Translate this page into:
Prevalence and characteristics of fabella in the Indian population – A radiograph-based prospective cross-sectional study

*Corresponding author: Pushkar Mendiratta, Department of Radiodiagnosis and Imaging, Military Hospital Mathura, Mathura, Uttar Pradesh, India. pushkar_indian@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Mendiratta P, Bhattacharjee S, Das DS, Kumar R. Prevalence and characteristics of fabella in the Indian population – A radiograph-based prospective cross-sectional study. Indian J Musculoskelet Radiol. doi: 10.25259/IJMSR_5_2024
Abstract
Objectives
Fabella is a sesamoid bone in the tendon of lateral head of gastrocnemius, whose prevalence data are based on Asian and Western population studies with no prevalence data reported in Indian population. The present study aimed to examine plain knee radiographs in the Indian population, document prevalence and characteristics of fabella, and analyze its variations with age and gender. The presence of fabella with posterolateral knee pain was also correlated.
Material and Methods
This was a prospective cross-sectional study with all consecutive patients undergoing bilateral knee radiographs included in the study. Prevalence and characteristics of fabella were documented; significance of its presence with respect to age, gender; and laterality was calculated; and relationship with the presence of posterolateral knee pain was analyzed.
Results
968 consecutive patients were enrolled with mean age of the subjects being 50 ± 16 years. The prevalence of fabella was maximum in the age group 51–60 years (41%). Overall prevalence of fabella was 27.05%. Posterolateral knee pain was present in 16.9% subjects, out of which fabella was present in 35.7%. The size of the fabella, however, was significantly larger in patients with posterolateral knee pain.
Conclusion
The prevalence of fabella in our study was less than what is reported for the Asian population. The presence of fabella did not have a significant relationship with posterolateral knee pain; however, its size in such patients was significantly larger, highlighting its role in posterolateral corner pathologies.
Keywords
Cross-sectional study
fabella
fabella syndrome
Posterolateral knee pain
Prevalence
INTRODUCTION
The fabella is a sesamoid bone located in the lateral head of gastrocnemius tendon and is represented in Figure 1. It also goes by the name of “sesamum genu superius laterale.” Very rarely, it has been reported in the medial head of gastrocnemius muscle.[1,2] Fabella’s prevalence with age, gender, its size, osseous/cartilaginous nature, and even unilateral or bilateral presence is very variable with wide variations in each parameter reported in literature. Its reported prevalence varies from 3% to 87% while its size has been reported to range from pinpoint to up to 30 mm.[3,4]
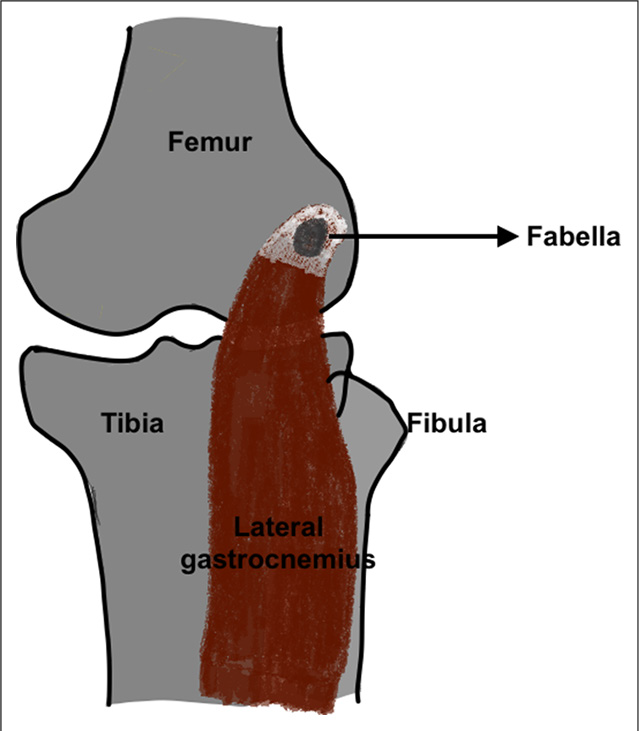
- Schematic representation of the posterior view of the knee joint illustrating fabella in the tendon of the lateral head of gastrocnemius.
