Translate this page into:
Subchondral Osteoid Osteoma of a Metatarsal Bone: An Uncommon Variant in an Unusual Location

*Corresponding author: Saurabh Maheshwari, Department of Radiodiagnosis and Imaging, Armed Forces Medical College, Pune, Maharashtra, India. saurabhmhshwr@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Shet A, Grewal DS, Maheshwari S, Bhanu KU. Subchondral Osteoid Osteoma of a Metatarsal Bone: An Uncommon Variant in an Unusual Location. Indian J Musculoskelet Radiol 2020;2(2):140-3.
Abstract
Osteoid osteoma (OO) is a benign bone-forming lesion leading to classical symptoms in the form of pain that aggravates during the night and is relieved by the treatment with salicylates. It constitutes 10% of benign skeletal neoplasms and is seen most often in males between the age group of 7 and 25 years. We report a rare case of subchondral OO of a metatarsal bone with unusual imaging features. This case illustrates the limitations of various imaging modalities in the diagnosis of bone tumors and the need for biopsy and histopathological analysis in difficult cases.
Keywords
Osteoid osteoma
Bone tumor
Foot
Metatarsal
Benign bone tumor
INTRODUCTION
Osteoid osteoma (OO) is a benign bone-forming lesion, leading to classical symptoms in the form of pain that aggravates during the night, and is relieved by the treatment with salicylates. It constitutes 10% of benign skeletal neoplasms and is seen most often in the males between the age group of 7 and 25 years. We report a rare case of subchondral OO of a metatarsal bone with unusual imaging features.
CASE REPORT
A 26-year-old otherwise healthy male presented with a 5-month history of the right lateral forefoot pain on weight-bearing. He gave the history of travel to a high-altitude region for 3 months duration before the onset of symptoms. His pain was progressively worsening but there was no history of aggravation at night. The pain was relieved by taking nonsteroidal anti-inflammatory drugs (NSAIDs). He repudiates any history of trauma. There was no increase in pain on the activity. Medical and surgical history was not contributory.
On physical examination, fullness and tenderness were noted in the fourth intermetatarsal space. There was tenderness over the fifth metatarsal head with painful movements at the fifth metatarsophalangeal (MTP) joint. There was no neurovascular compromise. The remainder of the local and systemic examination was within normal limits. The patient underwent imaging with a clinical suspicion of chilblains raised by the treating orthopedic surgeon.
Plain radiographs of the right foot revealed a well-defined small lytic lesion with a sclerotic rim over the lateral aspect of the head of the fifth metatarsal. This was associated with a smooth defect in the lateral cortical margin. No mineralization was apparent in this lucent area or the adjacent soft tissue. There was no periosteal reaction or associated soft-tissue component. The lesion was not involving the adjacent joint [Figure 1].
