Translate this page into:
Non-dominant leading wrist injuries in Indian professional cricketers

*Corresponding author: Abhinetri K.S.V., Department of Radiology, Mahajan Imaging, Sports Injury Centre, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. abhinetri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Batta NS, Abhinetri K, Batra V, Mittal M, Jain V. Non-dominant leading wrist injuries in Indian professional cricketers. Indian J Musculoskelet Radiol. 2023;5:97-105. doi: 10.25259/IJMSR_23_2023
Abstract
Cricket is a popular sport played worldwide, immensely popular in India, with a high prevalence of wrist and hand injuries varying from 11% to 13%. Among batsmen, the injury rates are higher in the non-dominant leading wrist. These injuries affect the ligaments, bones, triangular fibrocartilage complex, tendons, and neurovascular structures predominantly on the palmar and ulnar aspect of the wrist and occur due to the force vectors transmitted to the wrist during the bat swing. Specific injuries can be explained by the biomechanics of this double grip sport, and its force vector knowledge of these injuries can enable the sports physician to diagnose early and effectively treat the athlete, improving their performance and outcome. The main intent of this article is to review the biomechanics and clinical presentation of the most common injuries in the non-dominant or leading wrist of cricketers.
Keywords
Leading wrist
Non-dominant wrist
Cricketers
Hamate fracture
INTRODUCTION
Cricket is undoubtedly one of the most popular sports globally, with a massive following in countries like India. It is the second most popular sport in the world after football, being played in 105 member countries of the International Cricket Council. While cricket is considered a non-contact sport, it involves a wide range of physical activities, including batting, throwing, bowling, diving, catching, fielding, and running. As a result, injuries are quite common among cricketers, and these injuries can be classified based on various factors, including mode of onset as:- acute-onset non-contact injuries (e.g., anterior cruciate ligament tear due to twisting injury and ankle sprain while running), impact/traumatic injury (e.g., hamate fracture while batting and mallet finger while catching), gradual onset injuries (overuse injuries such as chronic low backache in fast bowlers secondary to pars interarticularis stress fractures), insidious without known mode of onset (e.g., ulnar-sided wrist pain due to extensor carpi ulnaris [ECU] tendinosis, anterior knee pain due to chondromalacia patella, and shoulder pain in overhead throwers secondary to superior labral anterior posterior lesions), and other medical illnesses.[1]
Studies have shown that approximately 25% of sports injuries involve the wrist and hand,[2] with a prevalence of 11–13% specifically in cricket.[3] The right or dominant hand is more frequently injured, often due to direct impact, either with the ball or the ground, and is more common while fielding rather than during batting,[4] whereas the non-dominant or leading hand is prone to a different set of injuries commonly related to the mechanics of the batting swing, which we will elaborate in this article.
BIOMECHANISM OF THE BATTING SWING AND WRIST INJURY IN THE LEADING WRIST
Understanding the mechanics of the cricket batting swing is crucial for comprehending the etiology of specific wrist injuries in the sport. The double-grip nature of cricket, where the batsman holds the handle of the bat with both hands, plays a significant role in how these injuries occur. The batting swing consists of five phases: the stance, backswing, forward stride, downswing to impact, and follow-through. The non-dominant or the leading wrist (the left wrist for a right-handed batsman) holds the top of the bat’s handle, and the trailing or dominant wrist (the right wrist for a right-handed batsman) is placed lower. During the stance and backswing phases, the non-dominant wrist is stabilized in a neutral position, and this is termed “locking” or “cocking” of the wrist [Figures 1a and b]. The leading wrist is “unlocked” or “uncocked” during the downswing phase to give placement and direction to the shot. It involves hitting the ball terminally in ulnar deviation and flexion [Figure 1c]. The sudden ulnar deviation of the leading wrist while uncocking makes it more susceptible to ulnar-sided injuries of the wrist. The dominant wrist plays a crucial role in generating power during the swing. It goes into extension during the backswing and reverts to a neutral (and ultimately flexion) position just before striking the ball. Studies have shown a correlation between distal ulnar loading and increasing ulnar deviation during the cricket swing. The force vectors and stresses placed on the wrist during the swing contribute to the risk of specific wrist injuries, such as ulnar-sided injuries.[5] The mechanics of the cricket swing and the resulting wrist injuries have similarities with other double-grip sports, namely, golf, racquetball, and tennis.
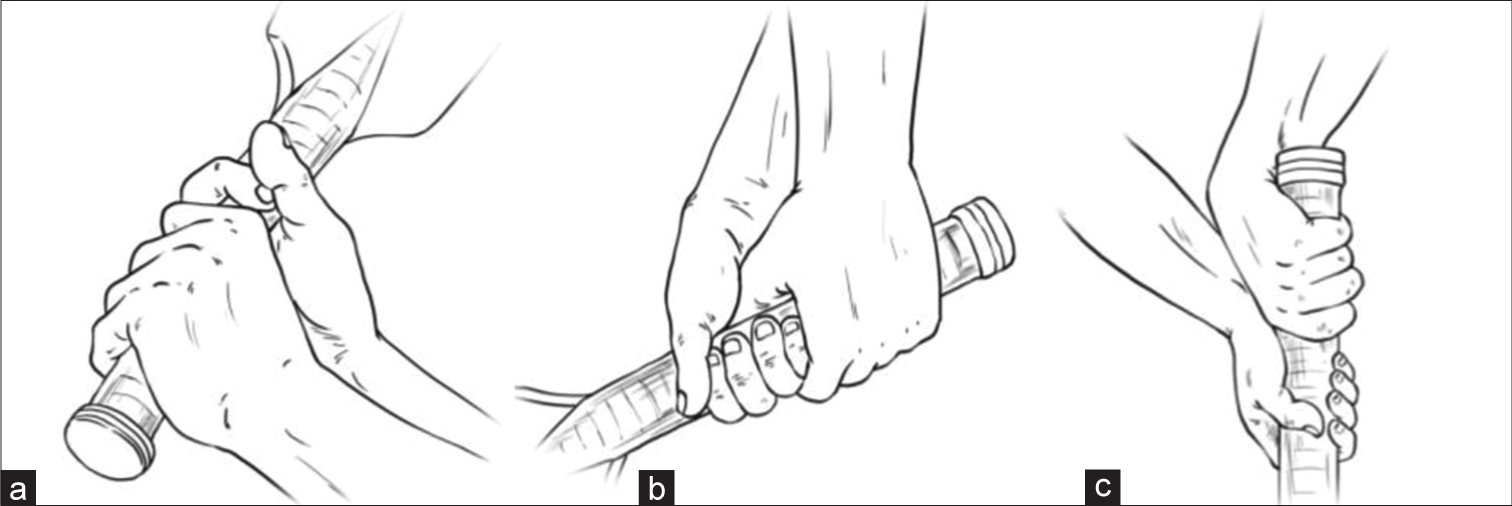
- Biomechanism of the batting swing. (a and b) The leading, non-dominant left wrist in right-handed batsmen, is in a neutral position during the stance and backswing phases. This is called cocking of the wrist. (c) During the downswing phase, the lead wrist is “unlocked” or “uncocked,” and at impact, it is in ulnar deviation and flexion. The trailing or dominant wrist (right wrist for a right-handed batsmen) moves in a different path altogether, moving quickly into maximal extension during the backswing, and coming back to neutral and ultimately flexion just before the ball strikes. The sudden ulnar deviation movements of the leading wrist while uncocking the wrist are likely to predispose to ulnar-sided injuries of the wrist.
