Translate this page into:
Progressively Increasing Teres Minor Calcific Tendinopathy in an Elderly Male

*Corresponding author: Abhinav Aggarwal, Department of Radiology, Mata Chanan Devi Hospital, Janak Puri, New Delhi - 110 058, India. abhinavagg@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aggarwal A, Singbal SB. Progressively Increasing Teres Minor Calcific Tendinopathy in an Elderly Male. Indian J Musculoskelet Radiol 2021;3(1):54-6.
Abstract
Calcific tendinopathy is a common pathology involving a variety of tendons across many joints. It is most commonly seen involving tendons of the rotator cuff with supraspinatus being the favorite. It can mimic aggressive pathologies such as neoplasms resulting in unnecessary interventions. Rarely, it involves teres minor tendon. We report a case of teres minor calcific tendinopathy detected over serial radiographs and diagnosed using magnetic resonance imaging.
Keywords
Calcific tendinopathy
Magnetic resonance imaging
Shoulder
Teres minor
INTRODUCTION
Calcific tendinopathy is a common pathology involving a variety of tendons across many joints. There is minor female predilection. It is most commonly seen involving tendons of rotator cuff. Teres minor is the rarest tendon involved. Etiologically it has been hypothesized that hypoxia induces fibrocartilagenous metaplasia of the critical zone. It can mimic aggressive pathologies like neoplasms resulting in unnecessary interventions.
CASE REPORT
An otherwise healthy retired 70-year-old male presented with pain in the left shoulder with a limited range of movements. The patient was advised radiograph of the left shoulder joint. It revealed a faint calcification posterior to the shoulder joint in the region of infraspinatus/teres minor [Figure 1a]. Since the patient was not relieved after 1 month of conservative treatment, also in accordance with the findings of serial radiographs [Figure 1b, which showed increase in density of calcification], the patient was advised a magnetic resonance imaging (MRI) scan of the left shoulder. MRI revealed extensive mineralization of teres minor tendon and musculotendinous junction suggestive of calcific tendinopathy [Figures 2a and b]. The patient also had full-thickness tears of supraspinatus and infraspinatus tendons along with severe tendinosis of subscapularis tendon.
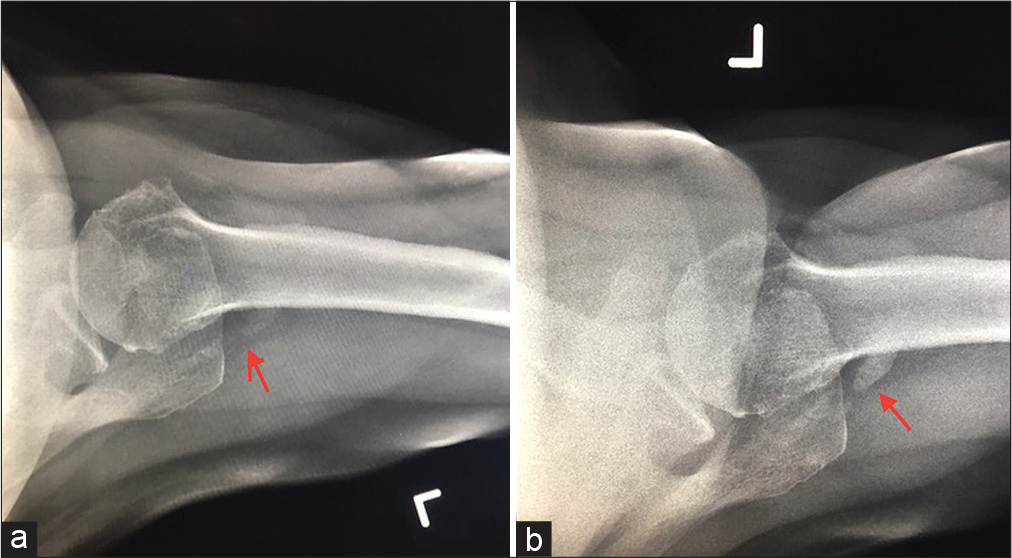
- Serial radiographs of left shoulder taken over a period of one-month show increased calcific opacity (red arrows) in rotator cuff region in posterior aspect of shoulder joint. The position of opacity suggests involvement of either infraspinatus or teres minor tendons, both of which are uncommon/rare.
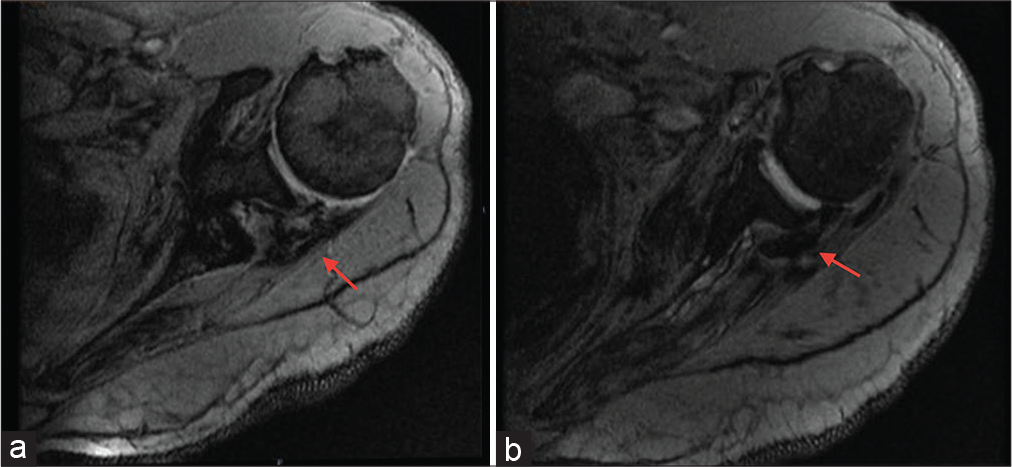
- Axial Medic images show hypointense signal in teres minor tendon and musculotendinous junction suggestive of mineralization (red arrows). Findings are consistent with diagnosis of calcific tendinopathy of teres minor.