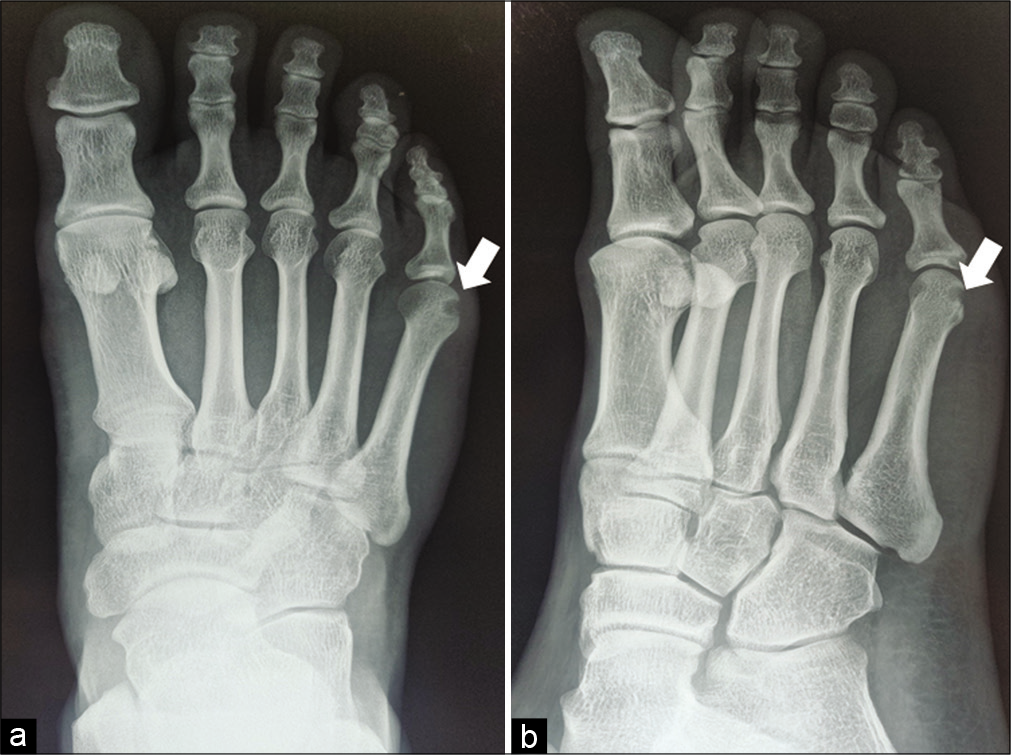
- Radiograph of the right foot anteroposterior (a) and oblique (b) views demonstrates a well-defined small lytic lesion (solid white arrows) with sclerotic border over the lateral aspect of the head of the fifth metatarsal showing a smooth defect at the lateral cortical margin. No mineralization was apparent in this lucent area or in the surrounding soft tissue.
For a better characterization of the lesion, a magnetic resonance imaging (MRI) scan was done for the right foot. It showed a 6 mm size well-defined focal lesion involving the posterolateral aspect of the head of 5th metatarsal. The core of the lesion was hypointense on T1-weighted image (WI), mildly hyperintense on short inversion time inversion recovery (STIR) images, and isointense on proton density fat-suppressed (PDFS) images and showed subtle post-contrast enhancement. The lesion had a thin hypointense rim at its interface with the bone consistent with sclerosis. Perilesional bone marrow edema was noted in the head and shaft of the 5th metacarpal in form of PDFS and STIR hyperintensity [Figure 2]. Following MRI possible diagnoses of a subchondral cyst, solitary juxta-articular erosion of gout and a benign bone tumor (chondromyxoid fibroma or OO) was considered. A serum uric acid level test showed normal levels excluding gout.

- Magnetic resonance imaging images of the right foot in coronal plane show a 6 mm size well-defined subchondral focal lesion involving the posterolateral aspect of the head of the 5th metatarsal which appears uniformly hypointense on T1-weighted image (solid white arrow in a). Central part of the lesion appears hyperintense on short inversion time inversion recovery (STIR) (b) and proton density fat-suppressed (PDFS) (c) images. It shows subtle post-contrast enhancement on T1 fat-saturated post-contrast images (d). The lesion shows a thin hypointense rim (small black arrowhead in b) around it on all sequences consistent with the sclerosis. Perilesional bone marrow edema is seen in the head and shaft of the 5th metacarpal in form of PDFS and STIR hyperintensity (void white arrow in b and c).
A limited computed tomography (CT) scan of the lesion for further characterization showed a sharply defined lytic lesion in the subchondral location. The lateral margin of the lesion showed a cortical breach. The rest of the margins showed a thin rim of sclerosis. The margins of the lesion appeared to be overhanging at a few places [Figure 3]. There was no mineralization seen within the lesion.
