Translate this page into:
Imaging insights into inflammatory and infective arthritis of the hip joint

*Corresponding author: Madhavi Kandagaddala, Department of Radiology, Christian Medical College, Vellore, Tamil Nadu, India. madhoo116@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mathew BB, Mathew AS, Joseph KT, Abraham VJ, Kandagaddala M, Chari R. Imaging insights into inflammatory and infective arthritis of the hip joint. Indian J Musculoskelet Radiol. 2025;7:26-40. doi: 10.25259/IJMSR_73_2024
Abstract
A diverse array of inflammatory conditions can impact the hip joint, including septic arthritis, crystal arthropathies, and the involvement of the hip joint in the context of inflammatory polyarthritis. Given the significant overlap in clinical presentations and the complexities associated with physical examinations and laboratory investigations, imaging emerges as a critical tool for accurate diagnosis. It aids in detecting subclinical disease, evaluating disease activity, and informing therapeutic decisions. This article aims to offer a comprehensive overview of the prevalent inflammatory and infectious arthritis affecting the hip joint. It will detail specific imaging modalities and elucidate the integral role of radiologists in this diagnostic process. Furthermore, the discussion will present a methodical approach to assessing patients with inflammatory hip pain, addressing potential conditions that may mimic inflammatory and infectious arthritis of the hip joint.
Keywords
Hip joint infection
Hip joint inflammation
Magnetic resonance imaging
Ultrasound
INTRODUCTION
The hip joint is a weight-bearing, synovial, and ball-and-socket joint that is highly congruent and stable yet allows for a wide range of motion. The joint is formed by a rounded femoral head (ball) articulating with a hemispherical acetabular fossa (socket), which is lined by articular hyaline cartilage, fibrocartilaginous acetabular labrum, joint capsule, and extra-articular ligaments, tendon, and bursae.
Inflammation within the hip joint may affect any of the components of the joint and can be due to infectious and non-infectious causes.[1] Due to its deep location and the wide range of pathologies that affect it, it is challenging to examine clinically and to localize the cause of pain.[2]
This article aims to highlight the role of imaging in evaluating the various inflammatory/infective pathologies affecting the hip joint.
IMAGING MODALITIES
Radiographs remain the standard first-line modality of evaluation. The anteroposterior (AP) view of the pelvis and both hips is the standard initial examination, while dedicated views such as the cross-table lateral, frog-leg lateral, or Dunn lateral may be performed for the symptomatic hip. The radiograph has an irreplaceable role in assessing bone density and structure, joint integrity, erosive lesions, and extraosseous calcifications. All of these play a significant role in narrowing the differentials of hip joint arthritis. Ultrasound (USG) can detect joint effusion, assess for synovial thickening, and guide joint fluid aspiration. Ultrasound may be used to look for evidence for crystal deposition and evaluation of the periarticular soft tissues. The addition of Doppler provides valuable information about the disease activity by detecting synovial hyperemia. However, despite several advantages of USG, due to the lack of standard imaging protocols, high operator dependence, and often suboptimal acoustic window availability, magnetic resonance imaging (MRI) is generally the modality of choice in hip joint evaluation.
According to the American College of Radiology, Musculoskeletal Imaging Criteria,[3] MRI is advocated as the next line of imaging for all chronic hip pain patients with negative radiographs.
MRI has superior resolution and great utility, particularly in assessing bone marrow, acetabular labrum, cartilage, and periarticular soft tissue. The decision to use intra-venous Gadolinium-based contrasts to enhance MRIs remains debatable.
Computed tomography (CT) usually only has a limited role as a problem-solving tool for better characterizing bony structures and lesions.
We will discuss the inflammatory hip joint pathologies under four broad categories:
Hip joint involvement in the setting of inflammatory polyarthritis
Predominant hip joint involvement presenting as a pauci-arthritis
Mono-arthritis and infections
Mimics and otherwise-non-specified conditions.
CATEGORY I: HIP INFLAMMATION AS PART OF POLYARTHRITIS SETTING
Juvenile idiopathic arthritis (JIA)
JIA is the most common chronic arthritis of childhood, and symptoms must start before 16 years of age. It affects approximately 16–150 children per 100,000 annually, and the female-male ratio is 2:1.[4-6]
JIA does not primarily affect the hip joint except in the “entheseal-related arthritis” (ERA) subtype of JIA [Figure 1]. Both hips are frequently involved in the ERA subtype of JIA, and 30% have sacroiliitis.
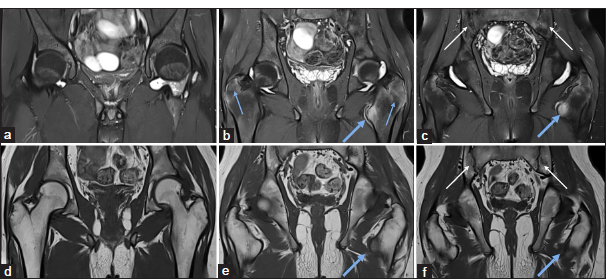
- (a-f) A 15-year-old child with a known case of juvenile idiopathic arthritis (JIA) presented with a recent onset of worsening pain. (a-c) Magnetic resonance imaging pelvis - short-tau inversion recovery coronal and (d-f) T1-weighted coronal images demonstrate moderate left hip joint synovitis and effusion and mild right hip joint synovitis and effusion. There is chronic bilateral inflammatory sacroiliitis (white arrows in c and f), significant enthesitis at the left iliopsoas tendon with associated bone marrow edema in the lesser trochanter (thick blue arrow in b,c,e and f), and mild enthesitis at the bilateral greater trochanter (thin blue arrow in b), suggests entheseal related arthritis subtype of JIA.
Although the hip is not the primary joint affected at the time of diagnosis, hip joint involvement is a marker that heralds future disability. A cohort of JIA patients showed a threefold increase in cases with hip involvement over a 5-year follow-up period despite being on medication.[7] Most children can develop irreversible changes within 5 years of diagnosis, and 26–44% of patients will require total hip replacement within the first 10 years of disease onset in the absence of appropriate treatment.[8,9] However, the increasing use of biological agents that prevent rapid destruction has stimulated the need for imaging modalities that are more sensitive in detecting preerosive early inflammatory changes.
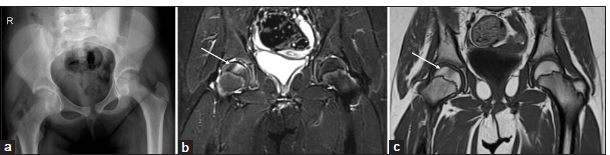
Although historically, radiography has been one of the main imaging techniques used to diagnose JIA, it now primarily serves as a baseline standard for follow-up. Entheseal inflammation of the ligamentum teres with resultant foveal widening on the radiograph is a characteristic feature of JIA [Figure 2].