HAMATE FRACTURES
Hamate fractures are relatively uncommon, accounting for approximately 2–4% of all carpal bone fractures. They are frequently observed among individuals who participate in double grip sports such as golf, baseball, or racquet sports.[6] These sports involve repetitive motions and high-impact forces that can lead to hamate hook fractures.
In cricket, batsmen are at risk of either acute fractures or chronic stress injuries affecting the hamate bone. The mechanism of injury often involves the impaction of the bat’s handle onto the volar and ulnar aspect of the hand, resulting in stress loading on the hamate hook. Factors like a slight relaxation of the grip during the swing or sudden resistance, such as hitting the ground, can transmit the centrifugal force of the swing or impact into the base of the hand, leading to a hamate hook fracture.
Stress injuries, on the other hand, develop gradually and are a result of repetitive microtrauma rather than a single traumatic episode. The leading (top) hand in cricket is particularly susceptible to injury as the bat’s handle rests on the hamate hook, and it is the non-dominant hand in which 100% of hamate hook fractures occur.[7] In other sports, such as tennis and racquet sports, where the arm is stretched or abducted and involves a single-hand grip, the dominant hand may be more at risk for hamate fractures due to the different biomechanical forces involved.[8] Symptoms of hamate hook injury typically include ill-defined deep ulnar-sided wrist pain, weakness of grip, and pain on flexion/abduction of the little finger, especially during resisted movements.
Diagnosing hamate hook fractures can be challenging because plain radiographs may not always clearly demonstrate the injury. As a result, the true incidence of these fractures may be higher than reported, as some cases might be missed initially. To improve diagnosis, other imaging modalities such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be necessary to visualize the fracture more accurately. In addition, a high index of suspicion is required, especially in athletes with persistent ulnar-sided wrist pain and grip weakness, to ensure timely diagnosis and appropriate management.
The anatomy of the hamate bone and its hook-like protuberance is crucial in understanding the potential consequences of a hamate hook fracture. The body of the hamate is located dorsally at the ulnar aspect of the carpal row. Its hook-like protuberance (also known as the hamulus) is a thin, long structure that projects radially and volarly to the hypothenar eminence. The hamulus serves as an attachment site for the transverse carpal ligament, pisohamate ligament, opponens digiti minimi, and flexor digiti minimi. The hamulus is in close anatomic proximity to the ulnar nerve, which lies just superficial to it. An acute or chronically non-united displaced hamulus fracture can impinge on the ulnar nerve or its bifurcation and result in ulnar nerve neuropathy. The other potential consequence of a hamate hook fracture is damage to the adjacent flexor tendons. A sharp, bony, fractured fragment may irritate the adjacent flexor tendons, either flexor digitorum profundus or superficialis tendons, eventually causing fraying or rupturing.[9] This can result in significant impairment in finger movement and grip strength.
Hamate fractures can be categorized as either body fractures or hook fractures. Combined body and hook fractures are extremely rare. The hook of hamate fractures is further classified into three types based on their anatomic location: type 1 fractures that involve the distal tip, type 2 fractures involving the mid portion, and type 3 fractures involving the base of the hook. Type 3 fractures are the most common, accounting for over 75% of the hamate hook fractures.[10]
Radiographically, on posteroanterior radiographs of the wrist, the hook of the hamate is seen as an ovoid to triangular bony density overlapping the midportion of the distal hamate body. Radiographic signs of a hook of hamate fracture include (1) Ring sign, which refers to the discontinuity of the cortical ring of the hook of hamate, (2) ghostly shadow sign, which refers to the non-visualization of the hamate hook with radiolucency at its expected location, indicating a displaced fracture, and (3) diffuse sclerosis of the hook of hamate with poor delineation of the cortical ring of the hook Figures 2a and b reflecting sclerosis of the fracture margins in cases of non-union.[11]
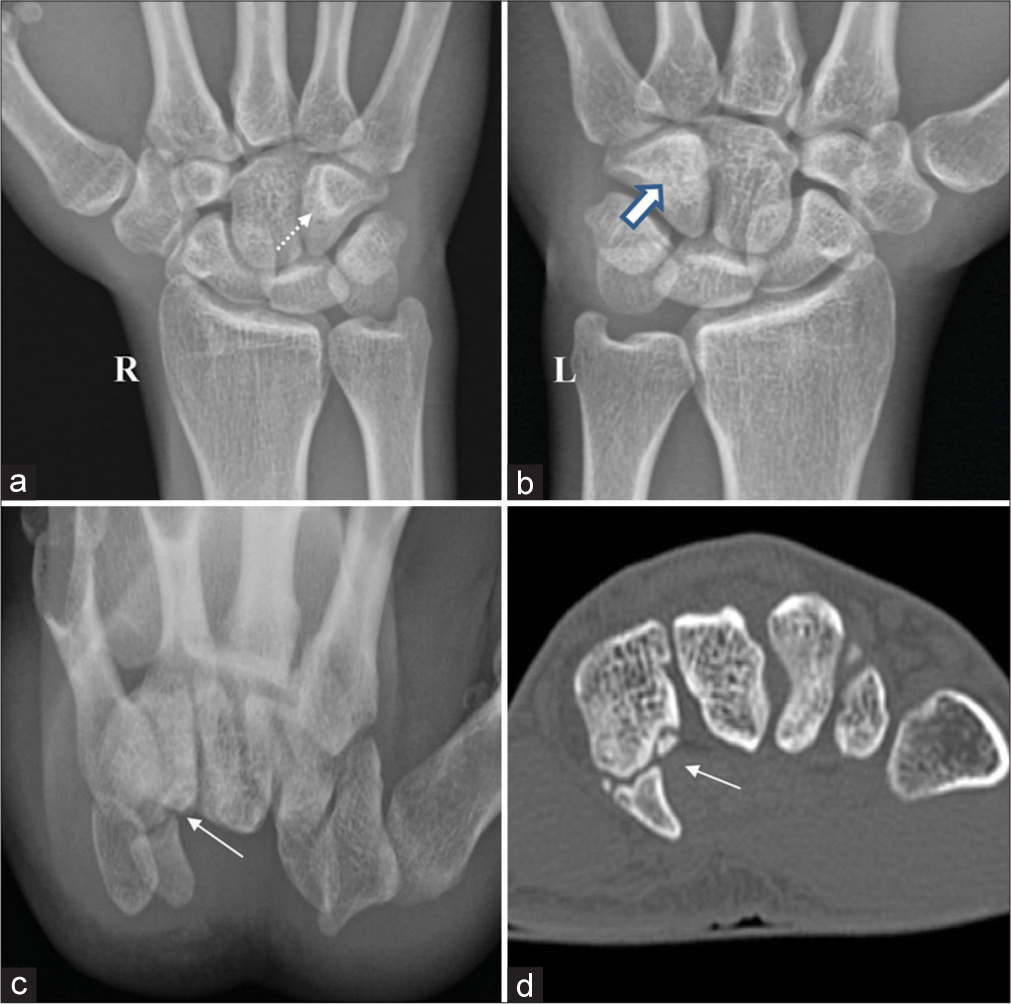
- Hamate fracture in the non-dominant left wrist of a 23-year-old cricketer. (a) AP radiograph of the right wrist reveals the normal triangular appearance of the hook of hamate (dotted arrow). (b) The AP radiograph of the left wrist shows mild sclerosis in the left hamate bone with non-visualization of the triangular hook of the hamate (white arrow). (c and d) Carpal tunnel view radiograph and axial computed tomography of the left wrist reveal an old fracture of the hook of the hamate with sclerotic margins (thin white arrows).
