Translate this page into:
An unusual cause of intramedullary bone cysts – Congenital afibrinogenemia

*Corresponding author: Dr. Raghu Teja Sadineni, Department of Diagnostic and Interventional Radiology, Pramodini Imaging and Diagnostics, Vijayawada, Andhra Pradesh, India. sadineniraghu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sadineni RT, Padavala S, Chalasani K, Boppana D. An unusual cause of intramedullary bone cysts – Congenital afibrinogenemia. Indian J Musculoskelet Radiol. 2024;6:132-5. doi: 10.25259/IJMSR_46_2024
Abstract
Solitary bone cysts have a wide range of differentials, but when there are numerous bone cysts involving multiple bone sites, a systemic hematological disorder would be the leading differential. We intend to highlight the multimodality imaging findings of multiple intramedullary bone cysts occurring as a rare complication of congenital afibrinogenemia. Intraosseous hemorrhages occur due to altered clotting mechanisms which later lead to formation of cysts.
Keywords
Intraosseous hemorrhages
Multiple lytic lesions
Multiple bone cysts
Hematological disorder
Clotting disorder
INTRODUCTION
Bone cysts are benign cavities which are filled with fluid and appear as lytic lesions on radiographs. Magnetic resonance imaging (MRI) may be performed to detect the fluid nature and rule out any associated solid components. They are of several unrelated types and few of them include unicameral cysts, aneurysmal bone cysts, subchondral cysts, and cystic like tumors. These types of cysts are usually solitary or discrete. The presence of multiple or confluent bone cysts within the medulla is quite unusual. Congenital afibrinogenemia is one such rare disorder where there is alteration in coagulation, leading to abnormal bleeding within multiple bones. We intend to describe the findings in a child with congenital afibrinogenemia, only child born of a consanguineous marriage showing intraosseous hemorrhages in multiple bones leading to the formation of confluent intramedullary bone cysts.
CASE REPORT
An 8-year-old boy with known congenital afibrinogenemia presented with recurrent bone pains, especially in both lower limbs from the past 2 months. His past history revealed apparently easy bruising. Laboratory work up showed significantly prolonged prothrombin time, prolonged activated partial thromboplastin time and non-detectable fibrinogen.
Initial radiographic evaluation of both lower limbs including thighs and legs was performed.
They revealed multiple lytic lesions involving the entire medullary regions of both femurs and tibia. Few internal thin-walled confluent lytic areas were noted. Epi-metaphyseal regions appeared uninvolved [Figure 1].

- Frontal plain radiographs of both (a) thighs and (b) legs showing near diffuse radioluceny with multiple lytic lesions in medullary cavities of both femurs (white arrows) and tibia (yellow arrows) with multicystic appearance and intact but thinned cortex. Areas of endosteal scalloping are noted within the bones, suggesting a long-standing process. No internal areas of matrix mineralization. Soft tissues appear to be normal.
For further assessment of the lesions, MRI of both lower limbs was performed. MRI revealed multiple contiguous long segmental cystic lesions involving near total medullary cavities of diaphysis of femurs and tibia in both lower limbs. These showed hyperintensity on fluid sensitive images with internal areas of fluid-fluid levels. T1-weighted images showed associated hyperintensities within the cysts suggesting internal hemorrhages and blood-fluid levels consistent with intraosseous hemorrhages of varying stages [Figure 2a-d]. Small intraosseous cysts are also noted involving bilateral calcaneal bones and right second metatarsal bone. No obvious associated pathological fractures were noted. Features were suggestive of intraosseous cysts and intraosseous hemorrhagic complications of afibrinogenemia.