Fabella, like most sesamoid bones, assists in muscle action with a possible biomechanical function. It is stabilized in its position by the fabellofibular ligament connecting its distal end to the fibular head.[5,6] Unsurprisingly, it is associated with several pathologies including fabella syndrome, characterized by posterolateral knee pain and a snapping or grating sensation, during extension of the knee.[7,8] Other pathologies associated with it include fabellar fracture, fabellar dislocation, osteoarthritis, peroneal nerve, and popliteal artery compression.[9-14]
Fabella is commonly encountered on knee radiographs, as depicted in Figure 2a-c. It may occasionally resemble intra-articular loose bodies, osteophytes, intra-meniscal calcifications, fracture fragments, popliteal artery calcification, and cyamella, a sesamoid bone within the popliteal tendon.[5,9]
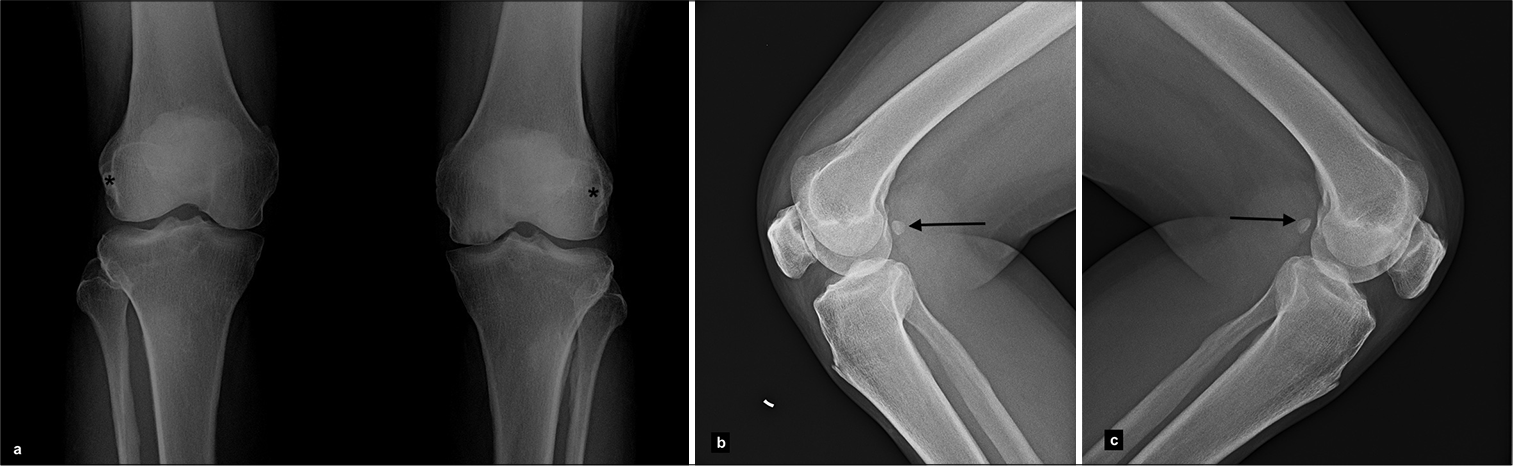
- (a) Radiograph anteroposterior view (b and c) lateral view of both knees in a subject shows fabella present bilaterally (black asterix in a and black arrows in b and c).
In view of the pathological conditions associated with fabella, it becomes imperative for the radiologist and the treating clinician alike to be aware of its prevalence, along with its normal anatomic and imaging characteristics. There have been literature studies on fabella prevalence in predominantly Asian and Western populations. Till date, its prevalence in Indian population has not been reported. This prospective study aimed to examine plain knee radiographs to determine fabella prevalence and investigate its variations with respect to age, gender, pattern of symmetry, and its relationship with the presence of posterolateral knee pain.