- (a-d) An 8-year-old child with right hip pain for 6 months. (a) Anteroposterior radiograph of the pelvis shows mild juxtaarticular osteopenia on the left side. (b) Ultrasound of the hip joint showed mild synovitis (thin white arrows) in the right hip joint, and the left hip joint was unremarkable. (c) Magnetic resonance imaging pelvis - short-tau inversion recovery coronal and (d) T1-weighted coronal images demonstrate mild to moderate synovitis in the right hip joint (blue arrow in c) and minimal synovitis in the left hip joint with widening of the bilateral foveal (short white arrows in c and d) which suggests erosion and is a classical feature of inflammatory arthritis.
In a known case of JIA, conventional radiographs provide insight into the natural course of the disease, joint damage (joint space reduction and bone erosions), growth disturbances due to a decrease in bone mineral density, epiphyseal enlargement and early physeal closure, and degenerative features such as ankylosis and joint malalignment.
MRI forms the mainstay of early disease detection and evaluation of disease response to treatment. MRI has the distinct ability to identify bone marrow edema, considered a pre-erosive abnormality, and an indication for initiating therapy to prevent irreversible joint damage [Figures 3 and 4]. Synovial inflammation and bone marrow edema in asymptomatic joints of JIA patients have been identified as predictors of relapse and disease progression.
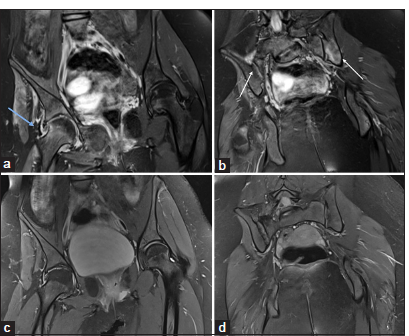
- (a-b) A 10-year-old child, a known case of juvenile idiopathic arthritis, presented with a recent onset of worsening hip pain. (a) Magnetic resonance imaging pelvis - short-tau inversion recovery coronal and (b) T1-weighted coronal images demonstrate mild synovitis in the bilateral hip joint, focal bone marrow edema-like signal in the left femoral head (blue arrow in a and b), which is considered pre-erosive abnormality. There is also a widening of the bilateral fovea (short white arrow in a and b) and a widening of the bilateral acetabular notch (thin white arrow in a and b), a classical imaging feature of inflammatory arthritis.
- (a-d) A 14-year-old child with a known case of juvenile idiopathic arthritis presented with a recent onset of worsening hip pain. (a) Initial magnetic resonance imaging (MRI) pelvis - short-tau inversion recovery (STIR) coronal and (b) T1-weighted coronal images demonstrate mild synovitis and effusion in the left hip joint and focal bone marrow edema-like signal in the left femoral head (white arrow in a and b) and progress to definite erosion (blue arrow in c and d) as seen in the follow-up MRI’s (c) STIR and (d) T1W coronal images.
Several MRI scoring systems have been proposed for evaluating juvenile hip arthritis;[10-14] however, there is currently no validated MRI scoring system for evaluating the hip joints in JIA.[15] The JIA outcome measures in rheumatoid arthritis clinical trials (OMERACT) working group published a methodological study in 2021 that standardized the whole-body MRI scoring system, including the hip joint, for evaluating disease activity in JIA.[16] As there are currently no well-established imaging protocols for follow-up of JIA patients, the timing and utilization of follow-up imaging in JIA must be tailored to the individual patient.
Rheumatoid arthritis (RA)
RA is an adult-onset chronic inflammatory disease characterized by persistent synovial inflammation leading to joint destruction. Like JIA, the hip joint may be affected in only 15–28% of all cases of RA and is rarely the primary joint involved.[17] Characteristic clinical features are the presence of early morning stiffness and pain lasting for several weeks; stiffness is more after inactivity with symmetric and multiple joint involvement. Imaging features depend on the disease duration and stage of the disease. Radiographs are often normal in the early stages of the disease. MRI helps detect synovial hypertrophy, effusion, and bone marrow edema. As the disease progresses, erosions can be easily identified on radiographs and MRIs. In advanced stages, osteopenia and joint space narrowing are observed, which are concentric [Figure 5] (in contrast to osteoarthritis, which frequently results in superolateral, weight-bearing joint space loss and is associated with subchondral sclerosis).[18] With the progression of the disease, medial and/or superior migration of the femoral head with protrusio acetabuli can occur. The end-stage disease can result in joint ankylosis, especially in the young-onset variant.
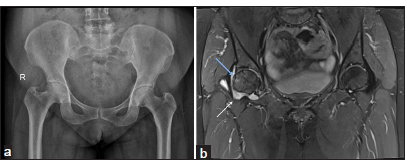
- A 40-year-old lady with right hip pain and stiffness. (a) An anteroposterior pelvis radiograph shows a narrowing of the right hip joint space. (b) Magnetic resonance imaging pelvis - short-tau inversion recovery coronal image show synovitis and effusion with erosions and subtle bone marrow edema (blue arrow).
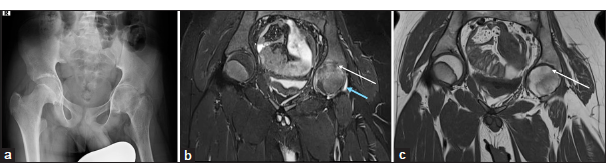
Spondyloarthritis (SpA)
SpA is a group of inflammatory diseases that include ankylosing spondylitis (AS), reactive arthritis, psoriatic arthritis, juvenile SpA, SpA-associated inflammatory bowel disease, and undifferentiated SpA.[19] About one-third of cases of AS involve the hip joint.[20] Reactive arthritis and psoriatic arthritis are less likely to impact the hip joint; however, when they do affect the hip, asymmetrical sacroiliac joint (SI) joint involvement is a key differentiating finding. In psoriatic SpA, entheseal site involvement is a prominent feature [Figure 6]. Patients with extensive active axial disease, entheseal, and early age-onset illnesses may have more severe hip involvement.[21,22] Chronic pain brought on by an acute inflammation of the synovitis or capsulitis is the usual sign. When the patient experiences significant hip discomfort, the damage is typically extensive. Hip replacement is currently the only viable treatment. After hip arthroplasty, nearly 90% of patients will report reduced pain and increased range of motion.[23,24] In the early stages, synovial hypertrophy, effusion, and bone marrow edema are frequent imaging findings better visualized in MRIs. As the disease progresses, both the radiographs and MRI demonstrate erosions, joint space narrowing, and ankylosis [Figure 7].