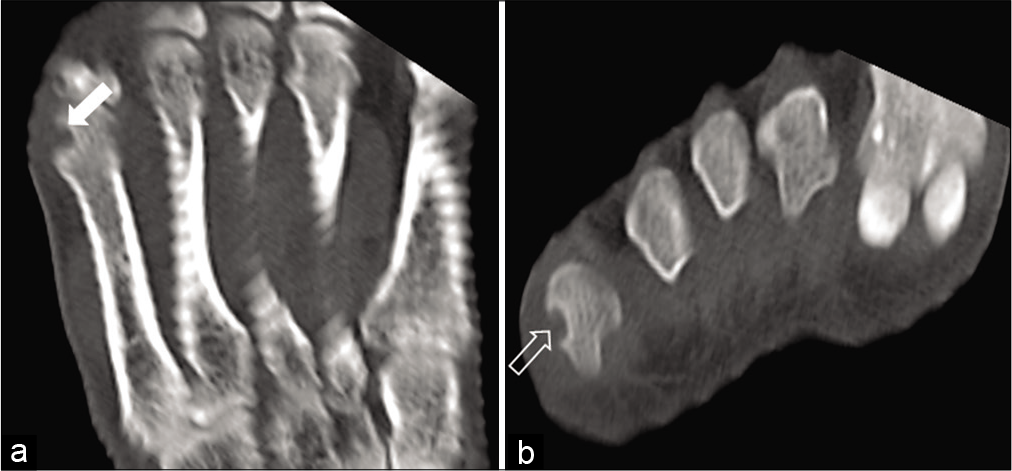
- Computed tomography images of the right foot in coronal (a) and axial (b) planes in bone window showing the subchondral location of the lesion surrounded by a thin rim of sclerosis (solid white arrow in a). Laterally, there is a smooth cortical defect (void white arrow in b) with overhanging margin.
Based on imaging findings, differential diagnosis of a subchondral cyst or a benign bone tumor was proposed. The patient underwent CT-guided core needle biopsy from the lesion. The biopsy was performed using the burr-down technique. There were no intra- or post-procedural complications. On histopathological examination, the lesion demonstrated mature cartilage with a central network of interlacing osteoid trabeculae that were variably mineralized and were surrounded by mature bone at the periphery. This was embedded in a hypocellular fibrovascular connective tissue. These histopathological findings confirmed the diagnosis of OO [Figure 4].

- Photomicrograph of histopathological section of the lesion. (a) Low-power photomicrograph of the resected nidus from the patient with hematoxylin and eosin staining demonstrates the abundant amount of woven bone mixed with the fibrovascular stroma. (b) High-power photomicrograph of the resected nidus from the patient with hematoxylin and eosin staining demonstrates the osteoblastic rimming (solid white arrow in b).
The patient had a moderate resolution of pain after the CT guided biopsy. No further therapeutic procedure was performed.
DISCUSSION
OO was first described by Jaffe in 1955. It was initially considered a form of osteomyelitis by the orthopedic community for many decades. However, presently, it is widely accepted to be a benign bone tumor of unknown etiology. These are commonly seen on the diaphysis and the metaphysis of the long bones, particularly the femur (37.5%), the tibia (20%), and the humerus (3.6%). Their occurrence in the foot is less common with the incidence varying from 1% to 16%. In the foot, the most common site of the involvement is in the talus. The occurrence in metatarsal is very rare (1.5% of all the skeletal tumors involving the foot).
It is a small spherical tumor with a usual diameter of 15 mm or less. It is composed of a nidus which consists of bone at different stages of maturity inside an extremely vascular connective tissue stroma. The core of the nidus shows a variable quantity of mineralization.
CT scan is useful in identifying the central calcified nidus, which may be difficult to identify on either the plain radiograph or MRI.[1] On MRI, the nidus is usually isointense on T1- and T2-WIs.[2] However, MRI is not the imaging modality of choice for this condition. In a scenario, where other imaging modalities are inconclusive; radionuclide imaging is a useful tool for diagnosis.
