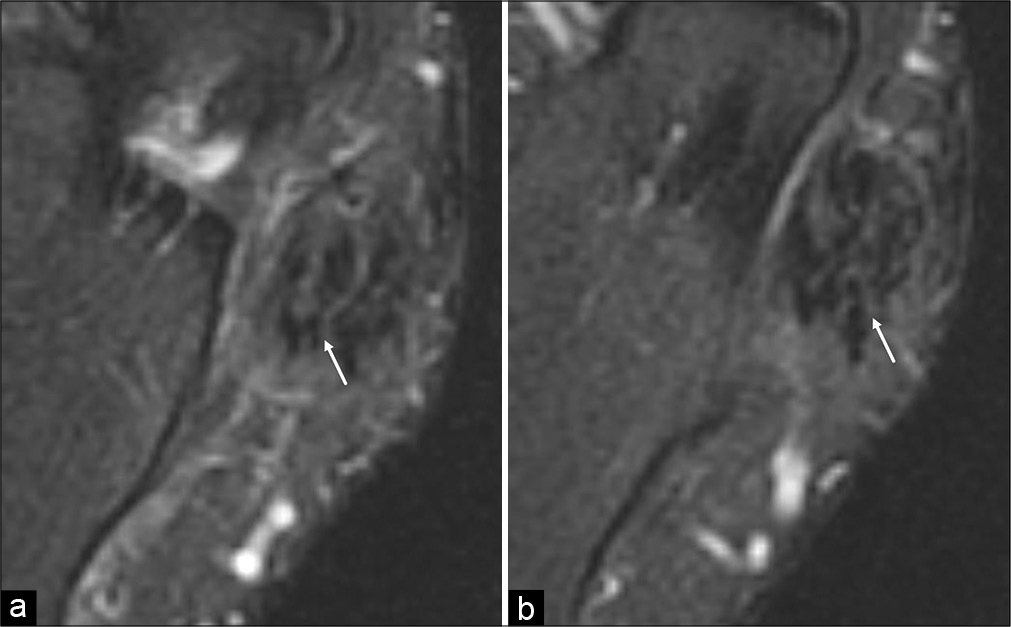
- A 61-year-old man with a surgically confirmed partial thickness tear of the peroneus brevis tendon following a work-related injury. Consecutive axial T2-weighted fat saturated MR images from superior (a) to inferior (b) of the inframalleolar lateral ankle demonstrate a positive cleft sign (white arrow). This case was called negative for a peroneal tendon tear on both the original report and by both readers.
Concerning the peroneus brevis, we do not endorse the use of the cleft sign in the retromalleolar location given the routine flattening in this location, increasing susceptibility to partial volume average effects. For the peroneus longus, we do not endorse the use of the cleft sign beyond the peroneal tubercle. In our experience, the peroneus longus tendon often contains increased intrasubstance signal with surface breach as it enters the fibro-osseous tunnel plantar to the cuboid, possibly due to a fanning-out morphology or concurrent tendinosis/tenosynovitis [Figure 4].
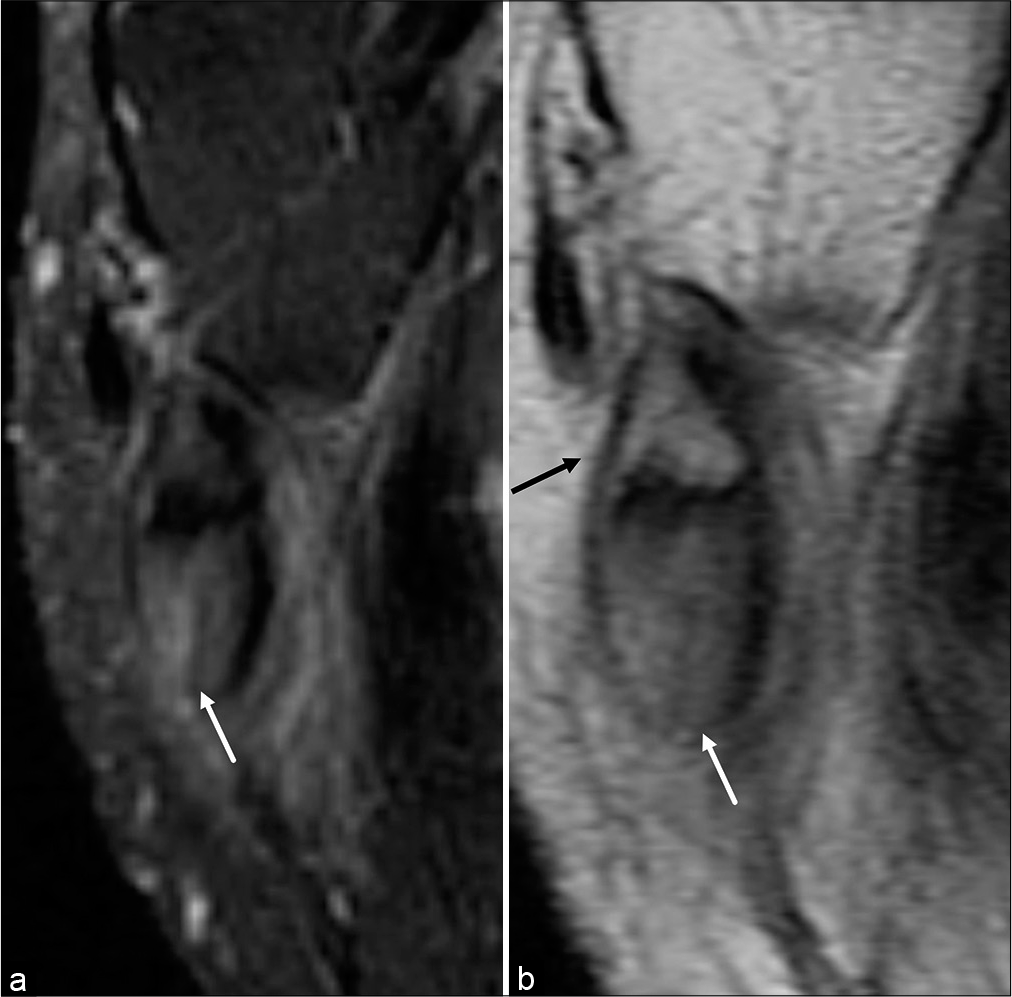
- A 48-year-old man with surgically confirmed peroneus longus tenosynovitis with an intact tendon. Axial T2-weighted fat saturated (a) and axial intermediate-weighted (b) MR images of the peroneus longus tendon distal to the peroneal tubercle demonstrate a falsely positive cleft sign (white arrow). The peroneus longus tendon fans out before surrounding an os peroneum (black arrow).
The readers were unaware of the criteria for the cleft sign at the time of the initial read. The cleft sign was introduced to the readers 2 months following the initial assessment of the peroneal tendons. The readers were asked to re-evaluate the MRI examinations from the surgical cohort for the presence of