Translate this page into:
Fatty disc: An unusual pattern of disc degeneration

*Corresponding author: Vikas Bhatia, Department of Radiodiagnosis and Imaging, Post Graduate Institute of Medical Education and Research, Chandigarh, India. drvikasbhatia@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhary N, Singh P, Bhatia V, Prakash M. Fatty disc: An unusual pattern of disc degeneration. Indian J Musculoskelet Radiol 2022;4:46-8.
Abstract
The intervertebral disc is the fibrocartilaginous structure between the endplates of adjacent vertebral bodies, providing support and mobility to the spine. Normally, the disc is isointense on the T1 weighted image (T1WI) and hyperintense on the T2 weighted image (T2WI). Degenerating disc shows loss of hyperintensity on T2WI due to disc dehydration. The development of hyperintensity on T1WI in degenerating disc is unusual. Causes of discal hyperintensity on T1WI include calcification, hemorrhage, melanin, mucin, or fat within the disc. Fat contents in the disc may be rarely seen in degeneration and appear as hyperintense signal on T1WI and T2WI. We, hereby report a case of discal hyperintensity on T1WI and T2WI due to fatty degeneration of the disc.
Keywords
Spine
Fatty degeneration
Magnetic resonance imaging
INTRODUCTION
Degenerative diseases of the spine is a major cause of morbidity with a prevalence of up to 27.3 ± 1.7%.[1] Imaging in degenerative disease of the spine is aimed at knowing the extent of degeneration and associated neural compressions which dictate further management protocol. Degeneration causes signal alterations in the disc and marrow. The disc gradually loses its water content which is seen as a loss of hyperintensity on T2 weighted image (T2WI). The presence of calcification, blood products, mucin, melanin, and fat within the disc can cause hyperintensity on T1 weighted image (T1WI) [Table 1]. The presence of fat within the disc is very rare and only a few case reports have been published so far in the literature. Fat within the disc may be seen either due to macroscopic fat or due to the presence of fatty marrow in progressive calcification of disc forming bony tissue. Hereby, we report a rare case of fatty degeneration of the disc.
| Calcification- degeneration, ankylosing spondylitis, ochronosis, pseudogout, hemochromatosis, and post-operative / post-traumatic sequel |
| Hemorrhage |
| Melanin |
|
Fat 1.Fatty degeneration 2. Marrow fat of ossified disc (advanced stage of degeneration, post-traumatic or post-operative sequel, ochronosis, ankylosing spondylitis, hyperparathyroidism, acromegaly, and amyloidosis, etc.) |
|
Mucin (T1WI : T1 weighted image) |
CASE REPORT
A 35-year-old female presented with neck stiffness and decreased range of motion for 6 months. There was no history of trauma, fever, or any other systemic illness. Magnetic resonance imaging evaluation of the cervical spine showed early degenerative changes in the form of multilevel discal hypointensity on T2WI suggesting disc dehydration. The posterior part of the C4-C5 intervertebral disc showed hyperintensity on T2WI and T1WI [Figure 1a and 1b]. Suppression of T1 hyperintense signal was seen on non-contrast fat-suppressed T1WI, suggesting fat content [Figure 1c]. A suspicious fissure was also seen in the right posterolateral aspect of the annulus fibrosus [Figure 2]. Overall features were suggestive of fatty degeneration of the intervertebral disc. The patient was managed conservatively with analgesia and physiotherapy and symptoms resolved within 1 month.