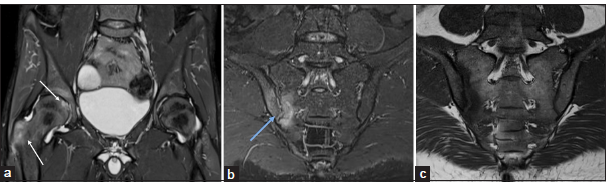
- (a-c) A 30-year-old male known case of psoriasis with inflammatory low back and hip pain. (a) Magnetic resonance imaging pelvis - short-tau inversion recovery (STIR) coronal image shows bilateral hip joint synovitis and effusion with active enthesitis at the right greater trochanter and the ligamentum teres attachment at the fovea (white arrows). (b and c) STIR oblique and T1 oblique coronal images of the sacroiliac joints demonstrate articular surface erosions and bone marrow edema (blue arrow) on the right side, and the left sacroiliac joint is unremarkable. These imaging features of asymmetric sacroiliitis and enthesitis suggest psoriatic spondyloarthropathy.
- 28-year-old lady with inflammatory low back and hip pain. (a) Anteroposterior pelvis radiograph shows diffuse osteopenia, bilateral hip joint space narrowing and erosions, and also subchondral sclerosis of bilateral sacroiliac joints. (b) Magnetic resonance imaging pelvis - short-tau inversion recovery (STIR) coronal image shows significant bilateral hip joint synovitis and effusion (short white arrows). (c and d) T1-weighted oblique and STIR oblique coronal images of the SI joints demonstrate bilateral articular surface erosions with juxta-articular fatty marrow replacement (blue arrow) and bone marrow oedema (yellow arrows). (e) STIR oblique axial image shows active enthesitis of paraspinal muscles (thin white arrow).
Role of the radiologist
The role of the radiologist may thus be considered three-fold in the evaluation of the symptomatic hip joint in the setting of an inflammatory polyarthritis setting:
Assist in establishing the diagnosis
Ascertain the cause of pain in an acutely symptomatic patient
Stage the disease and assist in treatment escalation/de-escalation.
While the first involves appreciating key radiological findings of inflammation, the latter two are interrelated and include assessing disease activity and differentiating disease flare-ups from other causes of acute pain or complications of the disease process.
In establishing the diagnosis, radiographs are limited in detecting early bone structural and soft-tissue changes. Ultrasound is a good tool for assessing synovial thickness, joint effusion, cartilage thickness, and erosions, as well as guiding diagnostic and therapeutic procedures. Doppler can also detect subclinical synovitis and disease activity by detecting synovial hyperemia.
MRI is the mainstay for detecting early inflammatory changes such as erosive changes, pre-erosive bone marrow edema, synovitis, and joint effusion even before they appear at physical examination. Early disease detection is essential for the timely initiation of disease-modifying agents and preventing permanent structural damage.
Determining abnormal or significant joint effusion may sometimes be challenging as a small amount of fluid within the joint capsule may be within normal limits; studies that provide absolute quantification of these parameters on MRI are lacking and still require subjective judgment by an experienced radiologist. Gadolinium-based contrast-enhanced T1-weighted sequences help to differentiate effusion from synovitis and to assess synovial enhancement and thickening.[25] Recent studies have highlighted the potential adverse effects of gadolinium and prohibited several linear-gadolinium-based contrast agents due to the reported gadolinium depositions in the brain.[26,27] Vo Chieu et al. showed that unenhanced MRI comprising proton-density-weighted sequences can detect disease activity in patients with JIA with equally high accuracy compared to contrast-enhanced MRI.[28] Recently, Panwar et al. considered “effusion/synovial thickening” as a single term, as it is often difficult to differentiate on non-contrast images.[16]
MRI helps to determine the cause of worsening pain due to active disease, evident as synovitis and effusion, or due to structural changes, and decide on treatment escalation; it is essential to differentiate inflammatory disease progress from structural changes and complications secondary to the disease process [Figure 8].
- A 15-year-old child with a known case of juvenile idiopathic arthritis presented with a recent onset of worsening hip pain. (a) An anteroposterior pelvis radiograph shows a narrowing of the bilateral hip joint space and erosions in the left femoral head and (b) Magnetic resonance imaging pelvis - short-tau inversion recovery (STIR) coronal image clearly demonstrates active disease evident as moderate joint effusion and synovitis (white arrows) and structural changes evident as erosions (blue arrows).
The end stage of any inflammatory joint pathology is chronic structural damage, which includes osteochondral changes, bone erosions, joint space narrowing, and ankylosis. Inflammatory and structural damage changes can co-exist depending on the duration and course of the disease [Figure 9]. Inflammatory arthritis patients also have an increased risk of fracture of the femoral neck and intertrochanteric fractures, likely related to periarticular osteopenia that are associated with both the disease and its treatment with corticosteroids[29] [Figure 10].
- A 15-year-old child with a known case of juvenile idiopathic arthritis. (a and b) Initial magnetic resonance imaging pelvis – short-tau inversion recovery (STIR) coronal images demonstrate active disease evident as mild right hip joint synovitis (blue arrow in a) and bone marrow edema and synovitis in bilateral sacroiliac joints (white arrows in b). (c and d) The follow-up MRI’s STIR coronal images after a course of biologics show complete resolution of synovitis and bone marrow edema.
- (a-e) A 14-year-old child with a known case of juvenile idiopathic arthritis presented with a recent onset of right hip pain. (a) An anteroposterior pelvis radiograph shows bilateral hip joint space narrowing and juxta-articular osteopenia; these changes are more pronounced on the right side. (b) Initial magnetic resonance imaging pelvis – short-tau inversion recovery (STIR) coronal image demonstrates mild right hip joint synovitis and severe bone marrow edema in the right femoral head (blue arrow). (c) The corresponding T1-weighted coronal image shows insufficiency fractures (white arrow). (d and e) After a course of conservative management, the follow-up MRI’s STIR and T1W coronal images show complete resolution of insufficiency fracture and bone marrow edema.
CATEGORY II – PREDOMINANT HIP JOINT INVOLVEMENT IN A PAUCI- ARTHRITIS SETTING
This category mainly includes crystal arthropathies.