the cleft sign within the peroneus brevis and longus tendons. The performance of the cleft sign for diagnosing peroneal tendon tears in isolation and in conjunction with traditional MRI assessment was compared to that of traditional MRI assessment alone regarding the surgical data.
Statistical analysis
All statistical analysis was performed with SPSS statistical software, version 25 (IBM, Armonk, New York). The Mann– Whitney U test was used to assess for significant differences in mean peroneus brevis muscle quality. McNemar’s test with binomial distribution was used to test for significant differences in performance measures between traditional MRI reads and using the cleft sign. Interobserver correlation was assessed using a weighted Cohen kappa coefficient for categorical items. The strength of agreement based on coefficient values was defined as follows: 0, poor; 0.01–0.20, slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; and 0.81–1.0, almost perfect.[18]
RESULTS
Patient characteristics
The age, sex, and laterality of the surgical and control groups are shown in [Table 1].
| Surgical Group (n=38) | Control Group (n=38) | |
|---|---|---|
| Age (years) | 43.5 (±9.1) | 43.6 (±10.6) |
| Sex | ||
| Male | 24 (63%) | 21 (55%) |
| Female | 14 (37%) | 17 (45%) |
| Side affected | ||
| Right | 18 (47%) | 20 (53%) |
| Left | 20 (53%) | 18 (47%) |
Surgical findings
The operative reports of the 38 surgical patients documented 26 patients with peroneal tendon tears and 12 patients without tears [Table 2]. Of the 26 patients with tears, 25 patients had peroneus brevis tears and six patients had peroneus longus tendon tears. Five patients had concomitant tears of both peroneal tendons. Only one patient had an isolated tear of peroneus longus.