Evaluating the hook of the hamate with standard lateral wrist radiographs can be challenging due to overlap with other carpal bones, limiting their ability to detect fractures accurately. To improve visibility and diagnostic accuracy, specialized radiographic views such as carpal tunnel and semi-supine oblique views are often used. However, obtaining these special views may not always be routine unless there is a high index of clinical suspicion. False-negative radiographic findings can occur with the hook of hamate fractures, even when special views are used in addition to the standard AP and lateral radiographs, leading to potential misdiagnosis.[12] The sensitivity of X-rays in detecting hook of hamate fractures can vary, with reported sensitivities ranging between 53% and 90%.[13] The location of the fracture within the hook of the hamate can also affect its detectability on radiographs. Types 1 and 2 hamate hook fractures, which occur at the distal tip or midpoint of the hook, are more readily detected in special views compared to fractures at the base of the hook, which tend to be obscured and are more challenging to visualize.[14]
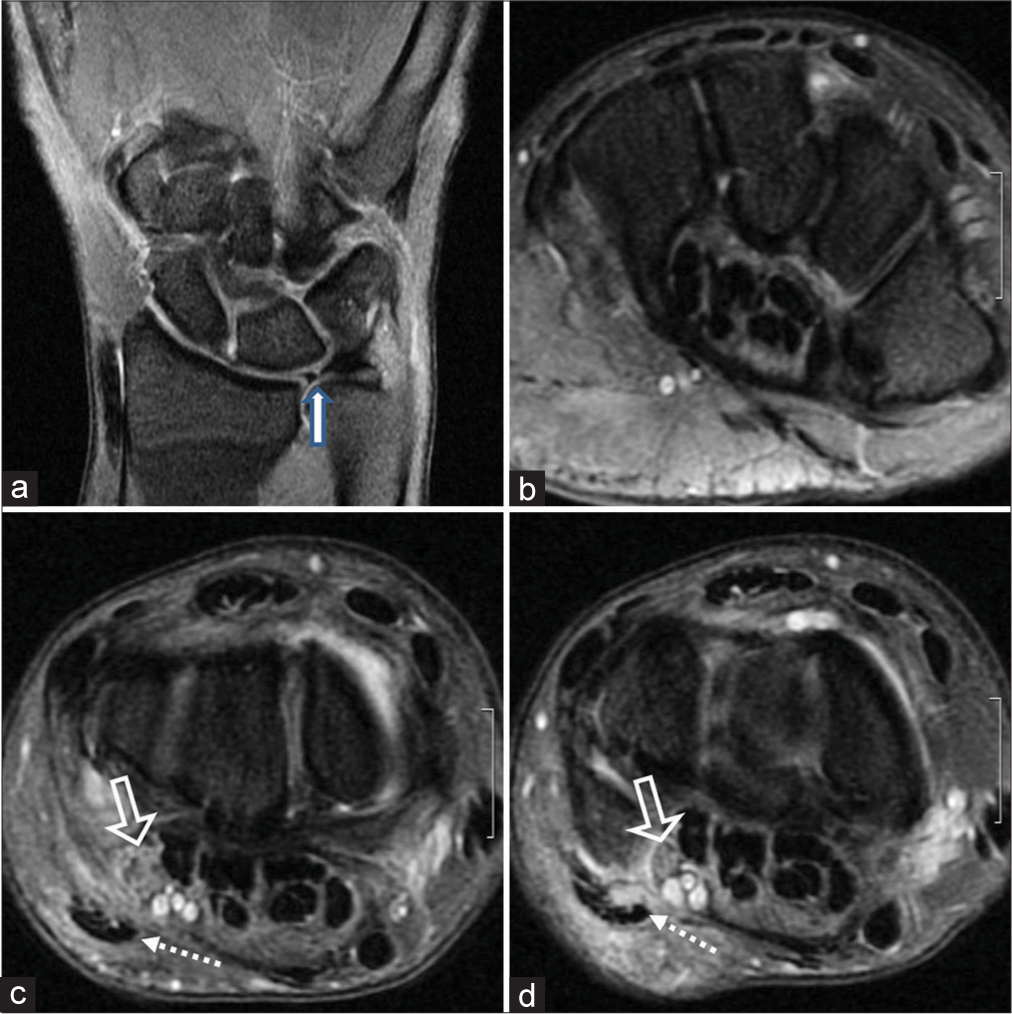
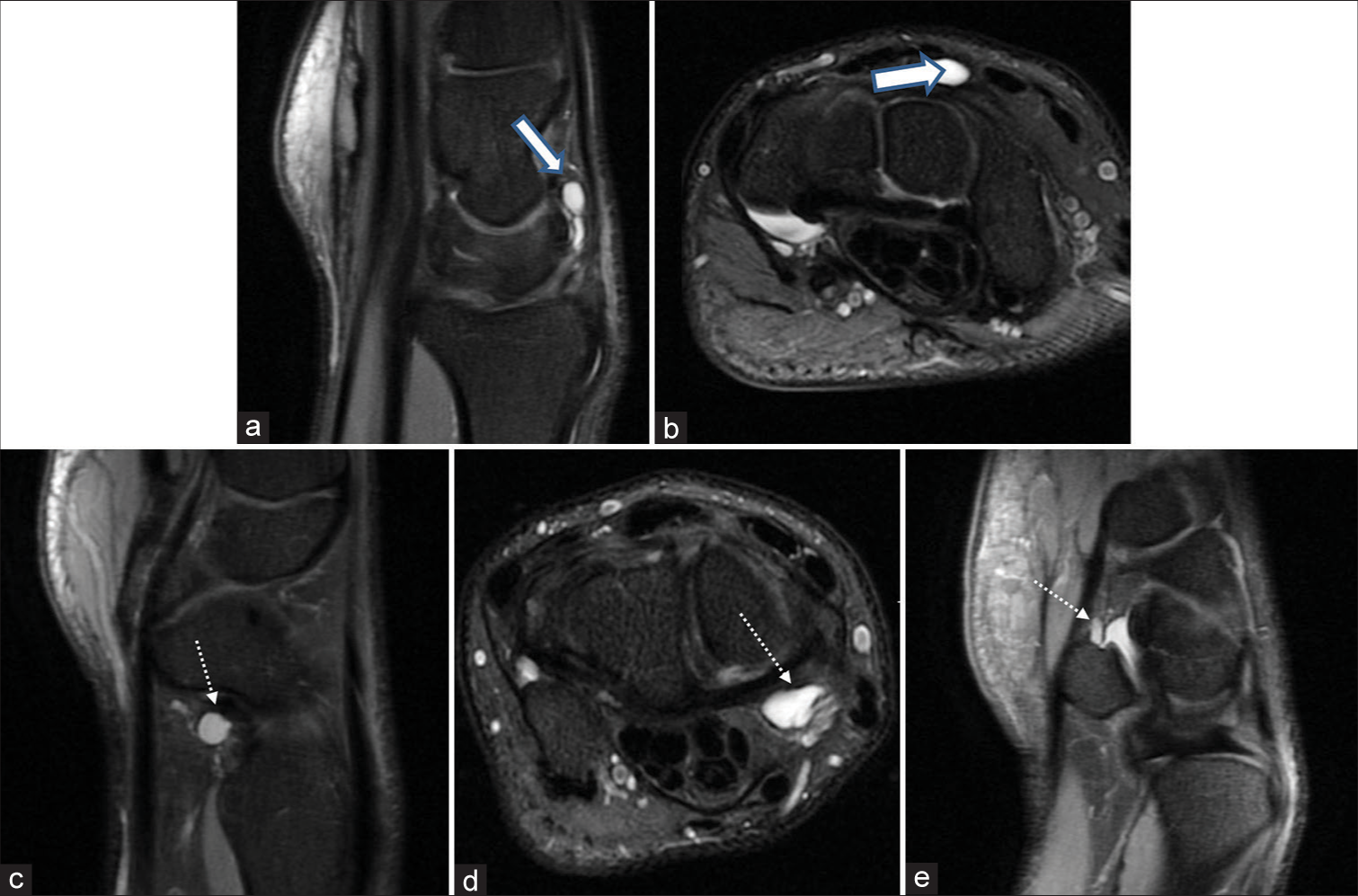
CT and MRI are highly sensitive imaging modalities for diagnosing hook of hamate fractures and play a crucial role in establishing a definitive diagnosis in both acute and chronic phases. CT has an excellent sensitivity of nearly 100% and is considered the reference standard for detecting hooks of hamate fractures, especially the type 3 (base of the hook) fractures.[13,14] CT can clearly visualize the fractured hamate hook and quantify the degree of displacement, which has implications for clinical decision-making. An acutely displaced fracture shows sharply defined margins on CT, while chronic non-united fractures may show sclerotic or corticated margins [Figure 2c and d]. CT can also identify undisplaced fractures, which appear as a thin, sharply defined linear radiolucency at the site of cortical disruption. It is also valuable in assessing fracture healing after treatment. MRI is useful for detecting