MATERIAL AND METHODS
This was a prospective cross-sectional study conducted between October 2020 and December 2021. The study was approved by the institutional ethical committee and was carried out according to the principles of the Declaration of Helsinki. All patients were included in the study after their written and informed consent. All consecutive patients reporting to the Department of Radiology for bilateral knee radiographs - anteroposterior (AP) and lateral views were included in the study. Patients for whom a single view was done or a single knee radiographed were not included in the study. A total of 968 consecutive patients who reported for bilateral knee radiographs were included in the study.
Patients with findings of knee osteoarthritis (Kellgren and Lawrence grade 3 and 4) were excluded to avoid confusion between osteophytes/loose bodies and fabella. Patients with trauma and fractures around the knee were also excluded to avoid confusion with bone fragments.
Radiographs were taken with standard exposure factors with the lateral view done in 45° flexion. All radiographs were done on a 300 mAs radiography machine. The images were processed on a single-loading computerized radiography system and reviewed by a single radiologist with 6 years of experience. Patient data including age, gender, presence of posterolateral knee pain, associated clinical features such as pain on extension of knee, snapping sensation if any, were documented. The size in all three dimensions, AP, transverse (TR), and craniocaudal (CC) measurements were measured in millimeters (mm) as shown in Figure 3. The presence of fabella in unilateral or bilateral knees was noted. Any other finding on the knee radiographs was also documented.
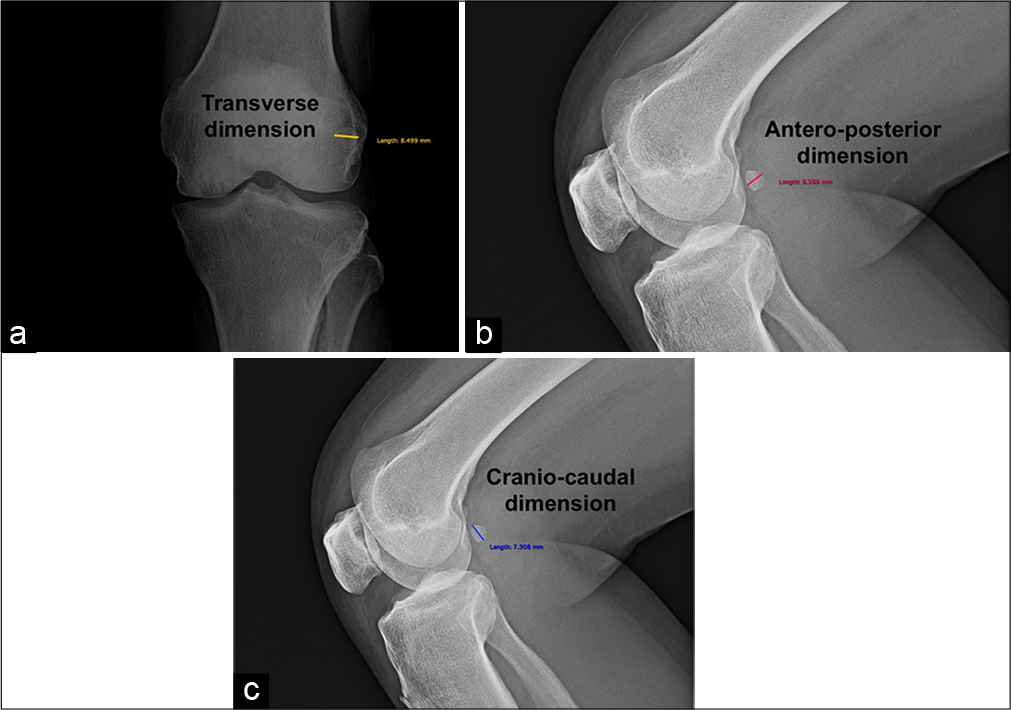
- Radiograph anteroposterior view and lateral views of the same subject showing technique of measurement of the fabella in (a) transverse dimension, (b) anteroposterior dimension, and (c) craniocaudal dimension.
