Translate this page into:
Extensor Hallucis Longus Tendonitis: A Rare Cause of Dorsal Midfoot Pain

*Corresponding author: Debasish Jena, Department of Physical Medicine and Rehabilitation, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. debasish.mbbs@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jena D. Extensor Hallucis Longus Tendonitis: A Rare Cause of Dorsal Midfoot Pain. Indian J Musculoskelet Radiol 2021;3(1):64-6.
Abstract
Although disorders of tendon are quite common, acute extensor hallucis longus (EHL) tendonitis is a very rare occurrence. Repeated friction across the top of the foot or excessive pressure from an ill-fitting shoe is among most common risk factors. We report a 59-year-old lady with acute EHL tendonitis where musculoskeletal ultrasound appears to be an effective choice for both diagnosis and for guiding corticosteroid injection into tendon sheath.
Keywords
Tendinopathy
Tendonitis
Foot pain
Musculoskeletal ultrasound
INTRODUCTION
Primary disorders of tendons are common and account for a high proportion of referrals to physiatrists and orthopedic surgeons. The most commonly involved tendons are the rotator cuff (particularly supraspinatus) and biceps brachii tendons in the shoulder, the forearm extensor and flexor tendons in the forearm, the patellar tendon in the knee, the Achilles tendon in the distal leg, and the tibialis posterior tendon in the ankle and foot.[1] Tendinopathy of the extensor hallucis longus (EHL) tendon is extremely rare and literatures depicting its diagnosis and treatment are scarce.
CASE REPORT
A 59-year-old lady from Purba Medinipur in West Bengal presented with chief complaints of acute pain and swelling over dorsum of her right midfoot for the past 10 days along with difficulty in walking. There was no history of any local trauma or any previous long-term illness. She gave a history of occasional rubbing of the strap of her footwear over the affected area. She is a housewife with no history of any sudden change of activity or any history of uphill walking. On inspection, the skin over the dorsum of the first metatarsal was tense and shiny depicting definite swelling and EHL tendon was not appreciable compared to the normal side [Figure 1]. On palpation, there was Grade III tenderness and the resisted dorsiflexion test for the great toe was positive. At presentation, her visual analog scale pain (VAS) score was 8.

- At presentation: Right foot showing tense and shiny skin over extensor hallucis longus tendon with swelling of overlying area (arrow).
Routine blood investigations revealed no apparent abnormalities. Radiographs of her right foot were normal and ruled out any stress fractures, calcific tendonitis, or any other bone pathology. Ultrasonography (USG) of the affected part showed anechoic area in the EHL tendon sheath along with thickening of the tendon compared to normal side, thereby confirming our diagnosis of EHL tendonitis [Figures 2 and 3].
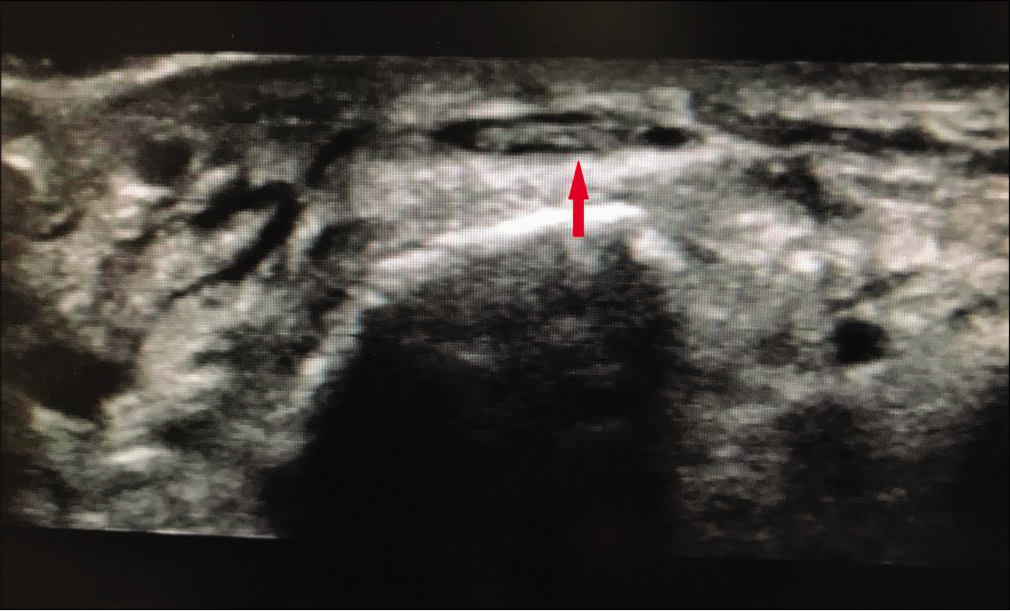
- Ultrasonography image taken in short-axis showing obvious anechoic area surrounding extensor hallucis longus tendon (arrow) suggestive of inflammation.