hook of hamate fractures, which may appear as thin linear low-signal intensity with associated marrow edema, especially in the acute phase [Figures 3-6]. Stress injuries of the hook of hamate manifest as marrow edema on proton density fatsuppressed/short-tau inversion recovery images without T1 signal change. The degree of displacement may also be determined by MRI, in addition to evaluating concomitant injuries, such as ulnar nerve and flexor tendon injuries. Overall, both CT and MRI offer valuable insights into the diagnosis and management of hook of hamate fractures. CT is particularly useful for assessing fracture displacement and healing, while MRI is well-suited for detecting acute fractures and associated soft-tissue injuries. The choice of imaging modality may depend on clinical indications, patient presentation, and the need for precise anatomical evaluation.
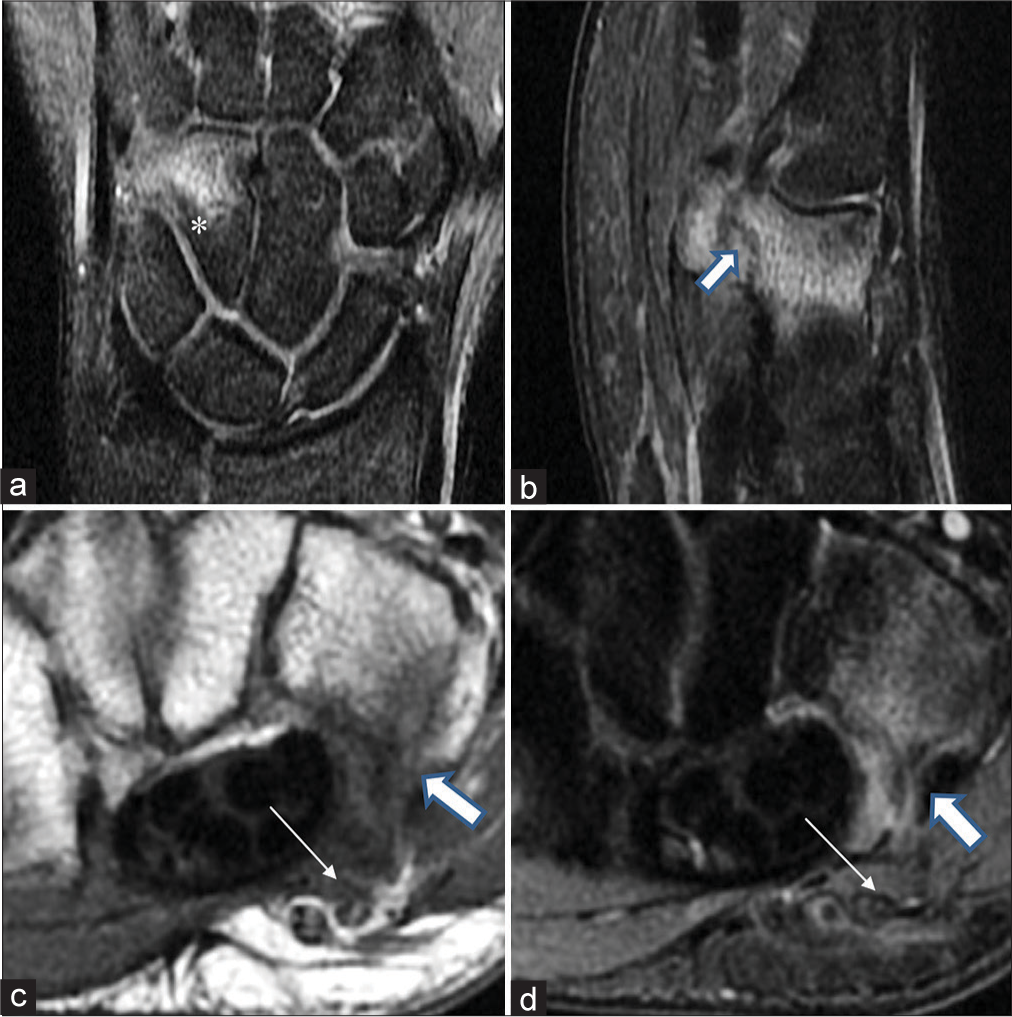
- Hamate stress fracture in the non-dominant wrist of a 21-year-old batsman presenting with ulnar-sided wrist pain. (a) Coronal proton density fat-suppressed (PDFS) images show ill-defined areas of marrow edema compatible with hamate bone contusion (*). (b-d) A well-defined hypointense dark linear signal (thick white arrow) is seen at the hook of hamate in sagittal PDFS (b), axial T1-weighted (c), and axial short-tau inversion recovery weighted (d) images. The thin white arrows mark blurring of the perineurial fat stripe along the ulnar nerve, which internally does not show any abnormal signal (c and d).
- Post-traumatic ulnar-sided pain in the leading wrist of a 20-year-old batsman. (a) Coronal proton density fat-suppressed (PDFS) images reveal an area of mild marrow edema at hamate (*) and mildly negative ulnar variance (double-ended arrow). (b) The axial T1-weighted image proximal to the level of distal radioulnar articulation depicts a shallow extensor carpi ulnaris groove (open white arrow) but no obvious subsheath or tendon tear. (c and d) Axial T1 and PDFS images exhibit the linear dark fracture line (white arrow) at the base of elongated hook of hamate which is compatible with a healing stress fracture.