The statistical analysis was performed by MS Excel (2018) and STATA 11.2 (College Station TX USA). The distribution of presence of fabella with respect to the age of subjects was expressed as mean ± standard deviation. Gender distribution, prevalence of fabella, and presence of posterolateral knee pain were expressed as frequency and percentage. The association of gender with the presence of fabella and significance of the presence of fabella in patients with posterolateral knee pain were measured using Pearson’s Chi-square test. Student t-test was performed to determine the significance of gender on the size of fabella. A two-sample independent t-test compared the mean sizes of fabella in patients with and without posterolateral knee pain. P < 0.05 was deemed to be statistically significant.
RESULTS
968 consecutive patients reported to the Department of Radiology for bilateral knee radiographs during the study period, out of which 10 patients with gross osteoarthritic changes were excluded. The age of the study subjects ranged from 1 to 88 years with mean of 50 ± 16 years. The study subjects were distributed into age groups at 10-year interval. Maximum subjects were in the age group 51– 60 years (n = 282, 29.47% of total subjects) and minimum subjects in the age group 81–90 years (n = 14, 1.45% of total subjects). The presence of fabella among various age groups is summarized in Table 1. Age group of 1–10 years (n = 23, 2.42% of subjects) has not been included in the summary since ossification of fabella has not been described in this age group. The presence of the fabella was maximum in the age group 51–60 years with a prevalence of 41% (n = 116). A Chi-square test for trend showed non-linear relationship between the age and the presence of fabella with a P < 0.0001 (P < 0.05 was taken as significant)
| Age group (years) | Number of subjects (n) | Percentage of subjects | Prevalence of fabella | Number of subjects with fabella (n) | Odds ratio |
|---|---|---|---|---|---|
| 11–20 | 37 | 3.86 | 25 | 9 | 0.87 |
| 21–30 | 23 | 2.42 | 20 | 5 | 0.75 |
| 31–40 | 167 | 17.39 | 19 | 32 | 0.64 |
| 41–50 | 208 | 21.74 | 18 | 37 | 0.58 |
| 51–60 | 282 | 29.47 | 41 | 116 | 1.89 |
| 61–70 | 162 | 16.91 | 29 | 46 | 1.07 |
| 71–80 | 42 | 4.35 | 22 | 9 | 0.4 |
| 81–90 | 14 | 1.45 | 33 | 5 | 1.5 |
36% (n = 345) of the study subjects were males and 64% (n = 613) were females. Overall prevalence of fabella was 27.05% (n = 259). Fabella was present in 29.8% (n = 103) of males while it was present in 25.4% (n = 156) of females. Chi-square test of independence revealed no significant difference in the prevalence of fabella between males and females, X2 (1, n = 958) = 2.1729, P = 0.140458 (P < 0.05 was taken as significant). 15.46% (n = 148) of total subjects had fabella in bilateral knees, 6.28% (n = 60) in right knee only while 5.31% (n = 51) in left knee only. There was no significant difference between the right and left-sided prevalence of the fabella, when present unilaterally, as demonstrated by Chi-square test with a P = 0.3761 (P < 0.05 was taken as statistically significant).