DISCUSSION
Calcific tendinopathy has been described in the literature, but the involvement of teres minor is one of the rarest.[1] There is slight female predilection with fourth and fifth being the most common decades of life.[2] Shoulder and hip are the most commonly affected joints with supraspinatus, infraspinatus, pectoralis major, and gluteus maximum tendons being commonly involved.[3,4] Etiologically, it has been hypothesized that hypoxia induces fibrocartilaginous metaplasia of the critical zone, tissue necrosis, and trauma that can all contribute to the formation of intra-tendinous calcification, which is generally due to deposition of hydroxyapatite crystals.[2,5]
Two commonly accepted pathogenesis are the ones described by Moseley[6] and Uhtoff and Loehr.[6,7] Uhtoff and Loehr described the process of calcific tendinopathy into three phases, namely, precalcific, calcific, and postcalcific. The tenocytes undergo fibrous metaplasia and avascular necrosis during precalcific phase. The calcific phase further consists of three stages: Formative, resting, and resorptive. Calcium deposition takes place informative and resting stages, whereas in resorptive stage, spontaneous resorption of calcium takes place, which may result in the acute inflammatory response. During the post-calcific phase remodeling of the tendon by fibroblasts takes to place.[7] Moseley described the pathogenesis having two stages, initial silent phase and later hyperemic dissolution phase. Calcium deposition takes place during the initial phase, whereas calcium disseminates through the bursal lining leading to an acute inflammatory response.[6] Various risk factors associated are thyroid and estrogen metabolism disorders and lifestyle factors such as alcohol consumption and obesity.[8]
Various imaging modalities commonly used to image calcific tendinitis are radiographs, ultrasound, and MRI. Since these can lead to cortical erosions, it can be confused with various aggressive pathologies such as septic arthritis and neoplasm.[3,5,8] Serial radiographs showing an increase in size can mimic aggressive pathologies, like in our case. In our case, we saw significant increase over the course of 1 month. After an extensive review of the literature, we could not find any study describing about increase in quantification of teres minor calcification within a specific time frame. Laboratory markers of inflammation may be elevated during acute phases. Calcification can also be present in bursae, commonly due to extrusion from tendons. These are easily diagnosed using ultrasound rather than radiographs. MRI can also be used to image bursal calcifications, especially after intrathecal gadolinium injections.[9] Since the pathology is self-limiting, treatment is usually conservative. However, ultrasound can be used for guided lavage aspiration and needling/barbotage under local anesthesia. Computed tomography (CT) plays a limited role in the diagnosis of calcific tendinopathy and is rarely used for CT-guided shock wave lithotripsy.[10]
CONCLUSION
In our case, increasing the density of calcification on serial radiographs raised a suspicion of a sinister lesion; however, imaging with MRI helped incorrect diagnosis and avoided unnecessary biopsy. Our patient underwent tendon repair surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Infraspinatus and teres minor tendon calcification with severe pain. West Undergrad Res J. 2017;8:1-4.
- [CrossRef] [Google Scholar]
- Calcific tendinitis: A pictorial review. Can Assoc Radiol J. 2009;60:263-72.
- [CrossRef] [PubMed] [Google Scholar]
- Intraosseous migration of tendinous calcifications: Cortical erosions, subcortical migration and extensive intramedullary diffusion, a SIMS series. Skeletal Radiol. 2015;44:1403-12.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical localizations of calcific deposits in the shoulder. Int J Surg Case Rep. 2015;10:206-10.
- [CrossRef] [PubMed] [Google Scholar]
- Calcifying tendinitis In: Rocwood CA, Matsen FA, eds. The Shoulder. Philadelphia, PA: Saunders Company; 1998. p. :971-91.
- [Google Scholar]
- Calcific tendinitis: Natural history and association with endocrine disorders. J Shoulder Elbow Surg. 2007;16:169-73.
- [CrossRef] [PubMed] [Google Scholar]
- Migration of calcium deposits into subacromial-subdeltoid bursa and into humeral head as a rare complication of calcifying tendinitis: Sonography and imaging. J Ultrasound. 2015;18:259-63.
- [CrossRef] [PubMed] [Google Scholar]
- Calcific tendinitis of the rotator cuff: State of the art in diagnosis and treatment. J Orthop Traumatol. 2016;17:7-14.
- [CrossRef] [PubMed] [Google Scholar]