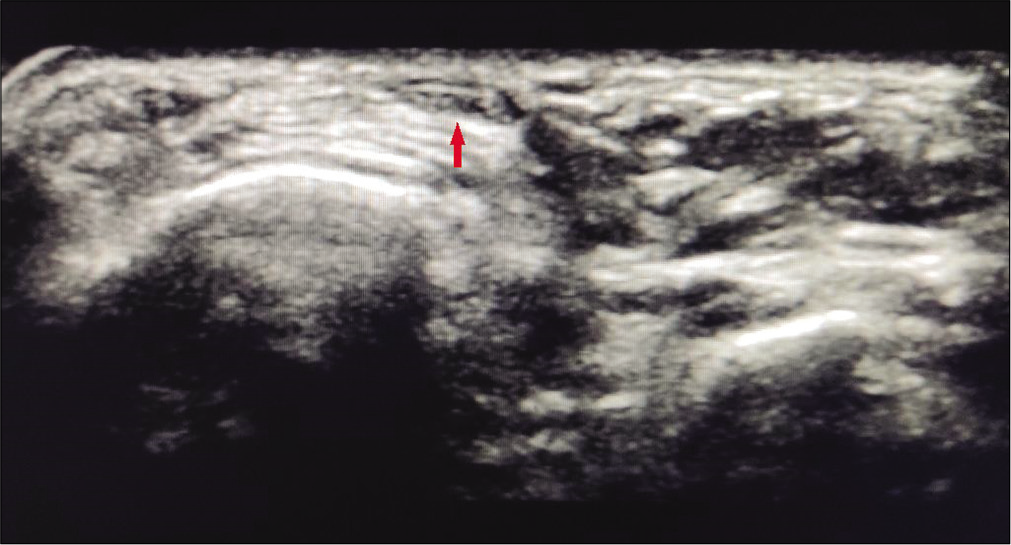
- Ultrasonography image of opposite foot showing a healthy extensor hallucis longus tendon with normal echotexture and echogenicity (arrow).
On her first visit, she was advised relative rest to the foot, ice application 2–3 times daily, and a short course of nonsteroidal anti-inflammatory drugs (NSAIDs) for 7 days. She was advised to use larger size footwear to avoid irritation of the EHL tendon. She visited after 1 week with persistent pain and swelling with a VAS score of 6. Under USG guidance, 1 ml triamcinolone acetonide (40 mg) and 0.5 ml lignocaine (2%) solution were injected into the tendon sheath. No post-procedural complications were reported.
She further visited our outpatient department 6 weeks post-injection. On examination, there was no swelling and EHL tendon was easily appreciable [Figure 4] with Grade 0 tenderness. The resisted dorsiflexion test was negative and the VAS score was 0. She was taught with eccentric training of EHL to regain previous strength, along with stretching exercises for gastrosoleus and footwear modification to prevent undue pressure over the tendon. A gradual return to previous activity level was advised. At 12 weeks post-injection, the treatment effect was persistent with no signs of recurrence.