The mean AP size of fabella was 5 ± 2.1 mm, mean TR size was 6.9 ± 2.7 mm, and mean CC size was 8.5 ± 3.6 mm. The mean size in all three dimensions was noted to be larger in males as compared to females. Student t-test showed significant effect of gender on the size of fabella, t(956) = 3.243, P = 0.001 (P < 0.05 was taken as significant). The mean sizes of fabella in the three dimensions in males and females are summarized in Table 2.
| Gender | Anteroposterior dimension (AP) ± SD (mm) | Transverse dimension (TR) ± SD (mm) | Craniocaudal dimension (CC) ± SD (mm) |
|---|---|---|---|
| Males | 5.1±2.1 | 7.3±3.3 | 9.3±3.6 |
| Females | 4.9±2.2 | 6.7±2.0 | 8.1±3.6 |
| Overall mean | 5±2.1 | 6.9±2.7 | 8.5±3.6 |
SD: Standard deviation
16.9% (n = 162) subjects complained of posterolateral knee pain. Out of these, 35.7% (n = 58) of subjects had fabella present while 64.3% (n = 104) did not have fabella present on radiographs. Chi-square test of independence demonstrated no significant association between presence of fabella on radiographs and presence of posterolateral knee pain, X2 (1, n = 958) = 7.5966, P = 0.005848 (P < 0.05 was taken as significant). The mean size of fabella in patients with posterolateral knee pain was 5.7 ± 2.4 mm (AP), 8.2 ± 3.1 mm (TR), 9.7 ± 4 mm (CC) while in those without posterolateral knee pain was 4.4 ± 1.6 mm (AP), 5.8 ± 1.6 mm (TR), and 7.6 ± 2.7 mm (CC). Two sample independent t-test illustrated this difference to be statistically significant, t(956) = 10.3247, P ≤ 0.0001 (P < 0.05 was taken as significant). The presence of posterolateral knee pain with respect to the presence of fabella is summarized in Table 3.
| Posterolateral knee pain | Subjects | Number (n) | Percentage | |
|---|---|---|---|---|
| Present | Total | 162 | 16.9 | |
| Fabella present | 58 | 35.7 | ||
| Fabella absent | 104 | 64.3 | ||
| Absent | Total | 796 | 83.1 | |
| Fabella present | 201 | 25.3 | ||
| Fabella absent | 595 | 74.7 | ||
DISCUSSION
Sesamoid bones are focal areas of ossifications within tendons or muscles. They protect the tendons and assist muscle action by relieving tension within them or by altering their direction of pull reducing friction or by allowing increased weight-bearing. Like most sesamoid bones, fabella starts as cartilaginous foci, undergoes endochondral ossification till age 10, and then, calcifies and ossifies by age 12–15 years. The development of sesamoid bones has been explained by phylogenetic theory highlighting the role of genetic intrinsic factors or by functional theory which suggests its formation from mechanical stress on a tendon.[15-17] Fabella lies at the point of confluent forces, formed by the terminal end of the lateral head of gastrocnemius tendon, the arcuate ligament, the oblique popliteal, and the fabellofibular ligaments.[18,19]
Fabella prevalence data are lacking in Indian population with literature search showing two Indian studies done on human adult cadavers for morphological analysis of gastrocnemius muscle and plantaris muscle, documenting fabella in 13.3% and 12.5% cases, respectively.[20,21] Fabella prevalence reported globally varies from 3% to 87% with the highest rates reported in Asian and Oceanian populations.[22,23] The prevalence of fabella noted in our study was 27.05%, similar to that reported in Western literature, while much less than that reported in Asian and Oceanic population. Phylogenetic theory of intrinsic genetic factors coupled with frequent kneeling and squatting habits causing prolonged contact and strain of the fabella against posterior aspect of lateral femoral condyle has been postulated as the cause for increased fabella prevalence in Asian populations.[1,3,22] The high prevalence in the Oceanian population has been postulated to be either an overestimate or due to the valgus knee alignment.[22]
The prevalence of fabella in our study showed no statistically significant gender-based difference as reported previously.[1,22,24,25] In our study, fabella was present in 15.46% of the subjects bilaterally, in 6.28% on the right and in 5.31% subjects on the left. These rates are similar to those reported previously[22,23,26] with some differences between right-sided or left-sided prominence.[27,28] In our study, fabella was found to be significantly larger in size in males as compared to females, which can be attributed to biomechanical dynamics including body weight, muscle mass, and physical activity, as reported previously.[23,24,29]