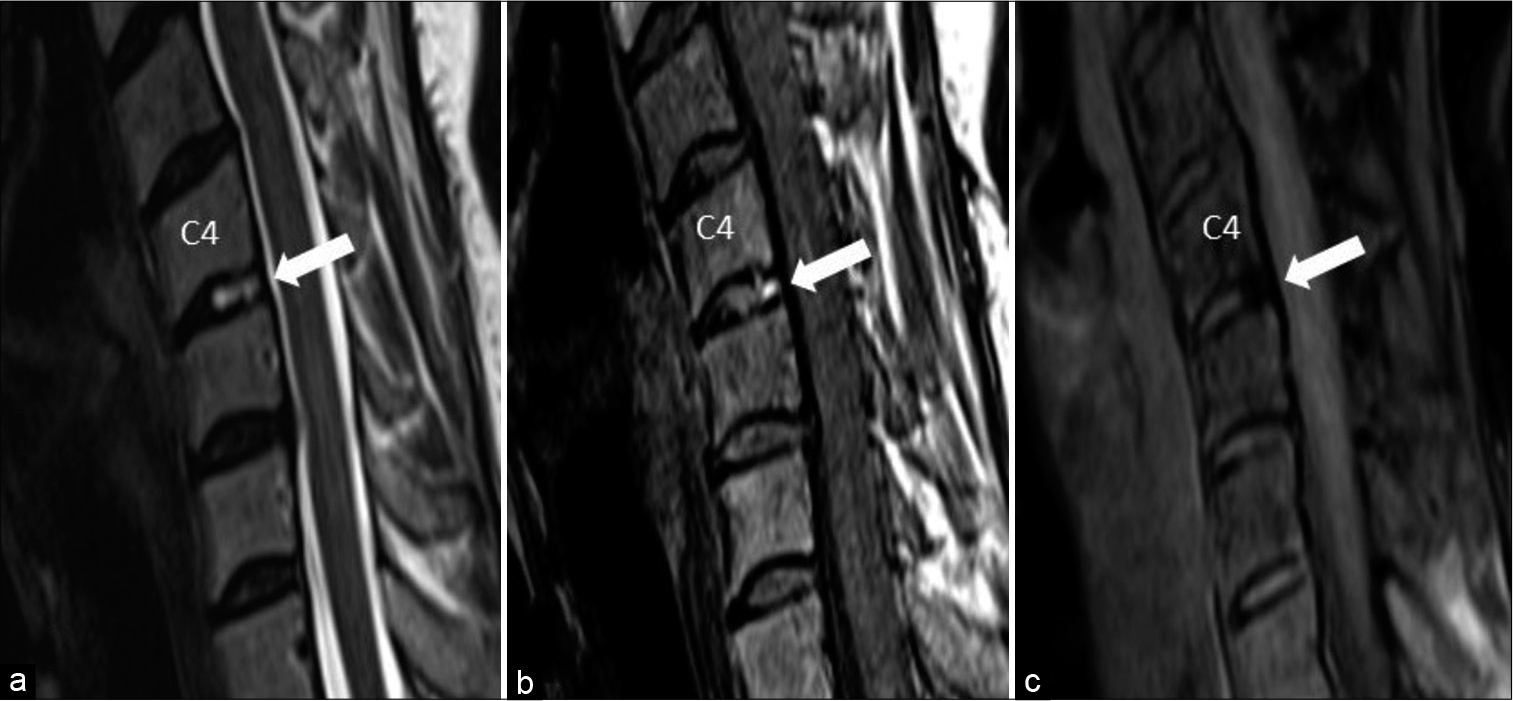
- Hyperintensity is seen in the posterior part of C4-C5 intervertebral disc on sagittal T2 weighted image (a) and T1 weighted image (b). Suppression of T1 hyperintensity is seen on fat suppressed T1WI (c).
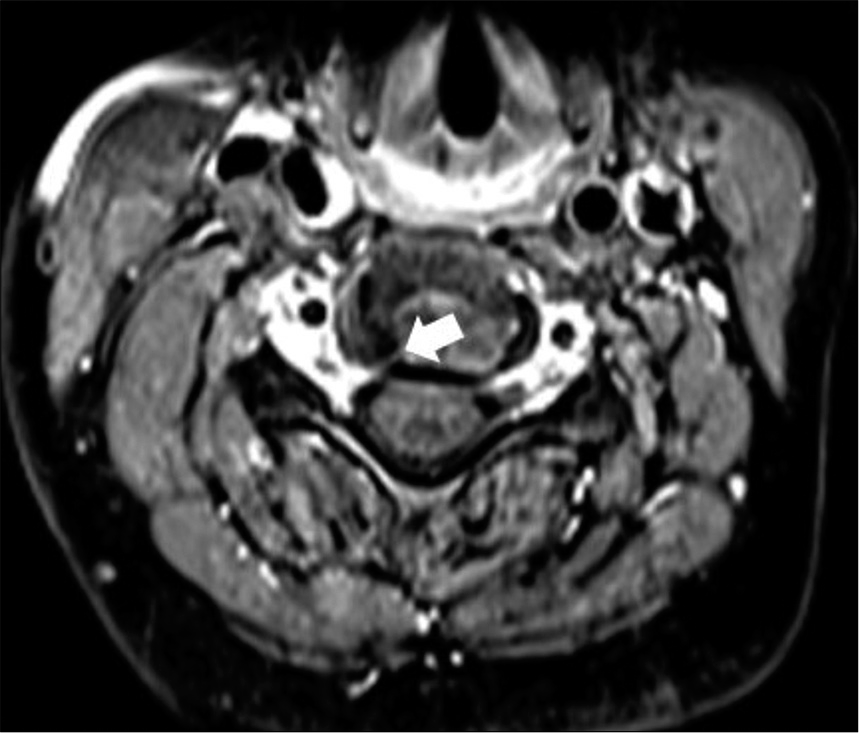
- Post contrast T1 axial image at C4-C5 level shows a suspicious fissure in right posterolateral aspect of annulus fibrosus (arrow) which may represent possible path of migration of nerve root sleeve fat.