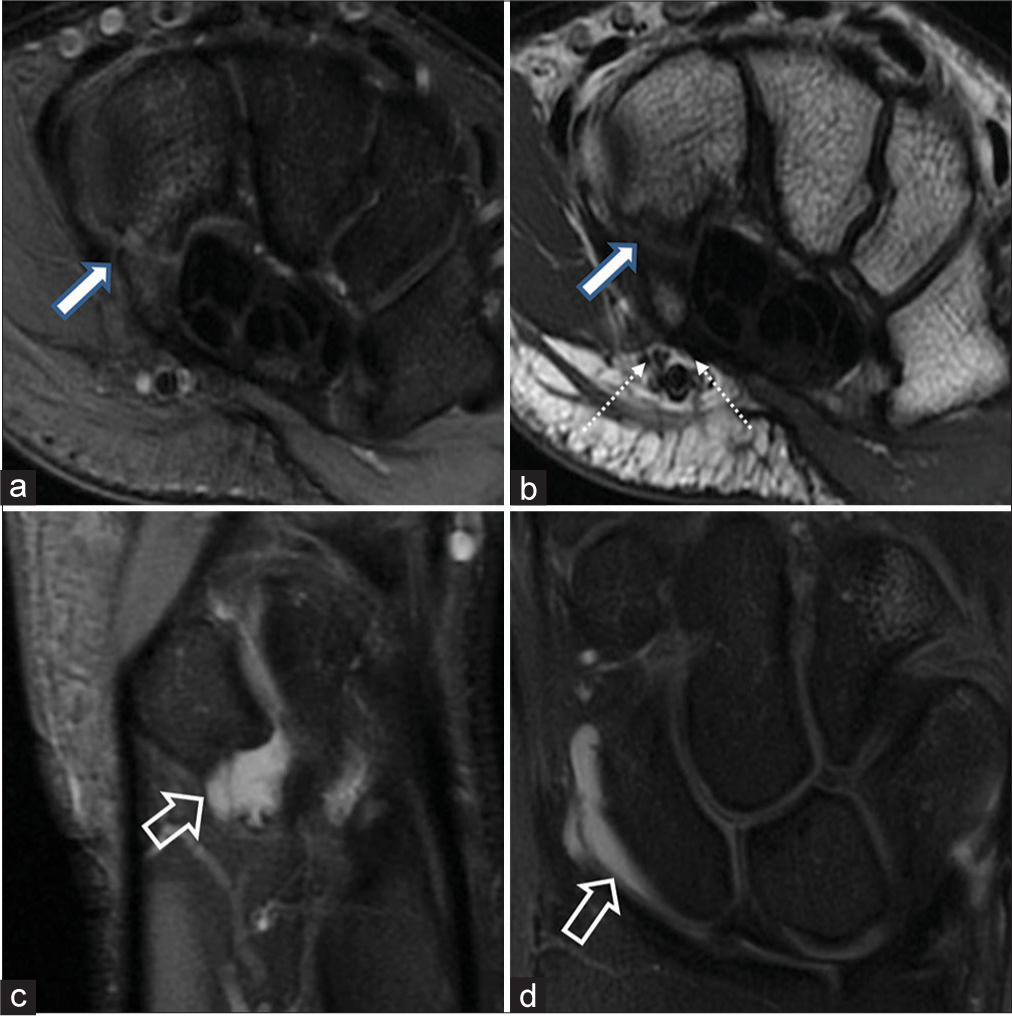
- Volar-sided pain in the left wrist of a 22-year-old batsman. (a and b) Axial proton density fat-suppressed and T1W images delineate a mildly distracted hamate hook fracture (thick white arrows) with intervening intermediate bright signal at the fracture site. The two branches of the ulnar nerve (medial-motor and lateral-sensory) marked by dotted white arrows (b) are intimately associated with the tip of the hamulus and show preserved perineurial fat stripe, excluding traumatic neuritis. (c and d) Small multiloculated ganglion cyst is seen (open arrow) at the pisotriquetral articulation (c) and deep to the radioscaphocapitate volar extrinsic ligament (d).
- Elongated hamate hook with ulnar nerve neuritis and Palmer type IA triangular fibrocartilage complex injury in a 40-year-old cricketer presenting with paresthesia in the little and ring fingers. (a) Palmer type 1 central perforation is seen in the triangular fibrocartilage (thick white arrow). (b) Axial proton density fat-suppressed (PDFS) images reveal an elongated hook of hamate without any fracture or marrow edema in the hamate bone. (c and d) The ulnar nerve appears thickened and edematous with intrasubstance and perineural PDFS hyperintense signals consistent with ulnar neuritis (open arrows). The flexor carpi ulnaris tendon (dotted white arrows) also appears thickened and hyperintense on PDFS images with longitudinal interstitial tears and extensive soft-tissue inflammation in the hypothenar eminence.
ECU TENDON INJURIES IN CRICKETERS
The ECU tendon pathologies, such as overuse tendinopathy and tenosynovitis, longitudinal split tears of the tendon, and acute subsheath injuries with subluxation or dislocation, are significant wrist injuries, especially in athletes like batsmen, which can lead to significant downtime in professional sports. Approximately 67% of the wrist injuries in the leading hand occur on the ulnar aspect of the wrist, with ECU tendon injury accounting for the majority of the ulnar-sided injuries.[15] The ECU tendon originates from the lateral epicondyle of the humerus and the dorsal surface of the ulna. It passes through a fibro-osseous tunnel within the extensor retinaculum at the ulnar head, in the 6th extensor compartment, where it is stabilized by a tendon subsheath. Its subsheath resists subluxation of the ECU tendon relative to the ulna during pronation and supination. When this subsheath is damaged due to repetitive strain or even a single traumatic event, it may lead to ECU instability. The ECU inserts onto the medial base of the 5th metacarpal. Its main function is to extend, and adduct or ulnar deviate the wrist joint.
Batsmen are particularly vulnerable to ECU tendon injuries due to the complex nature of their swing, with sudden ulnar deviation at the terminal end of the swing as it unlocks to drive the ball. The ECU tendon is anatomically held by a thin subsheath, making it susceptible to injury, especially when subjected to excessive tensile loading, further leading to the breakdown of the loaded tendon.[16,17] Acute subsheath injuries typically present with sudden-onset ulnar-sided wrist pain, often preceded by a traumatic event. The concomitant shallow ulnar groove may act as a predisposing factor. A “snapping” sensation may be felt during wrist supination and ulnar deviation due to subluxation of the ECU tendon. In cases of acute subsheath injuries, MRI may reveal malalignment of the ECU tendon relative to the ulnar groove either during supination or pronation. Peritendinous soft-tissue edema and bone marrow edema may be centered around the subsheath itself or at its bone insertion.