Crystal arthropathies
Hydroxyapatite crystal deposition disease (HADD)
HADD or calcific tendinitis is characterized by intra- or periarticular deposition of hydroxyapatite crystals and should be included in the differential diagnosis for hip pain. After the shoulder, the hip is the second most frequently involved site (5–15% of patients with HADD).[30] Radiographs can detect the deposits if they are calcified. MRI shows hypointense deposits within the affected tendons and periarticular structures with significant adjacent soft-tissue edema in the acute phase [Figure 11]. CT is sensitive for detecting hydroxyapatite deposits, and a comet-tail appearance is characteristic. The Hounsfield units (HU) measurement for hydroxyapatite deposits is around 100–400 HU, which is useful to differentiate from more dense bony fragments seen in the cases of avulsion injuries or heterotopic ossification.[31]
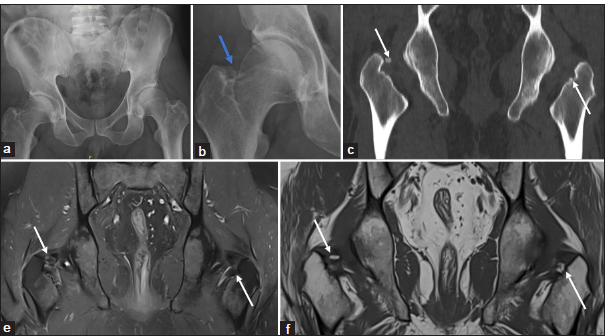
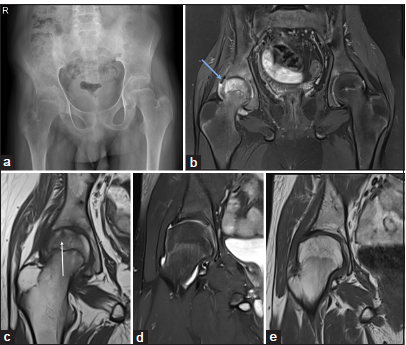
- A 40-year-old man with right hip pain. (a) The anteroposterior radiograph of the pelvis and the (b) magnified radiograph shows a calcified focus along the inner surface of the right greater trochanter (blue arrow). (c) The computed tomography coronal and (d) magnetic resonance imaging pelvis - short-tau inversion recovery coronal and (e) T1-weighted coronal images show a calcific deposit in the bilateral obturator internus tendons (white arrows in c-e) suggest calcific tendonitis. No calcifications, significant effusion or synovitis in the bilateral hip joints.
Calcium pyrophosphate deposition disease (CPPD)
CPPD, also termed “pseudogout,” is an arthropathy caused by the deposition of calcium pyrophosphate dihydrate crystals in the articular tissues, most commonly fibrocartilage (labrum) or even the hyaline articular cartilage as well as periarticular tissue.[32] CPPD is considered a great mimic due to its varied clinical presentation, which overlaps with multiple other arthropathies.[33]
The diagnosis is established by the detection of calcium pyrophosphate (CPP) dihydrate crystals in synovial fluid aspirate and the detection of calcification within articular cartilage.[34]
Imaging features, in addition to early or atypical degenerative arthritis-like features, include the detection of calcification along the labral fibrocartilage or the hyaline articular cartilage. Calcification within the cartilage may be detected by radiograph or USG. MRI does not have specific features; however, it plays a key role in excluding other differentials.
Gouty arthritis
Gouty arthritis rarely affects the hip joints, likely due to the lack of temperature variability and pH required for sedimentation of the monosodium urate crystals.[35] Hadler et al. reported that only 1–2% of patients with acute polyarticular gout had involvement of the hip joints.[36] Imaging features are only specific if bony erosions have protruding edges, sclerotic margins, or soft-tissue tophi. Prior studies report 3–18% of gouty arthritis patients having SI joint involvement [Figure 12]. Ultrasound may reveal crystal deposition over the femoral head cartilage – double contour sign and detect effusion and synovitis.[37]

- Gouty sacroiliitis – (a and b) magnetic resonance imaging of sacroiliac joints - T1-weighted and short-tau inversion recovery oblique coronal of the SI joints demonstrate articular surface erosions with subtle bone marrow edema and hypointense soft tissue in the left SI joint (white arrow). (c) Computed tomography axial sections demonstrate a high-dense soft tissue with deep excavating articular surface erosions with a sclerotic margin and overhanging edges along the iliac side of the posterior aspect of the inferior part of the left sacroiliac joint. No joint space narrowing (white arrow).
CATEGORY III – MONO-ARTHRITIS AND INFECTIONS
Infective arthritis
Infective or septic arthritis is an emergency that requires prompt diagnosis and management. It is more common in children than adults, and the hip is the most affected joint.[38] Delayed recognition and treatment of septic arthritis of the hip joint (SAH) can result in severe complications, including avascular necrosis of the femoral head, osteomyelitis, chondrolysis, hip dislocation, leg-length discrepancy, systemic sepsis, and future osteoarthritic degeneration.[39] Hematogenous spread is the most frequent source, and direct inoculation by trauma is rare. The common causative agent is Staphylococcus aureus, followed by methicillin-resistant Staph aureus, Streptococcus species, mycobacteria, and rarely Kingella kingae, fungi, and viruses.[40] Salmonella species is common in infective arthritis of the hip joint in children with sickle cell anemia. Male gender, previous trauma, immunocompromised status, and children under the age of three are risk factors for the development of septic arthritis. The typical clinical presentation is hip pain and limp. A prompt clinical diagnosis can be challenging as an absence of fever, normal leukocyte count, and negative C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), cannot be used to rule out septic arthritis.[40] Therefore, clinical suspicion must remain high in any child presenting with acute hip pain and/or inability to bear weight.