DISCUSSION
The fibrocartilaginous intervertebral disc has three components, outer annulus fibrosus, inner annulus fibrosus, and central nucleus pulposus.[2] The outer annulus fibrosus is composed of dense collagenous fibers. The inner annulus fibrosus is less compact and contains collagen fibers and collagenous matrix. The cartilaginous central nucleus pulposus is semisolid or gel-like in consistency and contains glycosaminoglycans. It appears hyperintense on T2WI due to its predominant water content. In disc degeneration, water content gradually diminishes and it becomes hypointense on T2WI. On T1 weighted image, the normal disc is hypointense as compared to the marrow. However, in cases of marrow infiltration (e.g. multiple myeloma, myelofibrosis, hematopoiesis, metastasis, etc.), reversal of the signal occurs, and the disc becomes more hyperintense than marrow. This is termed as “disc reversal sign.”[3] Causes of intrinsic discal hyperintensity on T1WI are the presence of blood, melanin, mucin, fat, or calcification.[2] [Table 1] Discal calcification may appear hyperintense on T1WI due to unmineralized calcium within and can be seen in cases of disc degeneration, ankylosing spondylitis, ochronosis, pseudogout, hemochromatosis, and post-operative / post-traumatic spine.[4] Discal hyperintensity on T1WI and T2WI due to presence of fat within, is an unusual phenomenon. Very few case reports have been published so far.[5,6] One hypothesis is the presence of fissures in the annulus fibrosus formed secondary to trauma or degeneration which may lead to migration of epidural fat into the disc. This theory may be true in the lumbar spine where ventral epidural fat is present.[7] However, epidural fat is absent in the cervical spine. Nonetheless, fat is known to be present around the nerve root sleeve.[7] And, migration of this perineural fat may explain its presence in the cervical intervertebral disc. Another mechanism may be secondary to metaplastic changes in the disc. Further studies are warranted to prove these hypotheses. Fat may also be seen in discal ossification containing fatty marrow within.[5] Causes of discal ossification include advanced stages of degeneration, post-traumatic or post-operative sequel, ochronosis, ankylosing spondylitis, hyperparathyroidism, acromegaly, and amyloidosis, etc.[4] A radiograph or computed tomography (CT) scan can help to differentiate fatty marrow from the fatty degeneration of disc, as hyperdensity will be seen in cases of discal ossification, while fatty degeneration will show fat attenuation on CT and radiolucency on the radiograph. T1 fat-suppressed imaging should be done in cases of discal hyperintensity on T1WI to confirm the presence of fat and to differentiate it from other causes of T1 hyperintensity such as hemorrhage, melanin, calcification, or mucin. Fatty degeneration of the disc is likely a “no-touch benign lesion” and can be followed up with imaging.
CONCLUSION
Fatty change in the intervertebral disc is a rare pattern of disc degeneration. Inclusion of T1 fat-suppressed sequences in the suspected cases can diagnose fatty change in disc and will help to rule out other causes of discal hyperintensity on T1WI.
Declaration of patient consent
Patient consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence of spine degeneration diagnosis by type, age, gender, and obesity using Medicare data. Sci Rep. 2021;11:5389.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging intervertebral disc degeneration. J Bone Joint Surg Am. 2006;88:15-20.
- [CrossRef] [PubMed] [Google Scholar]
- The bright intervertebral disk: An indirect sign of abnormal spinal bone marrow on T1-weighted MR images. AJNR Am J Neuroradiol. 1990;11:23-6.
- [Google Scholar]
- Hyperintense disks on T1-weighted MR images: Are they important? Radiology. 1995;195:325-6.
- [CrossRef] [PubMed] [Google Scholar]
- High signal intensity of intervertebral calcified disks on T1-weighted MR images resulting from fat content. Skeletal Radiol. 2005;34:80-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical implications of epidural fat in the spinal canal. A scanning electron microscopic study. Acta Anaesthesiol Belg. 2009;60:7-17.
- [Google Scholar]