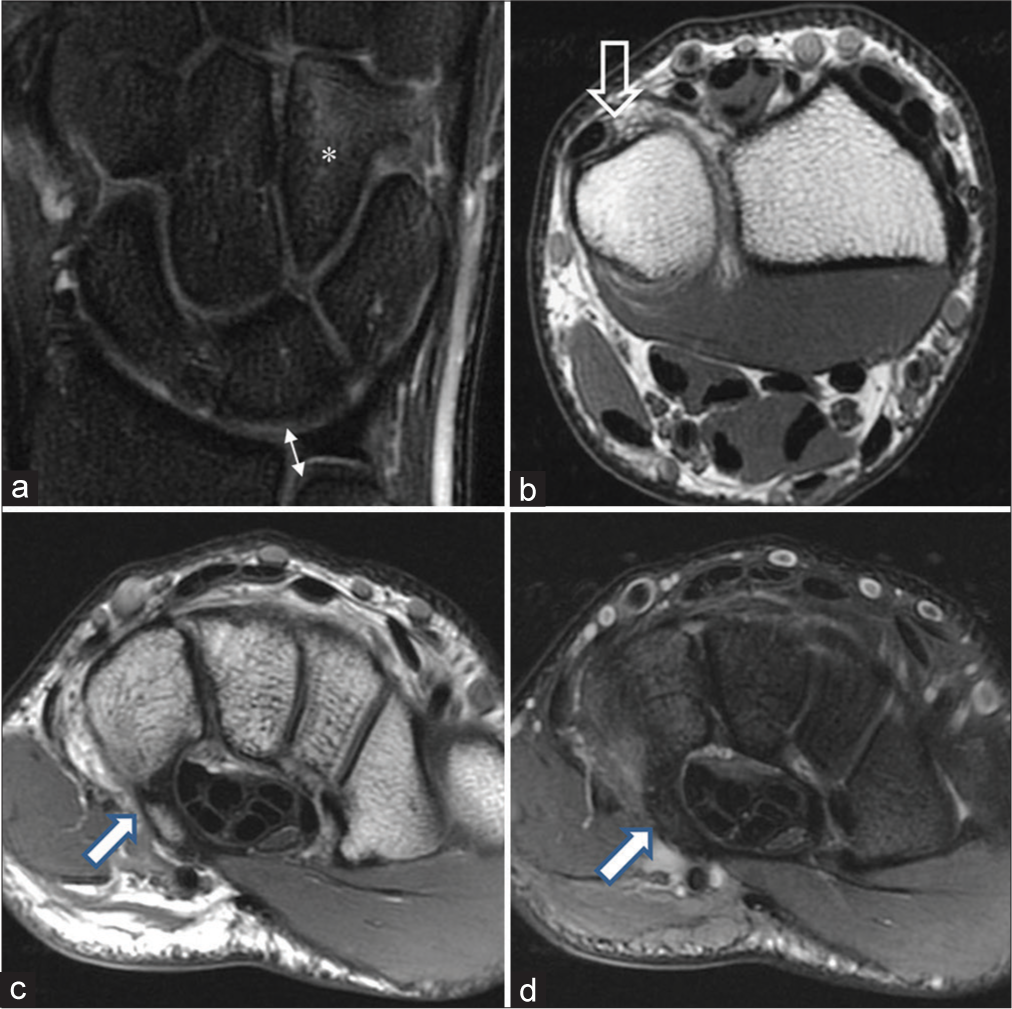
ECU tendinopathy and tenosynovitis are conditions that develop as a result of chronic overuse and mechanical irritation of the ECU tendon. ECU tendinopathy is a chronic overuse injury that occurs due to repetitive stress and strains on the ECU tendon. It may result in micro-tears when the musculotendinous unit is acutely exposed to excessive tensile forces, especially if the force is too sudden or too high. ECU tenosynovitis develops in a similar manner, resulting from mechanical friction between the ECU and the ulnar groove. It involves inflammation and irritation of the synovial sheath surrounding the ECU tendon. This condition often begins as tendon irritation manifesting as pain but can progress to friction between the tendon and the ulnar groove, leading to fluid distension of the tendon sheath. In batsmen, the repetitive motion and ulnar deviation of the wrist, especially in the supinated position, can contribute to ECU tenosynovitis. The key clinical signs of ECU tendinopathy include tenderness in the ECU groove on palpation and pain when the wrist is subjected to resisted extension and ulnar deviation. On MRI, the tendon may appear enlarged in size, and there may be increased signal intensity on both T1- and T2-weighted images due to increased fluid content within the tendon [Figure 7]. In more advanced cases, tears and longitudinal splits may be seen within the tendon. It is imperative to assess the tendon up to its insertion to fully evaluate the extent of the injury.
- Extensor carpi ulnaris (ECU) tendinosis in a 32-year-old cricketer with ulnar-sided pain in the leading wrist. (a and b) Marked thickening with intrasubstance hyperintense signal is seen in the ECU tendon on axial and coronal proton density fat-suppressed (PDFS) images (thick white arrow) with peritendinous edema and subsheath edema suggesting ECU tendinosis with tenosynovitis. (c and d) Axial PDFS images reveal irregular longitudinal splitting of the ECU tendon (dotted white arrow).
TRIANGULAR FIBROCARTILAGE COMPLEX (TFCC) INJURIES
Injuries to the TFCC can be a significant cause of ulnar-sided wrist pain, especially among batsmen who engage in rotation motions at the grip of the cricket bat. The TFCC is a vital structure in the wrist that plays a crucial role in stabilizing the distal radioulnar joint by transmitting the axial load between the ulna and the carpal bones.[18] It cushions and supports the lunate and the ulnar head during wrist movements, especially during ulnar deviation and axial loading of the wrist, and extends the gliding surface of the radius to facilitate smooth carpal motion. The TFCC comprises the triangular fibrocartilage (TFC), the meniscal homologue, the dorsal and volar radioulnar ligaments, the ulnar collateral, ulnolunate, ulnotriquetral, and triangular ligaments.
The TFCC complex is susceptible to overuse injuries and degeneration. A “weak” batting grip can lead to biomechanical abnormalities during the swing. Lack of effective uncocking at the bat swing can impose additional stress on the wrist, including compressive loading during ulnar deviation, thus contributing to TFCC injuries.
Since the TFCC has a differential attachment structure, with the radial side of the TFC disc having a hyaline cartilage attachment and the ulnar side having a bony attachment, the radial side is weaker and more vulnerable to injury compared to the ulnar side of the disc. The TFCC can tear or be strained from “hitting down on the ball” or from over-swinging. Hitting the bat on hard ground may also contribute to TFCC injury among batsmen. In an acute setting, TFCC tears can occur with hyperextension and pronation of the axially loaded, ulnar-deviated wrist. In the chronic setting, repetitive or micro trauma from rapid supination-pronation of the ulnar deviated wrist during the bat swing can cause peripheral TFCC tears over time.