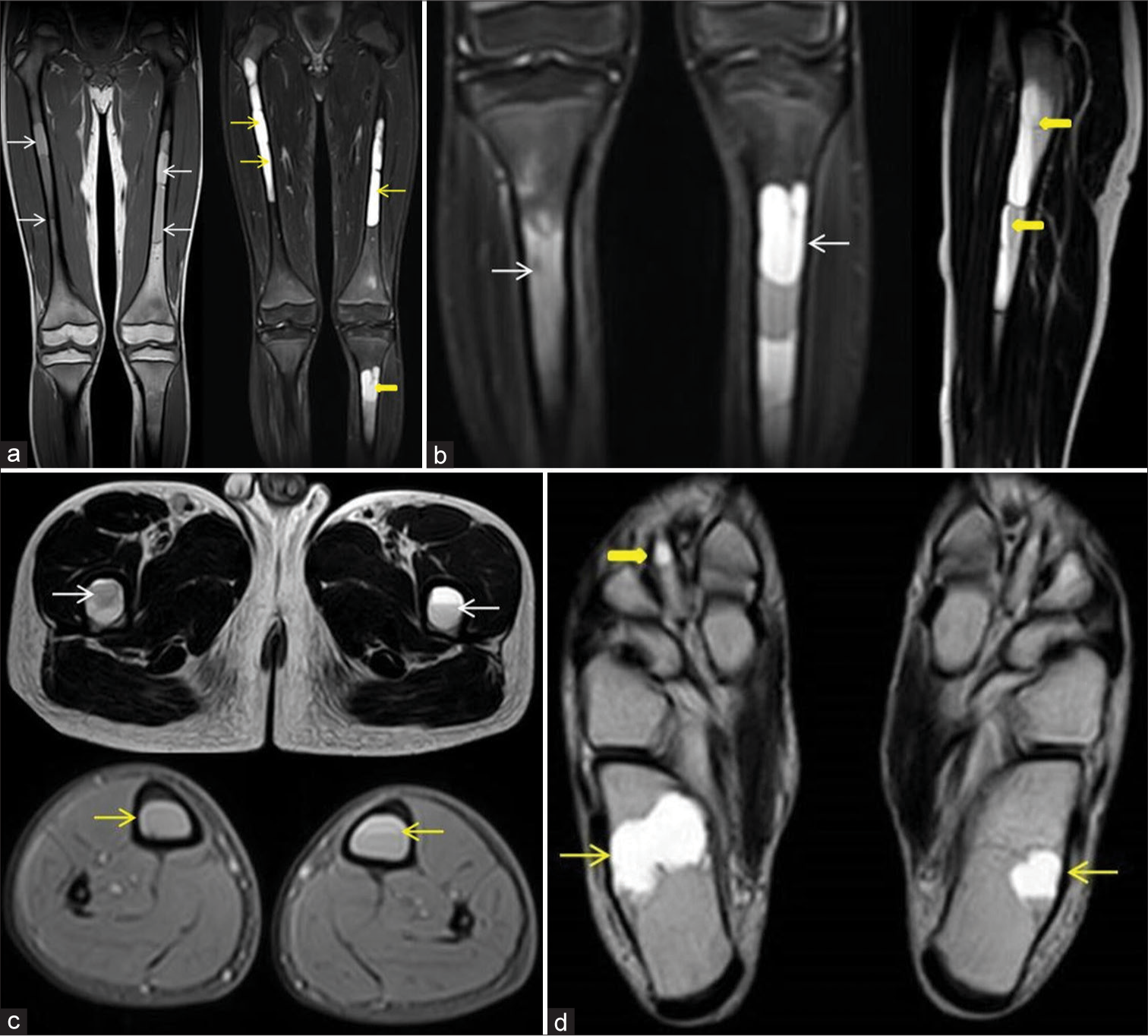
- (a) Long field of view T1-weighted spin-echo (SE) coronal and fluid sensitive fat saturated (STIR) coronal magnetic resonance (MR) images show long segmental near confluent cystic lesions involving near total medullary cavities of both femurs (white and yellow arrows) and tibia (thick yellow arrow) showing bright hyperintense signals on STIR images (thin yellow arrows) and few associated T1 hyperintensities (white arrows) suggesting internal hemorrhages. (b): Coronal fluid STIR MR image of both tibia (white arrows) and T2-weighted (T2W) SE sagittal MR image of left femur demonstrate internal fluid- fluid levels (thick yellow arrows). (c) Axial T2W SE and T2W gradient echo MR images of both thighs and legs demonstrating the internal fluid-fluid/blood fluid levels within the cysts at both femurs (white arrows) and tibia (yellow arrows). (d) Axial T2W SE MR image of both feet shows small intraosseous cysts involving bilateral calcaneal bones (thin yellow arrows) and right 2nd metatarsal bone (thick yellow arrow).