| Patient centered | |
| No tear | 12 (31.6%) |
| Isolated peroneus brevis tear | 20 (52.6%) |
| Isolated peroneus longus tear | 1 (2.6%) |
| Tears of both peroneus brevis and longus | 5 (13.2%) |
| Tendon centered | |
| Peroneus brevis tendon | |
| No tear | 13 (34.2%) |
| Tear | 25 (65.8%) |
| Peroneus longus tendon | |
| No tear | 32 (84.2%) |
| Tear | 6 (15.8%) |
Nine operative reports described prior peroneal surgery on the affected side. Seven of these involved the peroneus brevis (five repairs/tendon transfers, one debridement, and one Evans procedure) and five involved the peroneus longus (four repairs/tendon transfers and one debridement). An additional five operative reports described prior lateral ankle surgery not involving the peroneal tendons (two ORIF for lateral malleolar fractures, one accessory peroneus tertius resection without affecting the peroneus brevis/longus tendons, one fibular groove deepening, and one lateral column lengthening).
The mean interval between the pre-operative MRI and subsequent surgery was 130 days with a standard deviation of 94 days.
Traditional MRI and cleft sign performance for peroneal tendon tears
Within the entire surgical cohort, the MRI sensitivity, specificity, and accuracy of peroneus brevis tendon tears were 52.0%, 92.3%, and 65.8% for Reader 1 and 76.0%, 69.2%, and 73.7% for Reader 2, respectively [Table 3]. In the subset of patients without prior peroneal surgery, the performance measures improved slightly as a whole for both readers.
| Sensitivity | Specificity | Accuracy | |
|---|---|---|---|
| Reader 1 | 0.52 | 0.92 | 0.66 |
| No prior peroneal surgery | 0.60 | 0.89 | 0.69 |
| + Cleft sign | 0.95a | 0.67 | 0.86 |
| Prior peroneal surgery | 0.17 | 1 | 0.44 |
| + Cleft sign | 0.40 | 0 | 0.22 |
| Reader 2 | 0.76 | 0.69 | 0.74 |
| No prior peroneal surgery | 0.80 | 0.78 | 0.79 |
| + Cleft sign | 0.90 | 0.78 | 0.86 |
| Prior peroneal surgery | 0.60 | 0.50 | 0.56 |
| + Cleft sign | 0.80 | 0 | 0.44 |
The addition of the cleft sign as a diagnostic criteria for peroneus brevis tears, in conjunction with the traditional reads in patients without prior peroneal surgery, resulted in an increase in the number of true and false positives for Reader 1, with a significant improvement in sensitivity (P = 0.016), a non-significant decrease in specificity and a non-significant improvement in accuracy. In Reader 2, all measures improved (without significance), except specificity, which remained unchanged. In patients with prior peroneal surgery, the accuracy of traditional reads was 44.4% and 55.6% for Readers 1 and 2, respectively. The use of the cleft sign in these patients decreased specificity and accuracy for peroneus brevis tears to a non-significant degree.
Within the entire surgical group, the MRI sensitivity, specificity, and accuracy of peroneus longus tendon tears were 16.7%, 93.8%, and 81.6% for Reader 1 and 50.0%, 87.5%, and 81.6% for Reader 2, respectively [Table 4]. In patients without prior peroneal surgery, the performance measures were essentially unchanged for Reader 1 and slightly improved for Reader 2. With the addition of the cleft sign, the performance measures of both readers improved, although not significantly. In patients with prior peroneal surgery, the use of the cleft sign led to overall decreased performance.
| Sensitivity | Specificity | Accuracy | |
|---|---|---|---|
| Reader 1 | 0.17 | 0.94 | 0.82 |
| No prior peroneal surgery | 0.25 | 0.92 | 0.83 |
| + Cleft sign | 0.75 | 0.92 | 0.90 |
| Prior peroneal surgery | 0.50 | 1 | 0.89 |
| + Cleft sign | 0.50 | 0.57 | 0.56 |
| Reader 2 | 0.50 | 0.88 | 0.82 |
| No prior peroneal surgery | 0.75 | 0.92 | 0.90 |
| + Cleft sign | 1 | 0.92 | 0.93 |
| Prior peroneal surgery | 0 | 0.71 | 0.56 |
| + Cleft sign | 0.50 | 0.43 | 0.44 |
The interobserver reliability for peroneal tendon tears on MRI was moderate for peroneus brevis (0.45) and fair for peroneus longus (0.33). The interobserver reliability for the cleft sign was moderate for peroneus brevis (0.57) and substantial for peroneus longus (0.68).