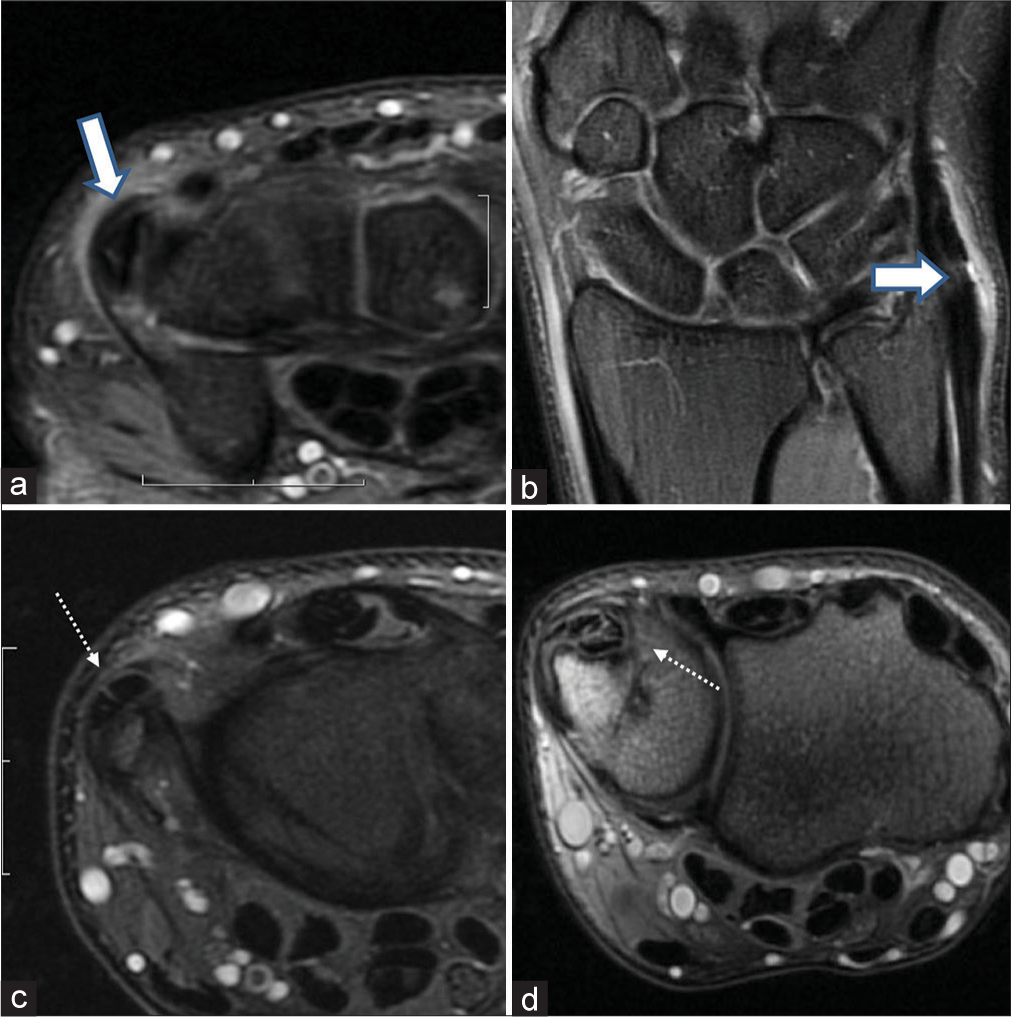
Patients commonly complain of deep, aching ulnar-sided wrist pain, which can be aggravated during gripping. Mechanical symptoms such as clicking or snapping may occur with pronation-supination. Tenderness at the prestyloid recess, which may be accentuated with extreme wrist movements, such as translation or rotation of the ulna, is a hallmark of TFCC injury. Standard radiographs do not demonstrate the TFCC but can be valuable for assessing the ulnar variance; the positive ulnar variance is a known risk factor for TFCC injuries. TFCC injuries are best evaluated with high-resolution MRI using dedicated wrist coils [Figure 8]. Supplementary magnetic resonance (MR) arthrography can enhance the detection of small or occult partial-thickness tears.
- Triangular fibrocartilage complex (TFCC) injury in a 31-year-old bats men with ulnar-sided pain in the non-dominant wrist. (a and b) Coronal GRE and proton density fat-suppressed images depict a central perforation (white arrows) through the triangular fibrocartilage consistent with Palmer type 1A TFCC injury.
The Palmers classification system groups TFCC injuries as either traumatic (class I) or degenerative (class II),[19] with further subclassification based on the underlying condition of the TFCC in degenerative lesions and the anatomical location of the traumatic injuries. Some patients with positive ulnar variance may also present with features of concomitant ulnar abutment syndrome.
GANGLION CYSTS
Ganglion cysts are common benign soft-tissue tumors most commonly encountered in the wrist. While they are commonly referred to as “cysts,” it is important to note that ganglion cysts are not true cysts because they lack a synovial or epithelial lining. Instead, they are surrounded by a pseudo capsule composed of compressed loose areolar tissue. The etiology or origin of ganglion cysts has been a subject of debate, and several theories have been proposed to explain their development. One of the most widely accepted theories is the “capsular rent” theory, which suggests the following sequence of events:- joint abnormality leads to altered biomechanics, weakening of the joint capsule, and eventual leakage of the synovial fluid into the periarticular tissue. This joint fluid incites a reaction with the periarticular soft tissue, leading to the formation of gelatinous cystic fluid and the development of the cyst wall. The small size of the rent results in a one-way valve mechanism preventing the extravasated fluid from returning to the joint, resulting in the gradual enlargement of the cyst. However, despite this widely accepted theory, there is no definitive correlation between the etiopathogenesis of ganglion cysts and their post-operative recurrence, despite arthroscopically confirming the presence of intra-articular joint pathology in 50% of ganglion patients. Alternatively, other theories propose alternate pathways for ganglion cyst formation, including joint stress leading to mucoid degeneration of the periarticular connective tissue with subsequent fluid accumulation and eventual cyst formation or stimulation of mucin secretion by mesenchymal cells in surrounding tissues. Ultimately, the coalescence of small pools of mucin is thought to result in the formation of the main cyst.
Ganglion cysts in the context of elite batsmen particularly affect the leading (non-dominant) wrist. They are more often seen on the volar aspect, which tends to be asymptomatic in most cases. However, when the cysts are seen on the dorsal aspect of the wrist, they may cause pain and discomfort. In cases of dorsal ganglion cysts, the pain is believed to result from the compression of the terminal branches of the posterior interosseous nerve and possible hemorrhage into the cyst. On MR, ganglion cysts typically appear as well-defined fluid-filled masses exhibiting low signal on T1-weighted images and high signal on T2-weighted images [Figure 9]. The cysts with a high protein content or hemorrhage tend to be isointense or hyperintense on T1-weighted images. In some cases, a narrow stalk or connection between the cyst and the joint may be visible on imaging.
- Ganglion cysts in the left wrist of a 31-year-old batsmen. (a and b) Sagittal and axial proton density fat-suppressed (PDFS) images reveal a multiloculated ganglion cyst on the dorsal aspect of the luno-capitate articulation along the dorsal scapholunate ligament (thick white arrow). (c and d) A ganglion cyst is seen along the volar radioscapholunate ligament (dotted white arrow). (e) Sagittal PDFS images reveal a ganglion cyst at the piso-triquetral articulation (dotted white arrow).
CARPAL BOSSING
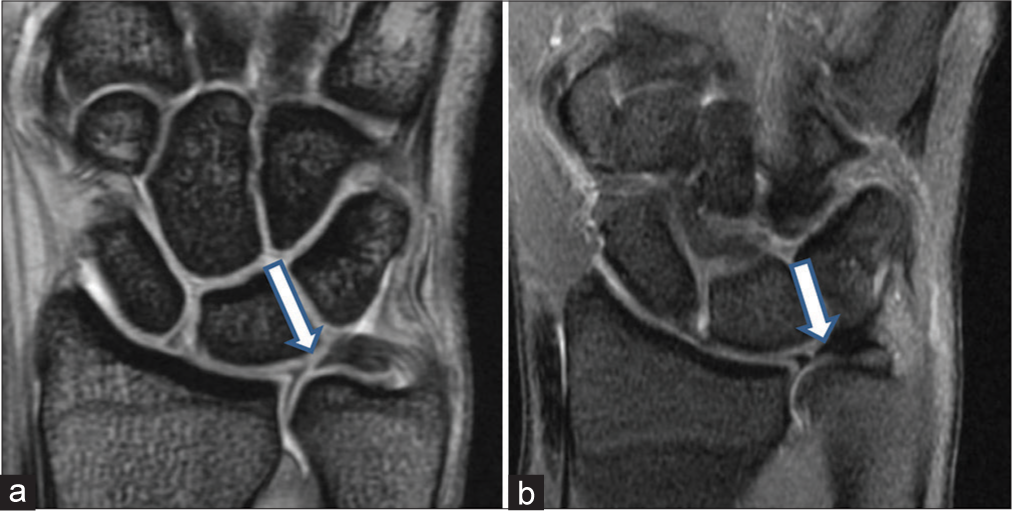
Carpal bossing refers to a bony protuberance appearing between the base of the second and third metacarpals, the capitate, and the trapezoid on the dorsal aspect of the wrist, this articulation is termed as quadrangular joint.[20] The exact etiology of the carpal boss is not fully understood, but it is associated with several factors, including joint instability, degeneration, trauma, an accessory ossicle, and partial or complete osseous coalition.