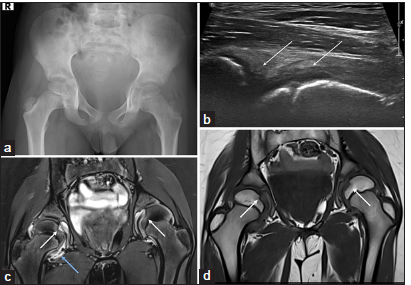
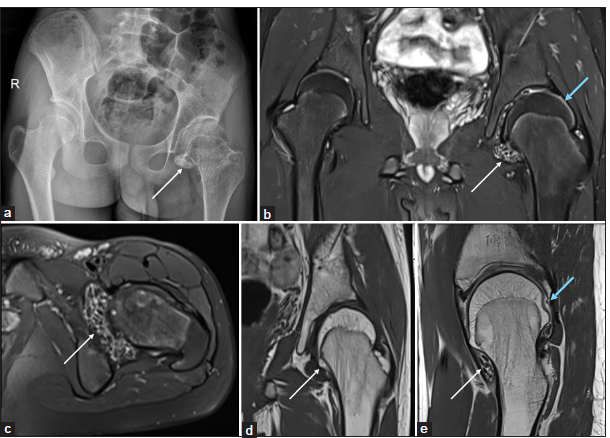
Standard radiographs are limited in evaluating and diagnosing patients with possible septic arthritis. It takes substantial time (at least 10–14 days) for radiographic visualization of associated osseous changes. Similarly, evidence of joint space asymmetry or widening due to a hip effusion generally may not be evident initially [Figure 13]. Widening of the physis indicates co-existing osteomyelitis and may be seen on the radiograph. However, it is better delineated on other modalities [Figure 14]. Ultrasound is a more widely applicable imaging modality in patients with suspected SAH. The presence of effusion within the affected hip joint, when compared with the asymptomatic side, is strong evidence that further evaluation is required for the pediatric patient with suspected SAH. In addition, ultrasound may be utilized as a guide for diagnostic aspiration of the joint fluid.
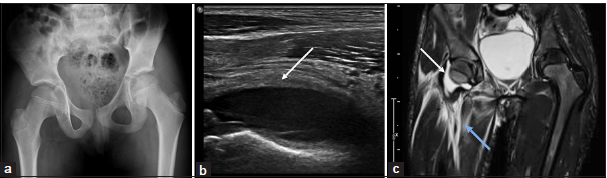
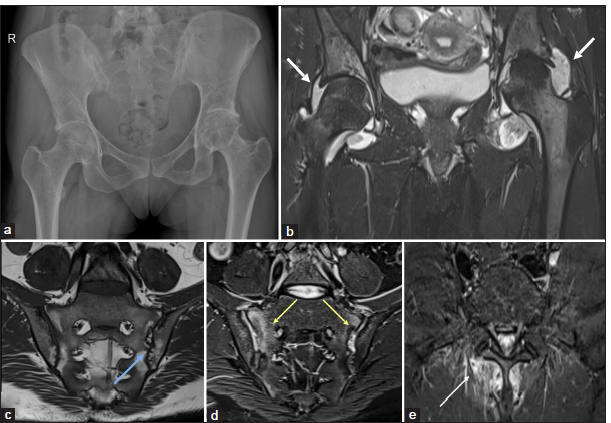
- A 14-year-old child with acute onset right hip pain and restricted movements. (a) Anteroposterior pelvic radiograph appears normal except for a mild pelvic tilt to the right side which could even be positional. (b) Ultrasound of the hip joint showed significant right hip joint effusion (white arrow) with distension of the capsule and (c) magnetic resonance imaging of pelvis – short-tau inversion recovery (STIR) coronal image show effusion (white arrow) and ill-defined edema along the myofascial planes of the proximal thigh (blue arrow) suggesting infective arthritis.
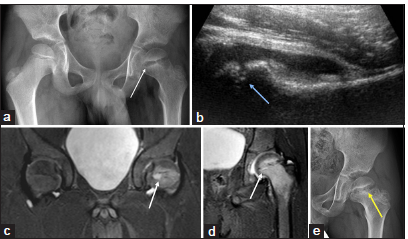
- A 9-year-old child with left hip pain. (a) Anteroposterior pelvic radiograph shows a widening of the left physis (thin white arrow) and osteopenia of the left proximal femur. (b) Ultrasound of the left hip joint shows effusion and widening of the peripheral physis (blue arrow). (c and d) Magnetic resonance imaging of pelvis – short-tau inversion recovery coronal images clearly demonstrate a small abscess in the proximal femoral physis (short white arrows in c and d) with the resultant widening of the physis and associated adjacent bone marrow oedema and hip joint effusion suggesting co-existing osteomyelitis and infective arthritis. (e) The follow-up anteroposterior pelvic radiograph of the pelvis demonstrates focal bony physeal bars in the proximal left femur (yellow arrow).
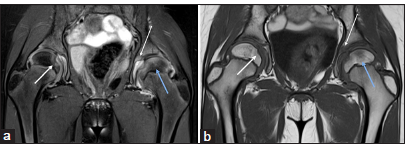
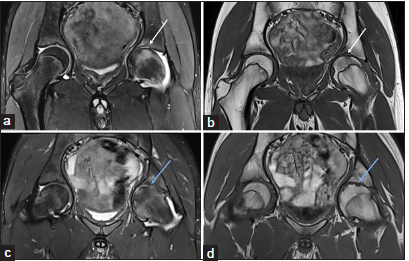
MRI improves the diagnostic efficiency in patients with SAH. MRI in pediatric patients often requires sedation, and, in some cases, MRI itself is not routinely available in an emergency. Hence, MRI has been reserved for those patients with signs and symptoms of SAH but who may have a negative hip ultrasound or a hip aspiration that is inconsistent with acute infection to assess the concomitant periarticular osteomyelitis and the status of the articular cartilage and avascular necrosis. One of the characteristic features of septic arthritis is the presence of joint effusion and edema of the peri-articular soft tissues [Figure 13]. On MRI, the thickened synovium caused by the perivascular inflammatory infiltrate is easily visible, and the vascularized granulation tissue may appear as a hyperintense rim on T1-weighted (T1W) images and may show contrast enhancement [Figure 15]. A more distinctive characteristic feature is the presence of collections in the periarticular soft tissues. Marrow edema beyond the subchondral bone into the medullary cavity and diffuse low signal on T1W images suggest possible osteomyelitis. MRI can assess the status of the articular cartilage since septic arthritis causes rapid erosions. In later stages, large erosions and frank bone destruction may occur [Figure 16].
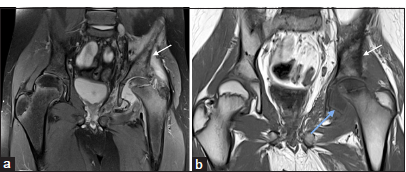
- A 12-year-old child with left hip infective arthritis. (a and b) Magnetic resonance imaging of pelvis – short-tau inversion recovery coronal image shows moderate left hip joint effusion with synovitis, which appears as a hyperintense rim on T1-weighted coronal image (blue arrow), suggesting vascularised granulation tissue. There is a widening of the proximal femur physis and a poorly defined bone marrow edema-like signal in the left proximal femur and ilium, which appears hypointense on T1-weighted images (white arrow in a and b); this suggests coexisting osteomyelitis.