DISCUSSION
Congenital afibrinogenemia is an autosomal recessive disease due to mutation in one of the fibrinogen genes (fibrinogen alpha, fibrinogen beta or four core genotypes).[1] There is absence or reduction of fibrinogen detected by antigenic and functional assays (usually <0.1 g/L). Fibrinogen is a plasma glycoprotein secreted by the liver and is essential for the coagulation pathway.
Most of the cases reported are from consanguineous marriage. Fibrinogen-related disorders may lead to excessive bleeding or abnormal thrombosis. Moderate-to-severe bleeding may occur; however, this is less than that seen in severe hemophilia. They present clinically due to spontaneous or post-traumatic bleedings at mucocutaneous regions, soft-tissues, joints, solid abdominal visceral organs, or genitourinary regions.
Imaging findings in these patients are related to the hemorrhages. There might be extradural or intracerebral hemorrhages, bleeding within the joints leading to hemarthrosis, muscle hematomas, and intraosseous hemorrhages. Arterial and venous thrombosis with morbidity in the pregnancy may be seen. Few cases of spontaneous splenic ruptures have also been reported.[2]
Cystic lesions of the bone are benign findings noted in few cases. They appear within the medulla in diaphysis of long bones, more often in femur, tibia, and humerus. Intraosseous hemorrhages usually occur at the site of entrance of nutrient artery which leads to destruction and reconstruction of bone with formation of cysts and adjacent fibrous reaction. Histologically, these lesions usually contain old blood clots with necrotic tissue and surrounding non-specific fibrotic tissue.[3] Large cysts may cause weakening of the bone and result in pathological fractures.[4] Whole-body screening with magnetic resonance may be performed in these individuals to evaluate the extent and multiplicity of bony involvement.
Management options include transfusions, cryoprecipitate, and fresh frozen plasma, but fibrinogen concentrate infusions are the mainstay of treatment. Prophylactic measures including limited weight-bearing and reduced sporting activities may be required to prevent pathological fractures. The bone lesions may sometimes require repeated packing surgeries and selective vascular embolization in episodes of acute severe hemorrhages.
Differential diagnosis
If radiographs of a single bone are performed, they may resemble cystic fibrous dysplasia, enchondroma, or Langerhans cell histiocytosis. MRI clearly depicts the absence of bone marrow or soft-tissue edema, confirms the fluid nature of the lesion, and further characterizes the cysts with fluid levels. Unicameral bone cysts are located at meta-diaphyseal regions and easily excluded from the differentials. Multiplicity of the lesions and occurrence in multiple bones provides the clue.
Multiple confluent bone cysts may also be seen in metabolic disorders like Wilsons disease where multiple confluent multiseptated intramedullary cysts are seen; however, additional involvement of other organs such as brain, liver, and joints suggests the diagnosis.
Similar fewer lesions may also be seen in congenital alpha 2-plasmin inhibitor deficiency, which is also a coagulation pathway disorder and can be diagnosed confidently with serology. Clinical examination to look for easy bruising and a past history of bleeding episodes at different sites helps in making a diagnosis of disorders of coagulation pathways.
Teaching points
The presence of multiple bone cysts involving many bones should prompt for a search to underlying hematological disorders.
Disorders with altered coagulation mechanisms lead to hemorrhages at multiple sites and even the bones are not exempt.
Intraosseous hemorrhages with time lead to the formation of confluent intramedullary cysts.
CONCLUSION
The presence of confluent intramedullary lytic lesions on radiographs and multiple cystic like areas on MR imaging involving multiple bones should prompt the search for an underlying hematological disorder. Intraosseous hemorrhages with confluent intramedullary cysts may be observed as a rare complication in congenital afibrinogenemia.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Congenital afibrinogenemia: A case report. Arch Pediatr. 2015;22:50-2.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous splenic rupture in a patient with congenital afibrinogenemia. Turk Arch Pediatr. 2014;49:247-9.
- [CrossRef] [PubMed] [Google Scholar]
- A case of intramedullary haematoma associated with congenital alpha2-plasmin inhibitor deficiency. Pediatr Radiol. 1998;28:978-80.
- [CrossRef] [PubMed] [Google Scholar]
- A rare complication of congenital afibrinogenemia: Bone cysts. Turk J Hematol. 2017;34:183.
- [CrossRef] [PubMed] [Google Scholar]