The symptoms associated with carpal bossing typically result from tenosynovitis of the extensor carpi radialis longus and brevis tendons as they insert on the dorsal aspect of the second and third metacarpals. Diagnosis of carpal bossing is primarily made through clinical examination and imaging findings after ruling out other potential differential diagnoses, with ganglion cysts being the most common cause of dorsal wrist protuberances.[21] Carpal bossing can be differentiated from ganglion cysts based on location and palpation. Approximately 60% and 70% of all ganglion cysts occur over the scapholunate ligament,[21] whereas carpal bossing is always over the quadrangular joint. Ganglions are mucin-filled cystic lesions that can be transilluminated, while carpal bossing has a hard, bony consistency.[22] Dorsal ganglia may resolve spontaneously in about 58% of cases, while carpal bossing is an osseous prominence and does not remit spontaneously.[23]
Carpal bossing may be diagnosed on plain X-rays, and if it is negative, a CT or MRI should be performed to exclude carpal bossing. MRI is the imaging modality of choice in such patients as it also provides detailed visualization of associated bone marrow edema, soft-tissue edema, tendon abnormalities, and any potential fractures [Figure 10].
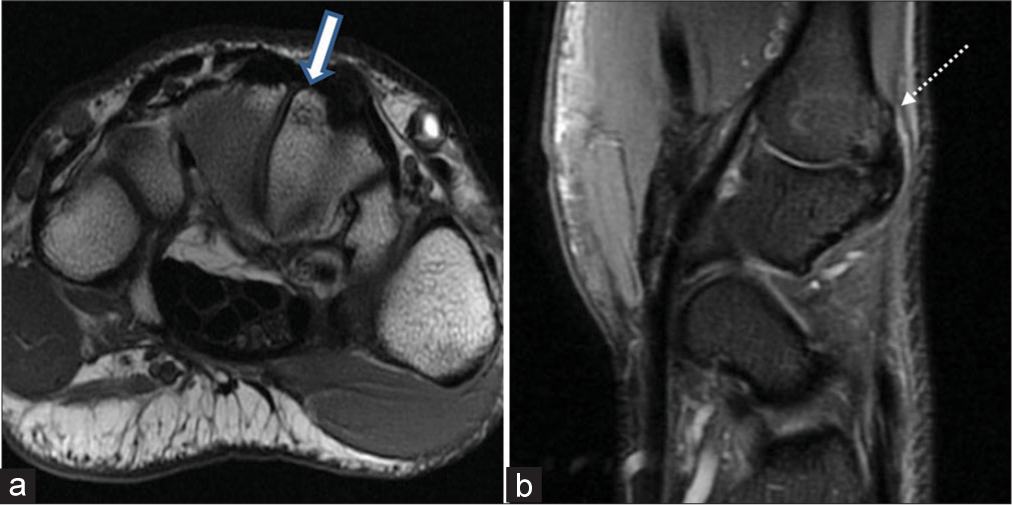
- Carpal bossing in a 34-year-old male with pain on the dorsal aspect of the non-dominant wrist. A hypertrophied bony protuberance is seen on the dorsal (a) aspect of the trapezoid bone (thick white arrow) and the base (b) of the 2nd metacarpal (dotted white arrow) suggestive of bone bossing. Mild dorsal capsular hypertrophy is also noted. No extensor tendinitis seen.
CONCLUSION
Understanding the biomechanics of a batsman’s swing and being aware of the specific injury patterns and pathologies that can occur in both the leading (non-dominant) and trailing (dominant) wrists are crucial for diagnosing and managing wrist injuries effectively in cricketers. Preventive measures, including proper batting technique, equipment selection (e.g., appropriate grips and gloves), and conditioning programs, can help reduce the risk of wrist injuries. Rehabilitation protocols tailored to the specific injury and the demands of cricket can aid in the early recovery and return to play.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- International consensus statement on injury surveillance in cricket: A 2016 update. Br J Sports Med. 2016;50:1245-51.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of hand and wrist injuries in sports. Hand Clin. 1990;6:379-81.
- [CrossRef] [PubMed] [Google Scholar]
- Injuries in Australian cricket at first class level 1995/1996 to 2000/2001. Br J Sports Med. 2002;36:270-4.
- [CrossRef] [PubMed] [Google Scholar]
- Measures to prevent cricket injuries: An overview. Sports Med. 1999;28:263-72.
- [CrossRef] [PubMed] [Google Scholar]
- The load on the radius and ulna in different positions of the wrist and forearm. A cadaver study. Acta Orthop Scand. 1984;55:363-5.
- [CrossRef] [PubMed] [Google Scholar]
- Athletic injuries of the wrist and hand. Part I: Traumatic injuries of the wrist. Am J Sports Med. 2003;31:1038-48.
- [CrossRef] [PubMed] [Google Scholar]
- Hook of hamate fractures in competitive baseball players. Hand (N Y). 2013;8:302-7.
- [CrossRef] [PubMed] [Google Scholar]
- Carpal fractures in athletes excluding the scaphoid. Hand Clin. 2009;25:371-88.
- [CrossRef] [PubMed] [Google Scholar]
- Finger tendon rupture secondary to fracture of the hamate. A case report. Acta Orthop Scand. 1985;56:96-7.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71:1202-7.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic signs of hook of hamate fracture: Evaluation of diagnostic utility. Skeletal Radiol. 2019;48:1891-8.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of hamate bone fractures in conventional X-rays and high-resolution computed tomography. An in vitro study. Invest Radiol. 1999;34:46-50.
- [CrossRef] [PubMed] [Google Scholar]
- The wrist In: Rogers LF, ed. Radiology of skeletal trauma (3rd ed). Philadelphia, PA: Churchill Livingstone; 2002. p. :839-41.
- [Google Scholar]
- The prevalence, variety and impact of wrist problems in elite professional golfers on the European Tour. Br J Sports Med. 2013;47:1075-9.
- [CrossRef] [PubMed] [Google Scholar]
- Overuse injuries and burnout in youth sport: A position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48:287-8.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiologic investigation of 1394 feet: Coincidence of hindfoot malalignment and Achilles tendon disorders. Foot Ankle Surg. 2012;18:119-23.
- [CrossRef] [PubMed] [Google Scholar]
- Pitfalls that may mimic injuries of the triangular fibrocartilage and proximal intrinsic wrist ligaments at MR imaging. Radiographics. 2011;31:63-78.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging interpretation of the Palmer classification of triangular fibrocartilage complex lesions. Radiographics. 1996;16:97-106.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of carpal boss and osseous coalition: An anatomic study. J Hand Surg Am. 2009;34:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging in the diagnosis of occult dorsal wrist ganglions. J Hand Surg Eur Vol. 2008;33:595-9.
- [CrossRef] [PubMed] [Google Scholar]
- The carpal boss: Review of diagnosis and treatment. J Hand Surg Am. 2008;33:446-9.
- [CrossRef] [PubMed] [Google Scholar]
- The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007;32:502-8.
- [CrossRef] [PubMed] [Google Scholar]