- (a-c) A 40-year-old lady with left hip pain and restricted movements. (a) Anteroposterior pelvic radiograph shows a defect (yellow arrow) in the medial wall of the left acetabulum and increased soft tissue opacity in the peri-acetabular region. (b and c) Magnetic resonance imaging of pelvis – short-tau inversion recovery coronal and axial images show significant left hip joint effusion, bone marrow edema in the acetabulum with a defect in the medial acetabular wall (yellow arrow), suggests septic arthritis with osteomyelitis and extensive collections and edema in the obturator internus muscle extending to the anterior subcutaneous plane.
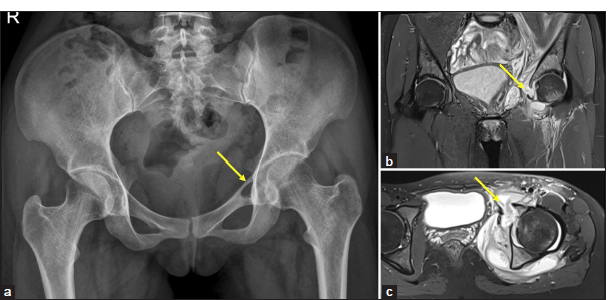
Distinguishing between septic arthritis and transient synovitis of the hip joint can be challenging, necessitating the use of validated diagnostic criteria and a multidisciplinary approach. The clinical presentations of septic arthritis and transient synovitis are similar to each other; transient synovitis resolves gradually after several days with no serious complications.[41] Kocher et al. have identified and verified four independent indicators (ESR >40 mm/h, WBC >12,000 cells/mm3, fever >38.5°C, and refusal to bear weight) to help distinguish between septic arthritis and toxic synovitis; however, these were proven to be of limited predicted value by other studies.[42,43] When two or more of these four independent variables are present, the likelihood is that septic arthritis will be the diagnosis. In addition, it has been demonstrated that CRP is a more accurate independent predictor of pediatric septic arthritis than ESR.[44] On imaging, lack of synovial hypertrophy, bone marrow edema, intact cartilage, and absence of erosions favors transient synovitis [Figure 17].
- (a-c) An 8-year-old child with recent onset of the right hip pain and limp. No fever. (a) Anteroposterior pelvic radiograph is unremarkable. (b and c) Magnetic resonance imaging of pelvis – short-tau inversion recovery (STIR) and T1-weighted coronal images show mild effusion and synovitis in the right hip joint (white arrow in b). No edema or collections in the peri-articular soft tissues. No bone marrow edema or erosions.
The key point is that it is vital to have an extremely high suspicion of septic arthritis in the setting of monoarthritis, particularly in the pediatric population, as misdiagnosis or delayed treatment has irreversible and morbid consequences [Figure 18].

- (a-f) The anteroposterior radiographs of the pelvis show a spectrum of post-infective sequel in various patients – (a) subluxation of the left hip joint due to capsular and ligament laxity, (b) coxa magna and breve of the right femur, (c) right hip joint arthritis with articular surface irregularity and small femoral head, (d) complete resorption of the right femoral head and neck, (e) avascular necrosis of the right femoral head and (f) complete ankylosis of the right hip joint.
CATEGORY IV – MIMICS AND OTHERWISE-NON-SPECIFIED CONDITIONS
There are many differentials for a patient presenting with hip pain and mimicking and inflammatory joint pathology. A few of the key differentials that should be kept in mind are listed in this category. In the pediatric population, transient synovitis and idiopathic chondrolysis of the hip (ICH) are the two main confounders in a child with acute/subacute hip monoarthritis. Transient synovitis has already been briefly discussed.
ICH
Chondrolysis or cartilage destruction classically occurs in the setting of a septic joint. ICH is another pathology of unknown etiology, wherein rapid cartilage destruction is followed by degenerative structural changes. The destruction of articular cartilage in idiopathic chondrolysis is not associated with significant inflammation.[45]
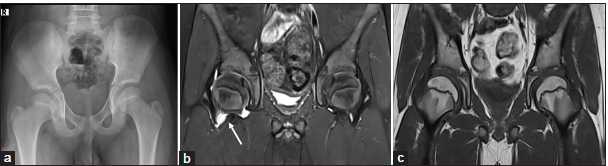
Cartilage loss is typically central to begin with, and MRI shows a trapezoidal segment of central epiphyseal signal change near the ligamentum teres, as the most characteristic finding.[46] This is usually accompanied by mild joint effusion, and synovitis is not a consistent feature. If untreated, in some cases, it progresses to severe osteoarthritis-like features and even partial ankylosis of the joint [Figures 19 and 20].
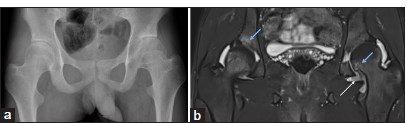
- (a-c)An 11-year-old female child with pain and stiffness in the right hip for 2 months. (a) Anteroposterior pelvic radiograph shows mild narrowing of the medial right hip joint space and ipsilateral pelvis tilting. (b and c) Magnetic resonance imaging of pelvis – short-tau inversion recovery (STIR) and T1-weighted coronal images reveal a focal area of thinning of the articular cartilage with geographic edema of the underlying marrow (white arrow) in the middle one-third of the right proximal femoral epiphysis suggests idiopathic chondrolysis of the right hip joint. Minimal reactive right hip joint effusion is noted.
- (a-c) A 13-year-old female child with left hip pain and stiffness for one year. (a) Anteroposterior pelvic radiograph shows concentric narrowing of the left hip joint space and ipsilateral pelvis tilting. (b and c) Magnetic resonance imaging of pelvis – short-tau inversion recovery (STIR) and T1-weighted coronal images demonstrate complete loss of articular cartilage with diffuse ill-defined edema of the femoral head and acetabulum and focal areas of fibrous ankylosis (thin white arrow). Minimal left hip joint effusion (blue arrow) is seen.