Size of the fabella may also play a role in its associated pathologies, by causing compression of adjacent structures.[14,30] However, no definite cut-off or critical value for size has been described in this context. Fabellar size as documented in literature varies in a wide range, while its size in our study was 5 ± 2.1 mm (AP), 6.9 ± 2.7 mm (TR) and 8.5 ± 3.6 mm (CC). In our study, the prevalence of fabella had a non-linear relationship with increasing age as also reported previously.[1,23-25,31] Few studies however have reported positive correlation of fabella with age.[22,32-34]
The posterolateral corner knee pain in fabella syndrome is due to mechanical irritation of soft tissues or compression of adjacent structures.[13,15] The present study revealed no significant association of fabella with posterolateral knee pain. Since this was a radiograph-based study, other causes of posterolateral knee pain such as meniscal injuries, ligamental injury, bursitis, and tendinitis could not be evaluated.[22,26] Significant association between the fabella and posterolateral knee pain has however been previously reported.[29] In the present study, mean fabellar size in patients with posterolateral knee pain was significantly larger than those without knee pain, implying a radiographically detected large fabella in a patient with posterolateral knee pain may be an indicator of fabella syndrome. Since positive correlation of fabella with age has also been reported, age and size may both act as confounding factors for posterolateral knee pain. Our study was limited being a radiograph-based study, wherein the relationship of fabella with posterolateral knee pain could not be ascertained. MRI would be required to confirm this association.
There were few other limitations of our study. Being a radiograph-based study, only the ossified fabella was identified, which may have underestimated the prevalence. Further MRI-based studies may be warranted to find the prevalence of fabella in Indian population. Although the study recruited a statistically significant sample size, fabella prevalence may still vary within Indian population based on ethnicities and varying physical habits of geographically and culturally different regions, which may have an effect on the growth of fabella.
CONCLUSION
The prevalence of fabella in our study, the first such study in Indian population, was 27.05%, similar to that reported in Western populations but lower than those reported in Asian and Oceanic populations. There was no significant association of fabella with age; however, males had significantly larger fabella than females substantiating its biomechanical function. Our study also determined that there was no significant association between the presence of fabella with posterolateral knee pain, though its size in patients with posterolateral knee pain was significantly larger. Knowledge of these fabella characteristics would definitely help the clinicians and radiologists alike in diagnosing patients with posterolateral knee pain and other pathologies that may be associated with fabella.
Ethical approval
The research/study was approved by the Institutional Review Board at Nayati Multi Superspeciality Hospital, Mathura, number IEC07102020, dated 7th October, 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Prevalence and distribution of the fabella: A radiographic study in Turkish subjects. Folia Morphol (Warsz). 2017;76:478-83.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical variations in the anatomy of the posterolateral corner of the knee. Knee Surg Sports Traumatol Arthrosc. 2007;15:895-900.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and radiological characteristics of fabellae in an Asian population. Singapore Med J. 2014;55:198-201.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic enlarged fabella. BMJ Case Rep. 2016;2016:bcr2016218085.
- [CrossRef] [PubMed] [Google Scholar]
- Unraveling the posterolateral corner of the knee. Radiographics. 2016;36:1776-91.
- [CrossRef] [PubMed] [Google Scholar]
- Posterolateral supporting structures of the knee: Findings on anatomic dissection, anatomic slices and MR images. Eur Radiol. 2001;11:2170-7.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging, MR arthrography, and specimen correlation of the posterolateral corner of the knee: An anatomic study. AJR Am J Roentgenol. 2003;180:1095-101.
- [CrossRef] [PubMed] [Google Scholar]
- Does the prevalence of ossified fabella vary in knee osteoarthritis and age-related degeneration? A meta-analysis of about 11000 knees. Cureus. 2021;13:e12535.