Technetium 99 metastable-labeled bone scintigraphy is used for the diagnosis of this lesion. The sensitivity of skeletal scintigraphy for the detection of OO reaches close to 100%.[3] The double-density sign is a classical finding with a very high uptake of the tracer in the nidus. The larger area of less intense radiotracer uptake adjacent to the nidus constitutes the host bone tumor reaction.[4] In the case of positive radionuclide imaging, a CT scan is more useful for strengthening the diagnosis than MRI. However, in negative radionuclide imaging, MRI should be done for the diagnosis of other pathologies.[5]
Intra-articular/subchondral OO is a clinically separate entity.[6] This is seen within or near to a joint and most commonly is seen about the hip joint. The knee, ankle, elbow, and wrist are less commonly affected. The clinical features may be puzzling and notable joint tenderness and effusion may contribute to the confusion in diagnosis.[6]
In the present case, an uncommon variant of OO is seen in an uncommon location. MRI showed adjacent bone marrow edema which is variably seen in OO.[7] The post-contrast enhancement of nidus on MRI has been often described in the literature.[8] A review of the literature showed only one reported case of intra-articular OO occurring in the head of the fifth metatarsal, which was managed with curettage and burring.[9]
The differential diagnosis in the present case includes subchondral cyst, juxta-articular erosion associated with gout, and infection. The differentiation with the subchondral cyst is difficult on imaging. However, the age of the patient, the presence of the perilesional bone marrow edema, and the absence of other degenerative changes should point away from this diagnosis. The most common site for erosions in gout is the first MTP joint. A serum uric acid level correlation may be performed in cases with a high index of suspicion for gout. Dual-energy CT is a recent modality which can noninvasively detect urate crystal deposition in gouty arthritis. Clinical presentation and the lack of joint effusion are against the diagnosis of infection.
Treatment of this entity depends on the symptoms of the patient. Pain is the most notable symptom of OO which can be treated with NSAIDs. For a long time, surgical treatment was considered the standard of care. However, today, radiofrequency ablation (RFA) is the modality of choice in many cases. This outpatient procedure is minimally invasive and recovery time is short. Because the nidus of an OO is rich in nerve refibers and usually very tender, the procedure must be performed under general anesthesia.
Specific management considerations about intra-articular OO include a theoretical risk of chondrocyte death due to thermal injury. However, several studies have described similar results with RFA in intra-articular and diaphyseal OOs.[10] The transarticular approach needs to be avoided during RFA. Surgical excision with osteochondral grafting has also be used for the management of these lesions in the larger joints.[10]
CONCLUSION
Even though OOs are common lesions, their presentation has a wide variation in clinical and imaging features. Unwarranted delay in diagnosis and treatment can be averted by consideration of the unusual presentations/locations of common lesions like OO.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am. 1996;27:559-74.
- [Google Scholar]
- Scintigraphic patterns in osteoid osteoma and spondylolysis. Clin Nucl Med. 1987;12:39-44.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoid osteoma. The double density sign. Clin Orthop Relat Res. 1987;222:167-73.
- [CrossRef] [Google Scholar]
- Radionuclide imaging in the diagnosis of osteoid osteoma. Oncol Lett. 2015;10:1131-4.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoid osteoma: An unusual cause of articular pain. Radiology. 1983;147:383-7.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of osteoid osteoma with dynamic gadolinium-enhanced MR imaging. Radiology. 2003;227:691-700.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoid osteoma in atypical locations: The added value of dynamic gadolinium-enhanced MR imaging. Eur J Radiol. 2009;71:527-35.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoid osteoma of the fifth metatarsal: A case report and literature review. J Foot Ankle. 2002;8:71-8.
- [CrossRef] [Google Scholar]
- Intra-articular osteoid osteoma of the distal femur treated with osteochondral grafting: A report of 2 cases. JBJS Case Connect. 2019;9:e0211.
- [CrossRef] [PubMed] [Google Scholar]