Rapidly progressive chondrolysis or osteoarthritis of hip joint
Another unique hip disorder of uncertain etiology characterized by rapid chondrolysis (>2 mm in 1 year or 50% joint-space narrowing in 1 year) in adults is “rapidly destructive osteoarthritis of the hip.”[47] The profile of affected patients is usually women, and the average age at onset (60–70 years) is greater than that of patients with regular osteoarthritis. Radiographs initially show no or mild osteoarthritic changes with severe progressive joint destruction with focal joint-space narrowing and extensive subchondral bone loss in the femoral head and/or acetabulum seen within a few months interval. No significant osteophyte formation is noted. MRI features include joint effusion, rapidly progressive cartilage loss, extensive bone marrow edema-like pattern in the femoral head and neck, and femoral head flattening along with cyst-like subchondral defects.[48]
Other important differentials
Other pathologies that may mimic inflammatory joint disease include an intra-capsular osteoid osteoma [Figure 21], synovial chondromatosis [Figure 22], tenosynovial giant cell of the tumor of the joint [Figure 23], marrow abnormalities related to infiltrative and metabolic pathologies, avascular necrosis, and subchondral insufficiency fractures of the femoral head. Detailed descriptions of these are beyond the scope of the present article. However, it is important to remember these conditions and systematically exclude them in challenging cases.

- (a-g) Osteoid osteoma - A 14-year-old child with left hip pain and limp. (a) Anteroposterior pelvic radiograph shows a lytic lesion in the medial wall of the left acetabulum with cortical thickening and benign periosteal reaction (long white arrow). (b) Computed tomography coronal image shows a lytic lesion in the medial wall of the left acetabulum with cortical thickening (white arrow). (c-e) Magnetic resonance imaging of pelvis – short-tau inversion recovery and T1-weighted coronal and T2 axial shows an isointense to the hypointense lesion with cortical thickening (white arrow) in the left medial wall of the left acetabulum with associated reactive bone marrow edema and mild left hip joint effusion and synovitis.
- (a-e) A 13-year-old male child with left hip pain and limp for three years. (a) Anteroposterior pelvic radiograph shows numerous ossified loose bodies (thin white arrow) in the left hip joint with juxtaarticular osteopenia, widening of the acetabular roof and coxa magna. (b-e) Magnetic resonance imaging of pelvis – (b and c) short-tau inversion recovery coronal and axial, (d) T1-weighted coronal, and (e) proton density sagittal images demonstrate numerous ossified loose bodies (white arrow in b-e), thinning of the articular cartilage and erosions of the femoral head (blue arrow in b and e).
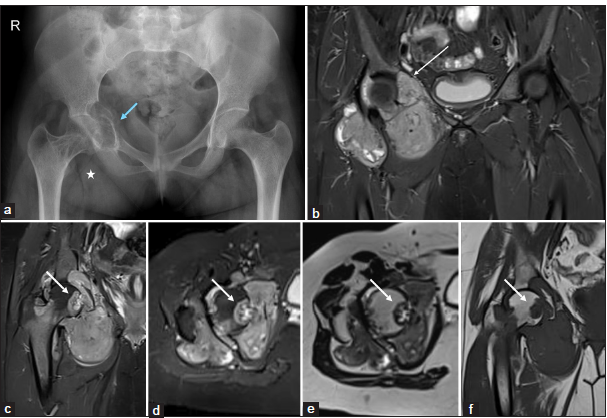
- (a-f) A 20-year-old lady with right hip pain. (a) Anteroposterior pelvic radiograph shows increased soft tissue opacity (white asterisk) in the right hip joint with erosions of the femoral head and acetabulum and mild expansion of the acetabulum (blue arrow). (b-f) Magnetic resonance imaging of pelvis – (b-d) short-tau inversion recovery coronal and axial, (e) T2-weighted axial, and (f) T1w coronal images show nodular synovial proliferation with characteristic T2 low signal intensity with erosions of the femoral head (white arrow in c-f) and erosions of the acetabulum (long white arrow in b).
A suggested algorithm to help systematically approach a patient with inflammatory hip joint pathology is depicted in the flow chart [Figure 24].
![Flowchart depicting the various inflammatory and infective arthritis of the hip joint. [JIA: Juvenile idiopathic arthritis, RA: Rheumatoid arthritis, SpA: Spondyloarhtiris, Ank Spond: Ankylosing spondylitis, IBD: Inflammatory bowel disease, ICH: Idiopathic chondrolysis of hip, RPOA: Rapidly progressive osteoarthritis, PVNS: Pigmented villonodular synovitis, AVN: Avascular necrosis, HADD: Hydroxyapatite deposition disease, CPPD: Calcium pyrophosphate deposition disease, GOUT: Gouty arthritis].](/content/107/2025/7/1/img/IJMSR-7-026-g024.png)
- Flowchart depicting the various inflammatory and infective arthritis of the hip joint. [JIA: Juvenile idiopathic arthritis, RA: Rheumatoid arthritis, SpA: Spondyloarhtiris, Ank Spond: Ankylosing spondylitis, IBD: Inflammatory bowel disease, ICH: Idiopathic chondrolysis of hip, RPOA: Rapidly progressive osteoarthritis, PVNS: Pigmented villonodular synovitis, AVN: Avascular necrosis, HADD: Hydroxyapatite deposition disease, CPPD: Calcium pyrophosphate deposition disease, GOUT: Gouty arthritis].
CONCLUSION
The hip joint is affected by various inflammatory and infective pathologies. MRI has emerged as the preferred imaging modality of choice due to its ability to clearly depict the pathologic process, disease activity, and structural damage and to identify complications. Radiographs form a baseline and should be reserved for cases with known chronic changes. Ultrasound helps identify effusion and guided interventions but is limited by the lack of standard imaging protocols and suboptimal window. A systematic approach, knowledge of various imaging findings and clinical features will help improve diagnostic accuracy.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- MR imaging of hip infection and inflammation. Magn Reson Imaging Clin N Am. 2013;21:127-39.
- [CrossRef] [PubMed] [Google Scholar]
- Hip imaging: Normal variants and asymptomatic findings. Semin Musculoskelet Radiol. 2017;21:507-17.
- [CrossRef] [PubMed] [Google Scholar]
- ACR appropriateness criteria® chronic hip pain. J Am Coll Radiol. 2017;14:S90-102.
- [CrossRef] [PubMed] [Google Scholar]
- MRI findings in hip in juvenile idiopathic arthritis. J Clin Med. 2021;10:5252.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome in juvenile idiopathic arthritis: A population-based study from Sweden. Arthritis Res Ther. 2019;21:218.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of joint involvement in juvenile idiopathic arthritis during a 5 year follow-up of newly diagnosed patients: Implications for MR imaging as outcome measure. Rheumatol Int. 2015;35:351-7.
- [CrossRef] [PubMed] [Google Scholar]
- The natural history of hip involvement in juvenile rheumatoid arthritis: A radiological and magnetic resonance imaging follow-up study. Rev Rhum Engl Ed. 1997;64:173S-8.
- [Google Scholar]
- Long-term follow-up of 246 adults with juvenile idiopathic arthritis: Functional outcome. Rheumatology. 2002;41:1428-35.