Peroneus brevis muscle quality assessment
Four surgical patients and one control patient were excluded from this part of the analysis as their MRI studies did not include the peroneus brevis muscle belly in the field of view. The interobserver reliability for MRI assessment of peroneus brevis muscle belly quality was almost perfect (0.89). The mean Goutallier grades of peroneus brevis muscles in surgical and control patients are shown in [Table 5]. There was no significant difference between the mean Goutallier grades of peroneus brevis muscle bellies in patients with and without peroneus brevis tendon tears during surgery (Reader 1: U = 159.0, P = 0.44; Reader 2: U = 166.5, P = 0.70). The mean peroneus brevis muscle grades in patients with peroneus brevis tendon tears were 0.68 for Reader 1 and 0.50 for Reader 2. The mean peroneus brevis muscle grades in patients without peroneus brevis tendon tears were 0.33 for Reader 1 and 0.40 for Reader 2. There was also no significant difference between the peroneus brevis muscle belly quality of surgical patients and controls (Reader 1: U = 834.0, P = 0.77; Reader 2: U = 768.0, P = 0.55).
| Mean muscle grade | ||||
|---|---|---|---|---|
| Reader 1 | Reader 2 | |||
| Surgery | 0.55 | 0.46 | ||
| Peroneus brevis tear | 0.68 | 0.5 | ||
| No tear | 0.33 | 0.4 | ||
| Control | 0.33 | 0.31 | ||
| P value | 0.77 | 0.44 | 0.55 | 0.70 |
DISCUSSION
Peroneal tendon pathology is common, with the prevalence of peroneus brevis tears estimated at 11–37% in cadaveric studies.[19] Although MRI is the gold standard diagnostic imaging tool for assessing the peroneal tendons, distinguishing between pathologies can be challenging. To date, there have been no established criteria for peroneal tendon tears on MRI. While complete tears are less of a diagnostic dilemma, partial thickness tears can have a variable appearance. For example, tendons with partial thickness tears can be thickened or thinned with intermediate or high, linear, or globular T2 signals.[20-22] Split tears of the peroneus brevis tendon have been described as two distinct bundles as well as a C or boomerang-shaped tendon surrounding the peroneus longus tendon with central thinning.[8,23-25] In such cases, differentiating between pathologic thinning and the normal flattening in the retromalleolar groove is challenging and likely reflects a continuum of degenerative change.
Given these challenges, there has been wide variation in the reported performance of MRI in diagnosing peroneal tendon tears. In our study, the sensitivities and specificities for the two readers in diagnosing peroneus brevis tears in patients without prior peroneal surgery were 60%/89% and 80%/78%, respectively, comparable with that in literature. The sensitivities and specificities for diagnosing peroneus longus tears in patients without prior peroneal surgery were 25%/92% and 75%/92%. Peroneus longus tears are less common than peroneus brevis tears, with much smaller cohorts in the literature, resulting in fewer and even wider variation in reported MRI performance indicators in the literature, with sensitivities ranging from 20% to 80%.[10,12] Similar MRI findings of peroneus longus tendon tears to peroneus brevis tears have been described.[26,27] More recently, imaging the peroneal tendons in oblique planes has shown potential for improved diagnostic performances compared to traditional orthogonal planes.[6,28] However, utilization may be limited by hardware and/or technical expertise.
We describe a set of novel, objective MRI criteria, named the cleft sign, that could improve the diagnostic performance of readers for peroneal tendon tears. We found that utilizing this sign could significantly increase a reader’s sensitivity and improved the accuracy of both readers to a non-significant degree when used in conjunction with their own reads. Similar to criteria used in the diagnosis of meniscal tears, the cleft sign requires an intermediate to high intrasubstance signal that breaches the tendon surface. Intrasubstance signal on its own can be seen with tendinosis/intrasubstance tearing, but cannot be confirmed on surgery without a surfacing component, a concept well-established with the knee menisci and shoulder rotator cuff.[29,30] The criteria for signal to be present on two contiguous slices improves specificity of the finding by decreasing the effect of partial volume averaging. The cleft sign is reproducible and practical, quickly detected on routine axial T2-weighted sequences, and can be used in situations where oblique-plane imaging sequences may not be readily available.