- After intervention: Extensor hallucis longus tendon easily appreciable (arrow) with no signs evident of inflammation.
DISCUSSION
The most important cause of midfoot pain is tibialis anterior tendinopathy but the pain here localizes to front of the ankle rather than top of midfoot. Other causes include navicular stress fracture, midtarsal joint sprain, Morton’s neuroma, and Lisfranc injury.[2] In Morton’s neuroma, pain typically occurs between the 3rd and 4th metatarsal with a positive Mulder’s sign. In our patient, localization of pain and tenderness over EHL tendon with a normal radiograph ruled out all the above conditions. Although calcific tendonitis of EHL has been reported in the past,[3] this is the first case of acute EHL tendonitis reported to our knowledge in the literature. The mechanism of injury for a particular tendinopathy can vary across geographical regions and from patient to patient with tensile overloading being the dominant mechanism. Risk factors can be extrinsic or intrinsic.[4] Extrinsic factors may include training errors, excessive loading, environmental factors like temperature (e.g., the tendon gets stiffer in cold weather which reduces its circulation), or a direct external injury. Typically, extensor tendonitis of foot develops due to repeated friction across the top of the foot or excessive pressure from an ill-fitting shoe. Intrinsic factors may include individual biomechanics (malalignments, muscle weakness or imbalance, and decreased flexibility), age, and adiposity. For EHL tendonitis, factors such as tightness of calf muscles and abnormal foot arches are of particular importance. Furthermore, medical conditions such as rheumatoid arthritis and diabetes mellitus may predispose to tendinopathies. Diagnosis is mainly clinical and USG confirms the diagnosis. Initial management should focus on rest to the affected tendon, ice application, short course of NSAIDs, and most importantly eliminating the trigger. An ill-fitting footwear as an etiologic factor should be ruled out in every case. Soft insoles and shoe inserts can be used to provide padding and support to the foot, taking any undue tension off the tendons. If conservative management fails, USG-guided corticosteroid injection into the tendon sheath appears to be an effective treatment. Care must be taken to avoid intratendinous corticosteroid injection as it may worsen the condition and lead to a tendon rupture. After pain and swelling subsides, the patient should be advised with eccentric training of EHL to regain previous strength. Gastrosoleus stretching should be advised as calf tightness is considered an important risk factor. Activity modification includes avoidance of the extrinsic trigger, for example, an ill-fitting shoe, walking over uneven surfaces or walking uphill, etc., followed by a gradual return to normal activity. Rehabilitation strategies emphasizing individualized biomechanics and overall movement/function have recently been validated in large randomized controlled trials, underlining the potential importance of biomechanics in the etiology of tendinopathy.[5,6]
CONCLUSION
EHL tendonitis is a rare but important cause of top of foot pain. Musculoskeletal USG appears to be an effective diagnostic tool and can be used further for guiding injection into tendon sheath. Rehabilitation programs should be individualized and emphasized on proper biomechanics, prevent training errors and footwear modifications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pathogenesis of tendinopathies: Inflammation or degeneration? Arthritis Res Ther. 2009;11:235.
- [CrossRef] [PubMed] [Google Scholar]
- Foot pain In: Brukner P, Khan K, eds. Clinical Sports Medicine (4th ed). New York: McGraw-Hill; 2012. p. :844-77.
- [Google Scholar]
- Extensor hallucis longus calcific tendonitis: A case report. Foot Ankle Int. 2006;27:144-45.
- [CrossRef] [PubMed] [Google Scholar]
- Tendinopathy: Update on pathophysiology. J Orthop Sports Phys. 2015;45:833-41.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: Randomised controlled study. Br J Sports Med. 2014;48:1456-7.
- [CrossRef] [PubMed] [Google Scholar]
- Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Man Ther. 2001;6:205-12.
- [CrossRef] [PubMed] [Google Scholar]