- [CrossRef] [PubMed] [Google Scholar]
- The role of MRI in the evaluation of hip joint disease in clinical subtypes of juvenile idiopathic arthritis. Br J Radiol. 2002;75:229-33.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical assessment and core outcome variables are poor predictors of hip arthritis diagnosed by MRI in juvenile idiopathic arthritis. Rheumatology (Oxford). 2007;46:699-702.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in MRI findings between subgroups of recent-onset childhood arthritis. Pediatr Radiol. 2011;41:432-40.
- [CrossRef] [PubMed] [Google Scholar]
- Role of MRI in evaluation of hip joint involvement in juvenile idiopathic arthritis. Egypt Rheumatol. 2012;34:75-82.
- [CrossRef] [Google Scholar]
- Inter-and intra-observer reliability of contrast-enhanced magnetic resonance imaging parameters in children with suspected juvenile idiopathic arthritis of the hip. Pediatr Radiol. 2018;48:1891-900.
- [CrossRef] [Google Scholar]
- Imaging assessment of children presenting with suspected or known juvenile idiopathic arthritis: ESSR-ESPR points to consider. Eur Radiol. 2020;30:5237-49.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus-driven conceptual development of a standardized whole body-MRI scoring system for assessment of disease activity in juvenile idiopathic arthritis: MRI in JIA OMERACT working group. Semin Arthritis Rheum. 2021;51:1350-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hip involvement in early rheumatoid arthritis. Ann Rheum Dis. 1995;54:45-8.
- [CrossRef] [PubMed] [Google Scholar]
- Radiological assessment of hip osteoarthritis. Lancet. 1999;353:87-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical manifestations and diagnosis of axial spondyloarthritis. J Clin Rheumatol. 2021;27:e547-60.
- [CrossRef] [PubMed] [Google Scholar]
- Hip disease in ankylosing spondylitis. Curr Opin Rheumatol. 2013;25:448-54.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical, radiographic and functional differences between juvenile-onset and adult-onset ankylosing spondylitis: Results from the PSOAS cohort. Ann Rheum Dis. 2008;67:233-7.
- [CrossRef] [PubMed] [Google Scholar]
- ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2006;65:442-52.
- [CrossRef] [PubMed] [Google Scholar]
- Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplasty. 2000;15:52-8.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty in patients with chronic autoimmune inflammatory arthroplasties. Int J Rheum Dis. 2010;13:235-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic contrast-enhanced magnetic resonance imaging in the assessment of disease activity in patients with juvenile idiopathic arthritis. Rheumatology (Oxford). 2009;49:178-85.
- [CrossRef] [PubMed] [Google Scholar]
- Gadolinium deposition in the brain: Summary of evidence and recommendations. Lancet Neurol. 2017;16:564-70.
- [CrossRef] [PubMed] [Google Scholar]
- Gadolinium based contrast agents in current practice: Risks of accumulation and toxicity in patients with normal renal function. Indian J. Radiol Imaging. 2017;27:141-7.
- [CrossRef] [PubMed] [Google Scholar]
- Juvenile idiopathic arthritis of the knee: Is contrast needed to score disease activity when using an augmented MRI protocol comprising PD-weighted sequences? Eur Radiol. 2023;33:3775-84.
- [CrossRef] [PubMed] [Google Scholar]
- Rheumatoid arthritis of the hip. J Am Acad Orthop Surg. 1997;5:332-8.
- [CrossRef] [PubMed] [Google Scholar]
- Case report 733. Calcific tendinitis of the origin of the medial and lateral heads of the rectus femoris muscle and the anterior iliac spin (AIIS) Skeletal Radiol. 1992;21:271-2.
- [CrossRef] [PubMed] [Google Scholar]
- Hydroxyapatite crystal deposition disease around the hip: A rare cause of piriformis syndrome and ischiofemoral impingement. BJR Case Rep. 2022;7:20210075.
- [CrossRef] [Google Scholar]
- Calcium pyrophosphate deposition disease: Clinical manifestations. Reumatismo. 2012;63:246-52.
- [CrossRef] [PubMed] [Google Scholar]
- Hip involvement in patients with calcium pyrophosphate deposition disease: Potential and limits of musculoskeletal ultrasound. Arthritis Care Res (Hoboken). 2019;71:1671-7.
- [CrossRef] [PubMed] [Google Scholar]
- Calcium pyrophosphate dihydrate crystal deposition disease: Nomenclature and diagnostic criteria. Ann Intern Med. 1977;87:241-2.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiology and treatment of gout arthritis; including gout arthritis of hip joint: A literature review. Hip Pelvis. 2024;36:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound and clinical features of hip involvement in patients with gout. Joint Bone Spine. 2019;86:633-6.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of acute septic arthritis of the hip joint in pediatric patients aged 10 years or younger. Arthroscopy. 2020;36:464-72.
- [CrossRef] [PubMed] [Google Scholar]
- Current approach to the evaluation and management of septic arthritis. Pediatr Emerg Care. 2019;35:50913.
- [CrossRef] [PubMed] [Google Scholar]
- Septic arthritis of the hip in children: A critical analysis review. JBJS Rev. 2020;8:e0103.
- [CrossRef] [PubMed] [Google Scholar]
- Gadolinium DTPA-enhanced magnetic resonance imaging of musculoskeletal infectious processes. Skelet Radiol. 1995;24:325-30.
- [CrossRef] [Google Scholar]
- Differentiating between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg. 1999;81:1662-70.
- [CrossRef] [PubMed] [Google Scholar]
- Differentiation between septic arthritis and transient synovitis of the hip in children with clinical prediction algorithms. J Bone Joint Surg. 2004;86:956-62.
- [CrossRef] [PubMed] [Google Scholar]
- Acute monoarthritis in children: clinical and laboratory factors distinguishing septic arthritis from noninfectious inflammatory arthritis. Eur Rev Med Pharmacol Sci. 2023;27:1278-87.
- [Google Scholar]
- Idiopathic chondrolysis of the hip In: The pediatric and adolescent hip. Berlin: Springer; 2019.
- [CrossRef] [Google Scholar]
- Idiopathic chondrolysis of the hip in children: Early MRI findings. AJR Am J Roentgenol. 2009;192:526-31.
- [CrossRef] [PubMed] [Google Scholar]
- Rapidly destructive osteoarthritis of the hip: MR imaging findings. Am J Roentgenol. 2002;179:657-63.
- [CrossRef] [PubMed] [Google Scholar]