Our intended use of the cleft sign is to be applied in conjunction with an interpreter’s own read. In cases where a peroneal tendon tear is undoubtedly present, such as in longitudinal split tearing of peroneus brevis with two distinct bundles, the cleft sign need not be assessed and in fact, may not be present. We have found the greatest value from the sign in distinguishing between tendinopathy and partial thickness tears and utilizing the sign can significantly improve sensitivity for diagnosing a tear [Figure 3]. With Reader 1, using the cleft sign for assessment in tendons without prior surgery resulted in two additional false positives. From a practical perspective, as with the assessment of various other musculoskeletal structures, the cleft sign can be falsely identified in peroneal tendons by increasing image contrast with extreme “windowing” and such alterations are strongly discouraged.
The use of the cleft sign is limited in a few situations and must be applied with caution in such instances. In the retromalleolar groove, the peroneus brevis tendon can be quite thinned and in intimate contact with the peroneus longus tendon. This can lead to partial volume averaging effects and difficulties in delineating tendon borders. In addition, we have observed the peroneus longus tendon to variably contain surfacing linear intrasubstance signal distal to the peroneal tubercle, as it courses plantar to the cuboid. We hypothesize that this may be a combination of tendinosis/ tenosynovitis and a natural fanning out morphology before the presence of an os peroneum. Fortunately, in this location, previously designated Zone C, tears of peroneus longus have been found to have a higher proportion of complete ruptures and partial thickness tears are more likely to involve proximal segments.[26] Finally, as expected, we found the cleft sign to be highly unreliable in peroneal tendons that have undergone prior surgery [Figure 5]. Analogous to post-operative meniscus and rotator cuff cases, the presence of intrasubstance signal is non-specific and can represent granulation tissue and/or fibrosis.[31,32] The evaluation of peroneal tendon tears on MRI in the post-operative setting likely requires surfacing fluid-signal to improve specificity, a topic for future research. In challenging clinical cases, further evaluation with ultrasound may add value due to its superior spatial resolution and potential for dynamic assessment.
- A 41-year-old man who had previously undergone peroneus brevis and longus repair with tendon transfer presented with a work-related injury. Second look surgery demonstrated an intact tendon with extensive intratendinous scarring. Consecutive axial T2-weighted fat saturated MR images from superior (a) to inferior (b) of the inframalleolar lateral ankle demonstrate a false positive cleft sign in the peroneus brevis tendon (white arrow).
To look for other markers of tendon injury, Res et al. found significantly higher Goutallier grades of peroneus brevis muscles with tendon tears diagnosed on MRI compared to control groups.[15] However, a limitation of their study was the lack of surgical confirmation of tendon status. We found no significant difference in Goutallier grades for peroneus brevis muscles both within the surgical cohort between proven cases of peroneus brevis tendon tears and no tears as well as overall between the surgical and control groups. Within the rotator cuff, the degree of fatty atrophy significantly correlates with tear size and chronicity, with the highest degrees of fatty atrophy present in chronic massive full-thickness rotator cuff tears.[33] In contrast, our surgical cohort was essentially comprised of only partial thickness tears and muscle quality in larger cohorts of complete peroneal tendon tear cases remains to be determined. Res et al. did not distinguish between partial thickness and full thickness tears in their study. In addition to tendon status, the degree of muscle atrophy is affected by various other factors, including disuse, denervation, and age. Although we controlled for age, we did not account for disuse or denervation in the affected extremity.
Our study is limited by its small sample size and retrospective design, comparable to other similar studies. Given the low number of individual tear types, we limited our analysis in a binary fashion to peroneal tendon tears versus no tears and did not explore the difference in imaging appearance between tendon tears types and other pathologies. We had a large proportion of tendon tears in the surgical cohort, a selection bias that is difficult to avoid without subjecting control patients to unnecessary lateral ankle surgery. Finally, despite excluding cases with excessively long intervals between preoperative MRI and surgery, the intervals in some included cases may still have contributed to false positive or negative MRI reads, potentially related to tendon healing or tearing.
CONCLUSION
Peroneal tendon tears can be challenging to diagnose on MRI, with an overlap in appearance with tendinosis. Application of the cleft sign can significantly increase sensitivity to improve diagnostic accuracy in such cases. We found no significant correlation between the Goutallier grade of the peroneus brevis muscle and the presence of a peroneus brevis tendon tear and the muscle quality likely depends on more complex factors including tear size/chronicity, limb use, and denervation.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21:809-15.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneal tendon tears: A retrospective review. J Foot Ankle Surg. 2003;42:250-8.