- [CrossRef] [Google Scholar]
- Fabella fracture with radiological imaging: A case report. Trauma Case Rep. 2017;12:19-23.
- [CrossRef] [PubMed] [Google Scholar]
- Dislocation of an enlarged fabella as uncommon cause of knee pain: A case report. Knee. 2007;14:330-2.
- [CrossRef] [PubMed] [Google Scholar]
- Compression neuropathy of the common peroneal nerve by the fabella. BMJ Case Rep. 2013;2013:bcr2013202154.
- [CrossRef] [PubMed] [Google Scholar]
- Fabella syndrome and common peroneal neuropathy following total knee arthroplasty. Case Rep Orthop. 2021;2021:7621844.
- [CrossRef] [PubMed] [Google Scholar]
- A case report on a very rare variant of popliteal artery entrapment syndrome due to an enlarged fabella associated with severe knee osteoarthritis. J Orthop Sci. 2017;22:164-8.
- [CrossRef] [PubMed] [Google Scholar]
- Coincident development of sesamoid bones and clues to their evolution. Anat Rec. 1999;257:174-80.
- [CrossRef] [Google Scholar]
- A new insight into the fabella at knee: the foetal development and evolution. Folia Morphol (Warsz). 2017;76:87-93.
- [CrossRef] [PubMed] [Google Scholar]
- The role of movement in embryonic joint development. Dev Biol. 1966;14:401-20.
- [CrossRef] [Google Scholar]
- Fabellar snapping as a cause of knee pain after total knee replacement: Assessment using dynamic sonography. AJR Am J Roentgenol. 2004;183:352-4.
- [CrossRef] [PubMed] [Google Scholar]
- The fabella syndrome-a rare cause of posterolateral knee pain: A review of the literature and two case reports. BMC Musculoskelet Disord. 2014;15:100.
- [CrossRef] [PubMed] [Google Scholar]
- Morphological analysis of proximal gastrocnemius muscle-a study in thirty adult human cadavers. Int J Anat Radiol Surg. 2016;5:41-3.
- [Google Scholar]
- The Ethnic and geographical distribution of fabella: A systematic review and meta-analysis of 34,733 knees. Cureus. 2021;13:e14743.
- [CrossRef] [Google Scholar]
- The morphology of fabella and its prevalence in Turkish society. Eur Rev Med Pharmacol Sci. 2022;26:1164-9.
- [Google Scholar]
- The incidence and structure of the fabella in a South African cadaver sample. Clin Anat. 2011;24:84-90.
- [CrossRef] [PubMed] [Google Scholar]
- Human biological variation in sesamoid bone prevalence: The curious case of the fabella. J Anat. 2020;236:228-42.
- [CrossRef] [PubMed] [Google Scholar]
- Fabella and patella variants: Radiographic prevalence, distribution and clinical relevance in a population of black african descent. Anat Cell Biol. 2021;54:184-92.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of fabella and its relationship with the lateral posterior condylar offset and lateral posterior tibial slope values. Jt Dis Relat Surg. 2022;33:588-98.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of the fabella and its association with pain in the posterolateral corner of the knee: A cross-sectional study in a Romanian population. Medicine (Baltimore). 2018;97:e13333.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of fabella syndrome with manual therapy: A case report. J Orthop Sports Phys Ther. 2003;33:33-9.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of a fabella in the gastrocnemius muscle on the common fibular nerve in Japanese subjects. Clin Anat. 2013;26:893-902.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of fabella in Turkish population and the association between the presence of fabella and osteoarthritis. SN Compr Clin Med. 2021;3:805-11.
- [CrossRef] [Google Scholar]
- Fabellar prevalence, degeneration and association with knee osteoarthritis in the Chinese population. Sci Rep. 2019;9:13046.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between fabella and posterolateral knee pain and common peroneal nerve injury. Zhongguo Gu Shang. 2020;33:1071-5.
- [Google Scholar]