- [CrossRef] [Google Scholar]
- Peroneal tendon injuries. J Am Acad Orthop Surg. 2009;17:306-17.
- [CrossRef] [PubMed] [Google Scholar]
- Operative treatment for peroneal tendon disorders. J Bone Joint Surg Am. 2008;90:404-18.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of debridement and primary repair of peroneal tendon tears. Foot Ankle Int. 2014;35:252-7.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the T2-weighted axial oblique MRI sequence in the assessment of peroneal tendons. Clin Radiol. 2020;75:642.e15-23.
- [CrossRef] [PubMed] [Google Scholar]
- Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics. 2005;25:587-602.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging and surgical correlation of peroneus brevis tears. J Foot Ankle Surg. 2004;43:30-6.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of MRI findings of peroneal tendinopathy in patients with lateral chronic ankle instability. Clin Orthop Surg. 2010;2:237-43.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcomes after peroneal tendoscopy in the treatment of peroneal tendon disorders. Knee Surg Sports Traumatol Arthrosc. 2016;24:1148-54.
- [CrossRef] [PubMed] [Google Scholar]
- Is MRI adequate to detect lesions in patients with ankle instability? Clin Orthop Relat Res. 2010;468:1115-9.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative assessment of the peroneal tendons in lateral ankle instability: Examining clinical factors, magnetic resonance imaging sensitivity, and their relationship. J Foot Ankle Surg. 2019;58:208-12.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical results of peroneal tendon repair in a retrospective series of 30 patients. Orthop Traumatol Surg Res. 2018;104:511-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and role of a lowlying peroneus brevis muscle belly in patients with peroneal tendon pathologic features: A potential source of tendon subluxation. J Foot Ankle Surg. 2015;54:872-5.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneal tendon tears: We should consider looking at the muscle instead. J Am Acad Orthop Surg. 2018;26:809-15.
- [CrossRef] [PubMed] [Google Scholar]
- Fatty muscle degeneration in cuff ruptures. Pre-and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83.
- [CrossRef] [Google Scholar]
- Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550-4.
- [CrossRef] [Google Scholar]
- Ultrasound and MRI of the peroneal tendons and associated pathology. Skeletal Radiol. 2013;42:1191-200.
- [CrossRef] [PubMed] [Google Scholar]
- High-resolution US and MR imaging of peroneal tendon injuries. Radiographics. 2015;35:179-99.
- [CrossRef] [Google Scholar]
- Magnetic resonance imaging findings in patients with peroneal tendinopathy and peroneal tenosynovitis. Skeletal Radiol. 2007;36:105-14.
- [CrossRef] [PubMed] [Google Scholar]
- MR features of longitudinal tears of the peroneus brevis tendon. AJR Am J Roentgenol. 1997;168:141-7.
- [CrossRef] [PubMed] [Google Scholar]
- Using MR imaging to differentiate peroneal splits from other peroneal disorders. AJR Am J Roentgenol. 1997;168:129-33.
- [CrossRef] [PubMed] [Google Scholar]
- MRI of peroneal tendinopathies resulting from trauma or overuse. Br J Radiol. 2013;86:20110750.
- [CrossRef] [PubMed] [Google Scholar]
- Characterization of patients with primary peroneus longus tendinopathy: A review of twenty-two cases. Foot Ankle Int. 2000;21:462-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tear of the peroneus longus tendon: MR imaging features in nine patients. Radiology. 2000;214:700-4.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneal tendon pathology evaluation using the oblique sagittal plane in ankle MR imaging. Acta Radiol. 2016;57:620-6.
- [CrossRef] [PubMed] [Google Scholar]
- MR of the knee: The significance of high signal in the meniscus that does not clearly extend to the surface. AJR Am J Roentgenol. 1991;156:333-6.
- [CrossRef] [PubMed] [Google Scholar]
- Glossary of terms for musculoskeletal radiology. Skeletal Radiol. 2020;49:1-33.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging the postoperative knee meniscus: An evidence-based review. AJR Am J Roentgenol. 2018;211:519-27.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder after rotator cuff repair: MR imaging findings in asymptomatic individuals--initial experience. Radiology. 1999;213:705-8.
- [CrossRef] [PubMed] [Google Scholar]
- Muscle fatty infiltration in rotator cuff tears: Descriptive analysis of 1688 cases. Orthop Traumatol Surg Res. 2009;95:319-24.
- [CrossRef] [PubMed] [Google Scholar]






